46234
0
In this article:
- Why get tested?
- Indications
- Preparing for a stool test for carbohydrates
- Decoding
- Deviations from the norm
- Useful video about lactase deficiency
Digestive problems are common in young children. To find out their origin and select treatment tactics, doctors prescribe various diagnostic tests. Feces for carbohydrates in an infant are examined if the child is suspected of having lactase deficiency.
The study allows us to accurately determine the causes of disruption of the digestive tract in infants, namely, to assess the process of breakdown and absorption of carbohydrates.
As a rule, this analysis is carried out in the first year of a child’s life, since in most cases the signs of lactase deficiency disappear over time, and the baby’s digestion returns to normal.
Data
A very interesting spread of lactose intolerance syndrome.
- Globally, 75% of the adult population cannot tolerate milk sugar, and with it dairy products;
- lactase deficiency is common among the indigenous populations of South America and Asia (up to 90% of Latin Americans);
- 75% of African Americans have this syndrome;
- on average, 25% of European adults have lactose intolerance (lactase deficiency) as adults;
- while, for example, in the Netherlands and Sweden, they do not know about this problem at all;
- Russia's share went to approximately 50%;
- men and women are affected equally often. The syndrome begins to manifest itself at the age of 20;
- 44% of pregnant women who were previously milk intolerant regain the ability to digest lactose during pregnancy;
- Lactose intolerance can be easily treated by eliminating milk from the diet;
- no one died from primary lactose intolerance;
- A complication of lactose intolerance can be osteopenia, which in old age can develop into osteoporosis.
Causes of lactose intolerance in children
Reduced lactase activity is observed in 2/3 of children born. In most cases this does not lead to illness. By 2-3 months of life, the enzyme begins to work at full strength.
In full-term children under one year of age, in the majority of cases, lactose intolerance is caused by overfeeding, intestinal immaturity and (or) its pathologies. In premature babies, low lactase activity is detected in almost everyone. Most often, it is in these cases that the doctor recommends a stool test for carbohydrates.
Lactose intolerance due to overfeeding is explained by excess milk sugar in the child's intestines. Although the amount and activity of the enzyme are normal, they are not enough to break down the carbohydrate supplied with excess milk. Undigested lactose is transported in large quantities into the large intestine, leading to diarrhea and other characteristic symptoms.
Most often, this condition is observed when feeding “on demand”. Lactose overload is of particular importance in the development of symptoms in infants born prematurely or exposed to hypoxia during labor. Dr. Komarovsky considers overfeeding to be the main reason for diagnosing lactose intolerance and ordering a stool test for carbohydrate content.
In children born at 28-30 weeks of pregnancy, the small intestine has not matured morphologically and functionally. Gradually, the intestine matures and enzyme activity returns to normal.
Acquired (secondary) lactose intolerance is quite common. Its causes are most often acute intestinal infections: rotavirus, salmonellosis, or the use of antibiotics and other drugs (anabolic steroids).
What are disaccharides in a child’s stool?
Synonyms: carbohydrate content in feces, reducing substances in feces;
Stool sugars; Reducing substances, fecal. Carbohydrates are one of the most important food components and the main suppliers of energy for the body. In products they are contained in the form of complex saccharides, which, after breakdown, are absorbed in the small intestine.
If the process of assimilation of carbohydrates is disrupted - malabsorption, provoked by congenital or acquired enzymatic deficiency, as well as certain diseases of the small intestine, a deterioration in the general state of human health is observed.
Carbohydrate deficiency is considered a fairly common pathological condition today. In addition, experts suggest that carbohydrate deficiency may be the cause of diseases that do not have a clear etiological picture (migraine, depression, etc.).
Analysis of stool for carbohydrate content makes it possible to timely diagnose such disorders and prescribe effective therapy to relieve the patient of unpleasant symptoms.
General information
Impaired absorption of carbohydrates in the small intestine - malabsorption - is a sign of enzymatic deficiency, which can be either hereditary or acquired.
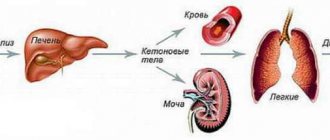
The most common type of malabsorption is lactase deficiency - lactose intolerance, i.e. the body's inability to break down and absorb milk sugar.
Congenital lactase deficiency manifests itself already in the first months of a child’s life and is characterized by a sharp delay in weight gain. In adulthood, the acquired form is most often diagnosed.
Less commonly observed is a malabsorption of sorbitol alcohol, fructose, trehalose, and sucrase-isomaltase.
Regardless of the type of enzymatic deficiency, the accumulation of large amounts of undigested carbohydrates in the intestines manifests itself in the same way:
- spasmodic pain (colic) in the abdomen, provoked by impaired intestinal motility;
- increased gas formation due to increased fermentation of bacterial microflora;
- diarrhea, the cause of which is the retention of a large amount of fluid in the lumen of the intestinal tube (osmotic effect);
- signs of intoxication of the body: headaches and dizziness;
- general weakness and lethargy;
- nausea and vomiting;
Malabsorption may also be temporary. Often this condition develops after an intestinal infection or an acute inflammatory process, serious operations on the gastrointestinal tract, etc. An ill-designed diet can also affect the speed and extent of carbohydrate absorption. For example, increased sorbitol content in familiar foods can impair the absorption of fructose.
Indications for analysis
The analysis is interpreted by a gastroenterologist, therapist, pediatrician or general practitioner.
- Chronic diarrhea and digestive disorders in adults;
- Headaches, apathy and weakness, lack of body weight,
- Stomach disorders without established causes;
- Previously identified malabsorption in adults;
- Diagnosis of congenital lactase deficiency in infants under one year of age;
- Lack of required weight gain in newborns.
An analysis of carbohydrate content in feces is a fairly informative diagnostic test. However, based on its results, only the total (total) amount of all carbohydrates can be assessed. It is not possible to calculate the concentrations of lactose, fructose, glucose and other sugars separately.
Norm of carbohydrates in feces
| Patient age | Amount of carbohydrates |
| Children under 1 year | 0 – 0,25% |
| Children over 1 year old and adults | Not detected |
Note: in children of the first year of life the following deviations from the norm may be observed:
- 0.3 – 0.5% (insignificant);
- 0.6 – 1% (average);
- more than 1% (significant).
Factors influencing the result:
- Violation of the rules for preparing for analysis;
- Errors when collecting biomaterial;
- Features of the daily diet;
- Patient's age;
- Genetic factors and family history;
- Intestinal infection or inflammation;
- Taking prebiotics, antibiotics and other drugs.
Carbohydrates in feces are increased
- Enzyme (lactase) deficiency;
- Chronic diseases of the small intestine: Crohn's disease (granulomatous inflammation of the gastrointestinal tract);
- celiac disease (impaired breakdown of gluten), etc.;
;
Preparing for analysis
To obtain reliable research results, the following preparation rules must be observed:
- 3 days before the analysis, exclude the use of rectal suppositories and cleansing enemas;
- a week before the procedure, stop taking medications: those that affect the character of stool (antidiarrheals, laxatives);
- increasing peristalsis (pilocarpine, belladonna);
- containing coloring pigments (barium, bismuth, iron, etc.);
- exclude colored (red and green) vegetables/fruits, juices from them, ketchup and tomato paste, alcohol from the diet;
A mandatory condition is not to undergo diagnostic tests with contrast (X-ray, CT, MRI, etc.) 2-3 days before the analysis.
Source: https://kishechnik-zhivot.ru/voprosy/disaharidy-v-kale-u-rebenka-chto-eto
Types of lactase deficiency
In clinical practice, there are three main types of pathology:
- Congenital lactose intolerance is inherited as an autosomal recessive trait and is very rare. Appears from birth;
- primary lactose intolerance (lactase deficiency);
- secondary lactose intolerance (lactase deficiency)
Primary lactose intolerance is associated with low levels of the enzyme lactase; the decrease in enzyme production occurs gradually and this form develops after childhood. Occurs only in adults. A type of syndrome characterized by insufficient lactase production in the absence of any damage to enterocytes.
If we return again to the question of nationality, tests for residents of northern Europe show high lactase activity at any age. But among Asians it begins to decline quite early.
Secondary lactose intolerance (lactase deficiency).
This type of syndrome occurs in adults and children. Lactase deficiency develops due to damage to small intestinal cells. Secondary, or acquired, lactase deficiency can develop in a person with a healthy small intestine during episodes of acute illness. This occurs due to damage to the mucous membrane or from drugs. Some causes of secondary lactase deficiency:
- acute gastroenteritis;
- giardiasis;
- ascariasis;
- Crohn's disease;
- celiac disease;
- tropical sprue, gastrinoma;
- radiation enteritis, for example during irradiation of cancer patients;
- diabetic gastropathy;
- carcinoid syndrome;
- Whipple syndrome;
- HIV enteropathy;
- kwashiorkor;
- chemotherapy;
- pancreatic adenoma, which provokes the development of ulcers;
- after a long period of forced feeding through intravenous drips.
We have dealt with primary enzyme deficiency - it poses no threat to adults. With secondary lactase deficiency everything is almost the same.
DO NOT DRINK MILK and there will be no problems. Milk is not a food for adults – period!
All the horror stories are like: dehydration, since prolonged diarrhea removes a huge amount of fluid, which is quite difficult to replenish;
deficiency of calcium and many other microelements, since the absorption of these substances practically stops in the intestines; the lack of nutrients coming from dairy products leads to a halt in the development of beneficial microflora bacteria; the population of putrefactive bacteria grows; Peristalsis decreases significantly; the overall immunity of the body decreases - this applies ONLY to children. They have nothing to do with the adult body! In adults, symptoms of primary lactose intolerance, lactase deficiency are the norm, not a disease, and international recommendations from nutritionists and gastroenterologists suggest the following as the first diagnostic test:
- exclude milk;
- if milk is excluded and things get better, then no in-depth “diagnosis” is needed! Unless you want to support a medical laboratory with your finances
In some doubtful cases, the same “international standards” recommend a couple more tests:
- blood test for lactose load. The patient drinks 50 ml of lactose and then the blood sugar level is measured, recording the data on a graph and plotting a curve. Lack of lactase makes the curve straightened; the graph does not show an increase in glucose after 60 and 120 minutes, since its absorption does not occur in the intestine.
- Milk load test gives 500 ml of milk and measures blood sugar levels. If the blood sugar level is less than 9 mg/dl, then this confirms the malabsorption of glucose in the intestine.
All other tests may be needed only for differential diagnosis with other more serious disorders, to study secondary lactose intolerance, for example, with celiac disease.
- Stool analysis. This test shows the amount of carbohydrates and the pH level. A healthy person does not have carbohydrates in their stool. In case of lactase deficiency syndrome, their presence is determined, and the pH drops to a level of 5.5 and below.
- analysis of the concentration of exhaled hydrogen. The same is done with a lactose load. Samples are made every half hour up to six times.
- biopsy and enzyme activity analysis. To carry it out, a wash is taken from the mucous membrane. The result of this test is considered to be as reliable as possible. (in practice this is not used, since it is an invasive method and has complications).
- Genetic testing is sometimes done to find out the cause of secondary lactose intolerance, such as in the case of celiac disease.
In addition to specific tests in adults, other diseases are excluded, the symptoms of which may be diarrhea and bloating. Only after receiving all the answers to the tests, a therapeutic diet menu is developed together with a nutritionist. Enzymes are prescribed and measures are taken to relieve symptoms.
research. The main syndromes of damage to the hematopoietic organs and the composition of peripheral blood. Variants of hemorrhagic syndromes, types of bleeding. HERE, INTERNET, CHAPTER 2 OF THE TEXTBOOK
1) vascular link - reduced vascular resistance
2) plasma link - activity of factors 2, 7, 9, 10, 11 and 12 is reduced
3) the platelet link is functionally reduced. Newborns - 100 - 300x10/l, up to 1 year - 150 - 300x10/l, over one year - 200 - 400x10/l.
anticoagulant system: a lot of heparin, low activity of tissue and plasma antithromboplastins, antithrombin 3, antiactivators 11 and 10 factors. increased fibrinolytic blood activity. little plasminogen. Duration of bleeding: 2-4 minutes. Coagulation time: 30-2, up to 5 minutes. Increases with inherited coagulopathy, liver disease, fibrinogen deficiency, use of drugs, disseminated intravascular coagulation syndrome stages 2 and 3. Shorten for bleeding and stage 1 DIC.
48.AFO of the heart and blood vessels in children and adolescents, connection with pathology. Features of the heart shape in young children and adolescents. Age-related changes in the projection of the heart to the anterior surface of the chest, the ratio of the diameter of the heart and the diameter of the chest. Age-related features of blood supply to the myocardium. Nervous regulation of blood circulation, features of the cardiac conduction system in children. INTERNET
49.Blood circulation in the fetus. The mechanism and timing of closure of the embryonic circulatory pathways (Arantian duct, foramen ovale, ductus botallus) after the birth of a child and the establishment of the pulmonary (lesser) circulation. HERE
— the presence of placental circulation;
— the functioning of fetal communications (shunts): foramen ovale, arterial (Botallov) and venous (Arantius) ducts;
- minimal blood flow through the lungs (6-9% of cardiac output).
The first inhalation and straightening of the alveoli cause a significant decrease in resistance in the pulmonary vessels, which leads to an increase in blood flow in the pulmonary circle by 5 or more times. Before birth, systolic pressure in the pulmonary artery is higher than in the aorta. From the moment of birth, there is a drop in pressure in the pulmonary artery.
As a result, blood flows from the aorta to the pulmonary artery through the patent ductus arteriosus (a reversal of the shunt from the one in the fetus). Functional closure of the ductus arteriosus begins 10–15 minutes after birth, while anatomical closure occurs in 35% of children by 2 weeks, in 80% by 8 weeks of life.
50.Healthy child. Basic concepts: healthy child – borderline health conditions – disease. The connection between child health and development. The role of hereditary-genetic factors, environmental conditions, nutrition, education, disease prevention for the proper development of the child. Methodological approaches to assessing children's health. The concept of health groups. Algorithm for determining the health group of children. HERE, INTERNET
. healthy children who do not have risk factors for any particular pathology;
. children at risk of developing chronic pathology and prone to increased morbidity, with functional abnormalities, and who are often ill;
. children with chronic pathology in the compensation stage;
V. children with chronic pathology in the subcompensation stage;
V. children with chronic pathology in the stage of decompensation.
a) in prenatal – occupational hazards, bad habits and alcoholism of parents; chronic extragenital diseases of the mother, a burdened obstetric history, the mother's age at the time of birth is younger than 18 years and older than 35 years, the pathology of the current pregnancy (threat of miscarriage, bleeding, toxicosis, infections); violations of the regime and nutrition during pregnancy;
b) deviations in the intranatal period - protracted, rapid, rapid labor; early rupture of amniotic fluid, long anhydrous interval; surgical interventions, pathology of the placenta and umbilical cord; large fetus, abnormal fetal position;
c) children with a burdened genealogical history, in whose pedigree hereditary diseases or diseases with a certain metabolic orientation are noted: allergies, metabolic nephropathy, endocrinopathies, gastroenterological diseases, lesions of the cardiovascular, skeletal systems, nervous and mental diseases, oncological pathology, immunodeficiency states and etc.
. B. “high-risk” group - children who suffered any disease (condition) in utero, during childbirth, or in the first hours of life and who have various health conditions after discharge from the hospital. These are premature children, immature, post-term, with congenital malnutrition, from multiple pregnancy, with intrauterine infection, after severe asphyxia, with post-hypoxic encephalopathy, birth trauma, hemolytic disease of the newborn, who have suffered lung diseases, infections and other pathologies.
Fecal analysis for carbohydrates in infants
The analysis of stool for carbohydrates in infants is directly related to lactose intolerance (lactase deficiency). In the first year of a child's life, the digestive system is not fully formed.
Hence the emergence of problems with the absorption of mother's milk or an adapted formula.
What are the symptoms for which a coprogram is indicated? How to correctly collect material for analyzing feces for carbohydrates and decipher the results?
Indications for stool analysis in infants
The intestines of an infant are immature and are sometimes unable to cope with the required digestive processes.
A full study of feces is carried out by a coprogram, which helps to assess the functioning of the gastrointestinal tract and other organs involved in digestion - the liver, gall bladder.
During the analysis of stool, among other things, the content of carbohydrates in it is necessarily revealed.
For a growing baby, lactase deficiency (lactose intolerance) becomes a serious problem.
A stool test for carbohydrates is indicated if there is a suspicion of inadequate absorption of mother's milk or formula. Lactase is involved in the breakdown of lactose. Enzymes are closely interrelated.
If there is insufficient production of the digestive enzyme in the child's body, milk is not completely absorbed, which causes lactose intolerance.
The following symptoms indicate lactose deficiency in an infant:
- sharp sour smell from feces;
- loose stools, sometimes foam is observed;
- increased gas formation, bloating;
- the presence of frequent bowel movements (the child goes to the toilet up to 10 times a day);
- poor weight gain by the baby, even a decrease in body weight may be observed;
- crying, capriciousness of the child during feeding or immediately after;
- Instead of diarrhea, the child may suffer from constipation.
Sometimes you can see undigested food, lumps of mucus, and greenish foam in the stool. Regurgitation and even vomiting are possible. The process of digesting milk (formula) becomes uncomfortable for the child.
Even when feeling hungry, the baby takes the breast and, not having eaten, throws it away. Feedings are delayed. A small amount of milk causes the baby's stomach to growl and swell.
Allergic reactions occur, and the skin may break out in a rash.
Violation of the intestinal absorption of nutrients leads to a lack of iron in the body. The level of hemoglobin in the blood drops. Externally, this is expressed in the blanching of the skin and mucous membranes.
Breast milk is the main source of nutrients. From it the child receives proteins, calcium, glucose, vitamins, macro- and microelements necessary for life and growth.
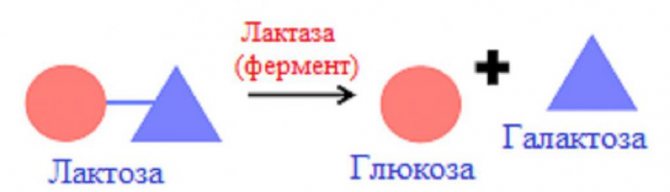
Lack of lactase provokes the inability of the intestines to fully absorb and accept the necessary nutrition. When lactose is broken down, galactose and glucose are produced.
The latter is the main source of energy for humans.
Galactose is necessary for the full development of the central nervous system. The danger of insufficient lactase for a child is developmental delay. Therefore, any of the above symptoms should be a cause for concern for parents, a mandatory visit to the pediatrician, and a reason for taking a stool test for carbohydrates.
How to prepare for a stool test for carbohydrates
The result will be as reliable as possible if the baby’s stool is collected correctly. It is necessary to feed a newborn in his usual way. The diet cannot be changed a few days before the material is collected; it should be normal for the child. It is not advisable to introduce new foods into the diet.
If the child is breastfed, this rule fully applies to the mother. You should not take any medications for several days prior to a stool test for carbohydrates. They are permissible only if absolutely necessary for the health of the baby.
Material for analyzing stool for carbohydrates is taken naturally, without an enema or drugs to facilitate bowel movements.
To collect feces from a baby who can already sit on the potty, the latter should be washed with baby or laundry soap, scalded with boiling water, and dried. Feces from very young children should be collected from the most sterile oilcloth.
Biomaterial scraped from the inside of a disposable diaper or fabric (sheets, diapers) is not suitable for analyzing stool for carbohydrates.
For analysis, a volume of stool equal to approximately one teaspoon is enough. The mixture should be collected in a clean container with a lid. It should close tightly, preventing air from entering there.
It is advisable to purchase a container with a stick for collecting material. Similar special containers are sold in pharmacies. Their cost is relatively low. After collection, the box should be delivered to the laboratory within four hours.
The countdown begins after the act of defecation.
Decoding the results of fecal analysis for carbohydrates
The pediatrician evaluates the result of a stool analysis for carbohydrates, while simultaneously comparing the data with the presence of other symptoms, the general state of health, and the child’s well-being.
Even if a stool test for carbohydrates shows a slight deviation, but the baby behaves well and no pathological symptoms are identified, treatment is not prescribed. A false positive result is usually assumed.
Repeated stool testing is scheduled.
What is included in a stool test for carbohydrates in infants? The content of carbohydrates in the masses under study, their acidity, the number of fatty acid molecules, leukocytes, and the presence of protein are assessed.
If lactose is poorly tolerated by the body, traces of it will certainly be found in children's feces. A lot of carbohydrates, proteins, and leukocytes indicate the presence of inflammation.
With an increased content of fatty acids, the intestines poorly absorb food. All this accompanies poor absorption of lactose in the body.
Highly acidic feces (having a pH of up to 5.5) are often observed when acetic and lactic acid are included in the process of breaking down undigested lactose.
Parameter Reference values Units of measurement
| carbohydrates in feces | Age |
| 0 - 2 weeks2 weeks - 6 months6-12 months | % |
The normal amount of carbohydrates in infant feces is up to 0.25% of the total volume. The detected elements can be either lactose, galactose, or glucose. If it is necessary to clarify the diagnosis, the doctor will prescribe additional examinations to prescribe treatment.
Deviations from normal value
What does the carbohydrate content in feces mean for a healthy baby under one year of age?
Carbohydrate indicators, % Explanation
| 0-0,25 | normal amount of carbohydrates, no lactase deficiency |
| 0,25-0,50 | minor digestive dysfunction, no treatment required |
| 0,60-1,00 | moderate form of lactose intolerance |
| More than 1.00 | observed only with lactase deficiency, therapeutic measures are required |
In infants up to the age of three months, the content of carbohydrates in feces is slightly higher than normal. This is caused by the formation of the digestive system, food processing, and enzyme secretion.
Up to 0.6% carbohydrate content is considered a conditional norm. 0.7 - 1% also do not require therapeutic intervention, in the absence of associated symptoms.
The health of such babies, their nutrition, and the introduction of complementary foods should be kept under the supervision of a pediatrician.
The body consumes a lot of carbohydrates from liquid and sweet foods. Lactase deficiency is diagnosed when there are more than 1% of detected carbohydrate inclusions in the test masses, provided they are highly acidic.
Source: https://ruanaliz.ru/kal/analiz-kala-na-uglevody-u-grudnichkov/
Advantages and disadvantages of the method
Fecal carbohydrate testing is widely used due to its low cost and ease of implementation. However, it has disadvantages:
- In infants, the microflora of the large intestine is just populating, so lactose is not utilized in the large intestine and more of it ends up in the feces, sometimes the content exceeds 1%.
- The method does not allow determining the content of individual carbohydrates: lactose, sucrose or glucose for the purpose of differential diagnosis of lactase, sucrase or other types of deficiency. It should be noted that lactase deficiency is much more common than other types.
Symptoms
The severity of hypolactasia occurs individually in each person. Symptoms of lactase deficiency in adults are similar in both forms of milk intolerance. The difference is that:
- the primary form and severity of symptoms depend on the large amount of milk entering the body,
- and in the secondary form, the symptoms flourish even when a minimal amount of milk sugar is ingested, since its breakdown in the inflamed mucous membrane of the small intestine is completely impaired.
But basically, the symptoms indicating lactose intolerance, which is caused by lactase deficiency, come down to the following manifestations.
- Symptoms are always associated with the consumption of milk or dairy products;
- There may be diarrhea, but constipation is no less common, sometimes an alternation of symptoms: sometimes diarrhea, sometimes constipation;
- constant uterine rumbling, pain, possible nausea;
- loss of appetite and feeling of severe bloating - flatulence
An adult may suspect lactose intolerance in himself, even before undergoing tests, if he knows the main symptoms, as well as the fact that no treatment methods help with this pathology, except strictly following a lactose-free diet.
The symptoms are very similar to irritable bowel syndrome, and the only way to differentiate one condition from the other is by completely eliminating dairy products. Sometimes these two pathologies coexist.
Carrying out analysis
Determination of carbohydrates in feces is carried out using the Benedict reaction or using test strips. There are several reactions for determining reducing sugars, which include lactose: the Trommer, Felling and Benedict reaction and others. They are based on the ability of some sugars in an alkaline environment to reduce metals in the salt, which leads to a change in the color of the solution. The reaction with Benedict's reagent is the most sensitive, that is, it allows one to detect very low carbohydrate content in a sample of material.

An equal amount of Benedict's reagent is added to a few drops of stool centrifugate. The test tube is placed in a water bath for several minutes, and after cooling, the result is assessed.
Carbohydrate content norm and interpretation of results
Carbohydrates in feces can normally be present in almost all infants, but their content must be within the established limits. Reference (normal) value - up to 0.25%. However, when deciphering the results, it is worth considering the following nuances:
- In newborns and infants at 2-3 months, the values may exceed the norm, since at this age the secretion of enzymes and digestion are at the stage of formation.
- If the analysis results show that the percentage of carbohydrates in feces is up to 0.6, there is no need to worry. Experts believe that these figures can be considered the norm.
- If the value is from 0.7 to 1.0%, treatment is not prescribed if the child does not have tummy problems. Such children are taken under control and are recommended to undergo repeated testing. If the result remains within the same range, the pediatrician may prescribe enzymes, for example Lactase Baby.
- More than 1% carbohydrates in feces indicates a high probability that the baby will have lactase deficiency (more details in the article: how is lactase deficiency treated in infants?). An indirect confirmation of the diagnosis will be increased acidity of the stool if the pH value is lower than 5.5.
INTERESTING: how to collect feces from a baby for coprogram? Pediatrician of the 2nd category, allergist-immunologist, graduated from the Belarusian State Medical University of the Federal Agency for Health and Social Development. Read more », Rate this article: (5 rated 4.40 out of 5) Loading...Share with friends!
Analysis results
Benedict's reagent contains copper sulfate, the solution of which is blue. If there are no sugars in the stool, the reaction does not occur, the mixture remains blue. If lactose is present in the stool, it oxidizes the copper ion to brick-red copper(I) oxide. A small amount of carbohydrates will produce a small amount of reddish oxide, which mixes with the blue color of the sulfate, resulting in a green color.
Interpretation of stool analysis for carbohydrates in infants:
- up to 2 weeks - no more than 1%,
- from 2 weeks to 6 months - 0.5-0.6%,
- from 6 months to a year - 0-0.25%,
- older than a year - 0%.
For newborns up to 2 weeks of age, a result of 1% and below is good; it indicates the formation of the microflora of the large intestine. A result greater than 1% is considered a deviation and requires a careful approach. Most likely, the analysis will need to be retaken.
For a breastfed or bottle-fed child from 2 weeks of age to 6 months, a good indicator is below 0.5-0.6%, indicating the absence of lactase deficiency. If the result is higher, lactase deficiency is possible. In children of this age, an increased content of carbohydrates in the feces is often noted, which most often indicates the immaturity of the digestive tract.
For children older than one year, the result should be 0%. If it is higher, incomplete utilization of lactose may be suspected. Most likely, the cause is pathologies of the intestinal tract or dysbiosis.
In children over 3-5 years of age and adults, the result should be 0%. An increased result most often indicates adult-type lactose intolerance, which occurs in 70% of the world's population.
Exceeding the norm is not a basis for making a diagnosis. Other studies are also needed. Therefore, a doctor should interpret the stool test for carbohydrates.
Norm of carbohydrates in feces
| Patient age | Amount of carbohydrates |
| Children under 1 year | 0 – 0,25% |
| Children over 1 year old and adults | Not detected |
Note: in children of the first year of life the following deviations from the norm may be observed:
- 0.3 – 0.5% (insignificant);
- 0.6 – 1% (average);
- more than 1% (significant).
Factors influencing the result:
- Violation of the rules for preparing for analysis;
- Errors when collecting biomaterial;
- Features of the daily diet;
- Patient's age;
- Genetic factors and family history;
- Intestinal infection or inflammation;
- Taking prebiotics, antibiotics and other drugs.
Signs of lactose, sucrose and monosaccharide intolerance
- It is recommended to read labels and limit consumption of products that contain milk sugar: for example, mayonnaise, sauces, candies
- Most patients can safely drink one glass of milk without developing unpleasant symptoms.
- Yogurt and cheese usually do not cause unpleasant symptoms
- You can consume fermented milk, soy milk,
- Calcium supplementation is recommended.
- Full-fat milk and chocolate milk are generally better tolerated than skim milk
Treatment of acute disorder
As we have already agreed, primary natural lactose intolerance should not be treated with pills. Secondary lactase deficiency is treated as follows:
- exclude the intake of lactose, that is, milk and dairy products;
- treat the disease that is the source of enzyme deficiency (for example, acute gastroenteritis);
- provide the body with the necessary enzymes to digest lactose; use the lactase enzyme in tablets or capsules.
And finally, a little more linguistics: “Lactose deficiency”, from a linguistic point of view, means “lack of milk sugar” in the body, theoretically, lactose deficiency - this could be called a lack of milk sugar in mother’s milk in a newborn or some kind of nutritional disorder in starving children in Africa.
My inquisitive mind forced me to find in medical journals a study of lactose deficiency in infants (Lactose Deficiency in Infants Clinical Pediatrics 11/2008); BUT this term has nothing to do with the topic of our article and the fact that adults do not digest milk sugar.
Sincerely, doctor A. Novocidou
Treatment of lactase deficiency
The treatment is carried out by a pediatrician.
First of all, it is necessary to establish the cause that caused lactose intolerance and try to eliminate it.
In case of secondary lactase deficiency, infectious and non-infectious enterocolitis, helminthiasis, giardiasis and others are treated. The duration of treatment for secondary lactase deficiency corresponds to the period of treatment for the underlying disease: 14 days or more.
Mom's diet while breastfeeding
In case of primary lactose intolerance, mothers are advised to limit or completely avoid whole milk, but keep fermented milk products, butter and cheeses in the diet, since they are the source of calcium needed by the baby. Also, a nursing woman should reduce her intake of sweet foods. However, it is important that the diet itself is balanced.
In no case should you give up breastfeeding, since mother’s milk, in addition to nutrients and vitamins, contains antibodies that create the child’s immunity and lactase. Most of the enzyme is present in hind milk, so the baby should suckle at the breast for at least 20 minutes. Night feedings should also not be stopped, because it is at night that hind milk is produced in greater quantities.
For moderately severe lactose intolerance, it is recommended to add Lactase Enzyme, Lactase Baby or Lactazar to breast milk. To do this, before starting feeding, you should express about 50 ml of milk and dissolve one of the listed drugs in it. After a minute, give the mixture to the baby from a spoon and continue breastfeeding. Enzymes must be added to each feeding without skipping; the dose volume depends on the level of carbohydrates in the feces.
Lactase withdrawal should occur gradually, as breastfeeding decreases due to the introduction of complementary foods.
Diet of children on artificial nutrition
For formula-fed children, lactose-free, low-lactose or soy formulas should be selected.
Complementary foods for children with lactase deficiency begin to be introduced earlier; vegetable purees and cereals are prepared on lactose-free or low-lactose bases. Fruit juices, on the other hand, are added to the menu later. Children should be given yoghurts, fermented milk mixtures with live biobacteria, and cheeses.
| The product's name | Company, country of origin | Ingredients | Energy value, kcal | ||||||||
| squirrels | fats | carbohydrates | |||||||||
| Total | lactose | ||||||||||
| lactose-free mixtures | |||||||||||
| Nutrilak lactose-free | Nutritek Group, Russia | 1,6 | 3,5 | 7,3 | 0 | 66,3 | |||||
| NAS lactose-free | Nestlé, Switzerland | 1,7 | 3,3 | 7,6 | 0 | 67 | |||||
| Enfamil Lactofri | Mead Johnson, USA | 1,42 | 3,7 | 7,2 | |||||||
| low lactose mixtures | |||||||||||
| Nutrilak low lactose | Nutritek, Russia | 1,6 | 3,5 | 7,3 | 0,9 | 66,3 | |||||
| Nutrilon low lactose | Nutricia, Holland | 1,4 | 3,6 | 7,1 | 1,33 | 66 | |||||
| Humana-LP | Humana, Germany | 1,8 | 2,0 | 9,2 | 1,1 | 62 | |||||
| Humana-LP+SCT | Humana, Germany | 1,9 | 2,0 | 8,9 | 0,5 | 61 | |||||
Table. Chemical composition and energy value of low-lactose and lactose-free milk formulas (in 100 ml of finished mixture)
In older children and adults, lactase deficiency is moderate to mild. They are advised to avoid whole milk, condensed milk and ice cream for life. Fermented milk products and cheeses are not limited.