How to measure the temperature under the arm
Most often, we measure the temperature under the arm with a regular mercury or electronic thermometer. Here's how to do it right:
- You should not take your temperature after eating or exercising. Wait half an hour.
- Before starting the measurement, the glass thermometer must be shaken off: the mercury column should show less than 35 °C. If the thermometer is electronic, just turn it on.
- The armpit should be dry. The sweat needs to be wiped off.
- Keep your hand pressed tightly. In order for the temperature under the armpit to become the same as inside the body, the skin must warm up, and this takes time. It is better to press the child’s shoulder yourself, for example, by picking up the baby in your arms.
- The good news: if you follow the previous rule, the mercury thermometer will take 5 minutes, not 10, as is commonly believed. Many electronic thermometers respond to temperature changes and measure as long as these changes exist. Therefore, if you do not press your hand, the temperature may change for a long time and the results will be inaccurate.
How to measure temperature rectally
This method is sometimes needed when you need to check the temperature of babies: it is difficult for them to hold their hand, it is unsafe to put something in their mouth, and not everyone has an expensive infrared sensor.
- The part of the thermometer that you will insert into the rectum should be lubricated with petroleum jelly or petroleum jelly (available at any pharmacy).
- Place the child on his side or back, bend his legs.
- Carefully insert the thermometer into the anus 1.5–2.5 cm (depending on the size of the sensor), hold the child while the measurement is taken. A mercury thermometer should be held for 2 minutes, an electronic one - for as long as written in the instructions (usually less than a minute).
- Remove the thermometer and look at the data.
- Treat your child's skin if necessary. Wash the thermometer.
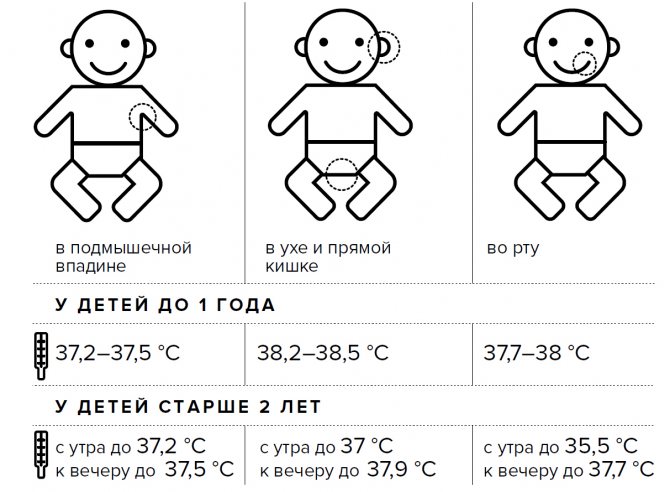
What indicators are considered normal?
What indicators are considered normal? A temperature in the range from 36.6 to 37.3 is considered normal. But as you know, different parts of the body have different temperatures. There are two concepts: core and periphery temperature. The core is our internal organs with good blood supply - the liver, the heart, where the temperature reaches 38 degrees. And the periphery is our limbs, where the temperature can reach 27.
- 36.6 - 37.4 C - in the armpit,
- 36.7 - 37.3 C - temperature in the oral cavity,
- 36.8 - 38.1 C - temperature in the rectum.
Let's consider temperature fluctuations in children under one year old in the armpit. Everything is considered provided that your baby feels well, has no sniffles, and is not capricious.
- 1 month – 37.0 -37.7 C,
- 2 months – 36.9 – 37.5C,
- 3 months – 36.8 -37.6 C,
- 4 months – 36.7 -37.6 C,
- 5 months – 36.6 -37.6 C,
- 6 months – 36.6 -37.6 C,
- 7 months – 36.6 -37.5 C,
- 8 months – 36.6 -37.5 C,
- 9 months – 36.6 -37.4 C,
- 10 months – 36.6 -37.2 C,
- 11 months – 36.6 -37.0 C,
- 12 months or 1 year – 36.6 -36.9 C.
How to measure ear temperature
There are special infrared thermometers for this: it is useless to stick other thermometers into the ear. Age guidelines do not measure ear temperature in children under 6 months of age because due to their developmental characteristics the results will be inaccurate. You can measure the temperature in your ear only 15 minutes after you return from the street.
Pull your ear slightly to the side and insert the thermometer probe into your ear. It takes a few seconds to measure.
Uptodate.com
Some infrared devices measure temperature on the forehead, where the artery runs through. Data from the forehead or from the ear is not as accurate Fever: First aid as with other measurements, but it is fast. But for household measurements, it is not so important what your temperature is: 38.3 or 38.5 °C.
How to read a thermometer
The measurement result depends on the accuracy of the thermometer, the correctness of the measurements and where the measurements were taken.
The temperature in the mouth is higher than under the armpit by 0.3-0.6 °C, rectal - by 0.6-1.2 °C, in the ear - up to 1.2 °C. That is, 37.5 °C is an alarming figure for measurement under the arm, but not for rectal measurement.
The norm also depends on age. In children under one year old, the rectal temperature is up to 37.7 °C (36.5–37.1 °C under the arm), and there is nothing wrong with that. The 37.1°C under the armpit that we suffer from becomes a problem as we age.
In addition, there are individual characteristics. A healthy adult's temperature ranges from 36.1 to 37.2°C under the armpit, but someone's personal normal is 36.9°C and someone else's is 36.1. The difference is big, so in an ideal world it would be nice to take your temperature for fun when you are healthy, or at least remember what the thermometer showed during your medical examination.
Most often, when a baby shows signs of illness, parents try to find out if their child has a fever. Indeed, measuring his body temperature is a convenient method of assessing the baby’s health. Of course, the absence of a rise in temperature does not at all guarantee that everything is fine with the child, because well-being must be considered comprehensively. However, an elevated temperature in a child is a clear sign that something is wrong.
Measuring the temperature of a child who was recently born is not so difficult, but for the first time it can cause some difficulties - after all, the baby cannot sit quietly for the prescribed 10 minutes with a thermometer pressed under his arm. What to do?
Normal body temperature in a child up to one year old
An elevated temperature in a child is always a trigger for parents to panic. But many do not suspect that the temperature in children under one year old can range from 36.6 to 37.5. Why? The answer is simple.
Immediately after birth, the infant's thermoregulation system is not formed. Heat transfer processes prevail over heat production. That’s why all mothers wrap up their child so much in the first months of life.
What indicators are considered normal?
What indicators are considered normal? A temperature in the range from 36.6 to 37.3 is considered normal. But as you know, different parts of the body have different temperatures.
There are two concepts: core and periphery temperature. The core is our internal organs with good blood supply - the liver, the heart, where the temperature reaches 38 degrees.
And the periphery is our limbs, where the temperature can reach 27.
- 36.6 - 37.4 C - in the armpit;
- 36.7 - 37.3 C - temperature in the oral cavity;
- 36.8 - 38.1 C - temperature in the rectum.
Let's consider temperature fluctuations in children under one year old in the armpit. Everything is considered provided that your baby feels well, has no sniffles, and is not capricious.
- 1 month – 37.0 -37.7 C;
- 2 months – 36.9 – 37.5C;
- 3 months – 36.8 -37.6 C;
- 4 months – 36.7 -37.6 C;
- 5 months – 36.6 -37.6 C;
- 6 months – 36.6 -37.6 C;
- 7 months – 36.6 -37.5 C;
- 8 months – 36.6 -37.5 C;
- 9 months – 36.6 -37.4 C;
- 10 months – 36.6 -37.2 C;
- 11 months – 36.6 -37.0 C;
- 12 months or 1 year – 36.6 -36.9 C.
How to measure temperature correctly
Some mothers do not approach temperature measurement correctly, using their subjective sensations (I put my lips to the child’s forehead). Thermometry is the best way to measure temperature. For infants, it is better to use an electronic thermometer, as it is safer and takes less time to measure.
The standard is to measure temperature in the left armpit. Before measuring, it is better to hold the thermometer in your hands and warm it up so that the child does not feel discomfort.
It is best to measure the temperature 2 hours after eating, so that the child is calm, does not become capricious, and does not engage in intense physical activity (running, jumping).
If you have a mercury thermometer, you should not lower the temperature below 36.3-36.0. The mercury thermometer increases very quickly for the first 2 minutes, then it moves for a very long time, and only by tenths of degrees, they have no fundamental significance. If your child has a fever, it will rise in 2 minutes, there is no need to torture the child.
Infants and children up to one year old can have their rectal temperature measured. There the norm is considered to be from 36.8 to 38.1. We lay the child on your knees on his tummy and insert the thermometer 1.5-2 cm into the butt. We hold it there for about one minute and take it out. And we evaluate the results.
If a child has a disease, the temperature should be measured every 3 hours. The temperature must be measured until normal individual values appear.
How to maintain your baby's temperature at the same level
You should always remember that the temperature of infants is always higher than normal values, the second is adjusted depending on their condition (eating, crying, playing).
How to measure the temperature of newborns and infants?
The correct choice of a thermometer for measuring body temperature largely determines the reliability of the results obtained, so when buying a thermometer for a baby (and the baby needs its own device, separate from adults), it is worth weighing all the pros and cons.
When time counts down to seconds, special scales are used to assess the condition of a newborn in the first moments of life, allowing you to make a quick and accurate decision about how much specialized help and care the baby needs
Mercury thermometer
(maximum mercury thermometer), when used correctly, is accurate, but to a certain extent it is dangerous to use: the glass case can break and injure with fragments, and the mercury contained in it is dangerous due to its vapors. In addition, measuring temperature with such a thermometer takes a certain time.
Due to the listed features, using a mercury thermometer to measure temperature for newborns and infants is not very convenient.
Digital Thermometer
. Today there are a lot of electronic thermometers on sale that vary greatly in quality and price. And, unfortunately, many of them, due to poor quality, are not able to show the correct temperature or quickly fail. Such thermometers must be checked periodically. Please note that for the baby it is better to take a waterproof thermometer that can be washed.
The easiest way to evaluate the reliability of the readings of an electronic thermometer is to compare the results it produces with the reading of a mercury thermometer. An adult family member (!) measures his body temperature first with mercury and then with an electronic thermometer (or in reverse order) and the readings are compared.
A type of electronic thermometer is a nipple thermometer. This is a special pacifier in which a temperature sensor is inserted - the child sucks on the pacifier and at the same time the temperature in the mouth is measured.
Infrared thermometer
. An infrared thermometer measures the temperature emanating from an object using an infrared sensor. Thermometers of this type can boast very high accuracy. The most convenient way is to measure the temperature in the ear - a special attachment will not allow you to insert the thermometer too far, and you will get the result almost instantly. However, they are not recommended for children under 3 months, as they may show incorrect results due to the structural features of the newborn ear.
Many infrared thermometers can measure forehead temperature. However, this procedure does not always give accurate results, since the temperature of the forehead skin can change not only depending on how you feel, but also on environmental factors (for example, room temperature, heating of the forehead by the sun, etc.).
Strips for measuring body temperature.
This strip is applied to the forehead and highlights a number indicating the temperature of the forehead. The strips are an imprecise diagnostic tool, but they can at least roughly indicate the presence of temperature.
There are disposable varieties of such thermometers. For example, the Fevermonitor Continuous Measurement Thermometer, which allows you to attach an inconvenient small sticker to your child’s forehead that will continuously show their temperature throughout the day. This relieves parents of the need to constantly measure the temperature of a sick child.
Body temperature norms for children and adults
Home / Facts
Share on Facebook VKontakte Twitter Odnoklassniki
Did you know that normal human body temperature is also called normothermia? It can be measured in the mouth, in the ears, in the armpit or rectally. The result depends on the place. Age, a person’s activity level, and in women also the stage of the menstrual cycle also play a role.
A few facts:
- Temperatures may vary throughout the day.
- The temperature may be too low, or it may rise above normal.
- A temperature above 38°C most often means you have a fever caused by an infection.
- Normal temperature ranges from 36.5°C to 37.5°C.
- Depending on the part of the body in which you measure the temperature, thermometers will also differ.
What is the normal temperature for an infant?
In the first months of life, the temperature fluctuates around 36°C - 38°C.
What is a child's normal body temperature?
On average, a child's normal body temperature is about 37°C. Usually in the morning - 36.3°C, and in the evening - up to 37.6°C.
What is the normal body temperature for adults?
In the mouth - 36.8°C. In the armpit - 36.5°C. Rectal or ear temperature: 37.5°C.
At what temperature does fever begin?
The American Academy of Pediatricians insists that a fever is any temperature that rises above normal.
What is basal body temperature?
Basal temperature is the lowest temperature achieved during rest and sleep. Basal temperature should be measured immediately after waking up, but even then it will be higher than during sleep. In women, basal temperature differs at different periods of the menstrual cycle. With its help, you can track ovulation to avoid or promote pregnancy.
What is core temperature?
This is the working temperature of the body, which relates to certain organs, for example, the liver. This temperature will be different from normal because it is maintained within a narrow range of the body.
What is hyperpyrexia?
This is the name of a fever with the highest temperature readings. They can even exceed 41.5°C.
What is hyperthermia?
High temperature, which is not as dangerous as the one we talked about above. The causes of hyperthermia can be heat stroke, reactions to medications, stimulants.
What is hypothermia?
Decrease in body temperature below 35°C. It can be caused by hypothermia or loss of strength.
As you can see, temperature has many different indicators and values that really affect your health. To avoid problems, you should take your temperature whenever you feel unwell. If the readings are above or below average, consult a doctor!
Source
Share on Facebook VKontakte Twitter Odnoklassniki
Where to measure the body temperature of a newborn or infant?
In both children and adults, temperature is traditionally measured in the armpit, but there are other options:
- In the armpit or inguinal fold
- Temperature in the anus (rectal temperature)
- In the ear (tympanic temperature)
- In the mouth (oral temperature)
- Forehead temperature
The most suitable measurements for newborns and infants are measurements in the mouth (requires an electronic thermometer), in the anus (in other words, in the butt) (requires an electronic thermometer) or in the ear (requires an infrared (tympanic) thermometer). Despite this, you can also measure the temperature in the armpit.
Measuring the temperature of newborns and infants in the armpit
Measuring the temperature under the arm is traditional, but has its own characteristics that you definitely need to know about.
Firstly
- if you suspect an increase in temperature, it is necessary to evaluate the body temperature, and when applying a thermometer to the armpit, the thermometer will measure the temperature of the skin surface. Therefore, to obtain correct results, the position of the hand immediately before measuring the temperature is extremely important:
- If the hands were raised, the measurement will show a temperature lower than the real one;
- If the hand was pressed to the body for at least 5 minutes, the temperature measured in the armpit will correspond to the real body temperature.
Based on this, in order to measure the temperature correctly, you need to press your hand to your body for several minutes before placing the thermometer under your arm. To measure temperature with a mercury thermometer, it is enough to hold the thermometer for 5 minutes.
Secondly
– the skin in the armpit must be dry before placing the thermometer there. Moisture from sweat can also cause unreliable results.
Regardless of whether you take measurements with a mercury or electronic thermometer, you must keep the child’s hand tightly pressed to the body throughout the measurement, and be extremely careful with the mercury device. The tip of the thermometer should be exactly under the armpit, and not stick out or rest against the folds of clothing.
Measuring the temperature of newborns and infants in the anus
For this type of measurement, the tip of the thermometer, pre-lubricated with Vaseline, is inserted shallowly into the baby’s anus. The child's legs must be kept bent. This type of measurement is not recommended to be carried out with a mercury thermometer due to the risk of damage.
Measuring the temperature of a newborn or infant in the ear
To measure tympanic temperature, only infrared thermometers are used, which assess the temperature of the eardrum in the child’s ear. The infrared thermometer is fast (only a couple of seconds), safe and accurate. Under no circumstances should you put a mercury or electronic thermometer into your ear.
Measuring the temperature of a newborn or infant in the mouth
The already mentioned thermal pacifier will help parents with this. Under no circumstances should you put a mercury thermometer into your baby’s mouth.
Measuring the temperature of a newborn or infant on the forehead
This type of measurement is not very accurate. Can be done with an infrared thermometer or strips to measure body temperature.
Question No. 2 Why 36.6 (what is “normal temperature” and where did it come from)?
In most animals - insects, spiders, fish, reptiles - the intensity of metabolism is directly related to the ambient temperature: the warmer it is, the more active the metabolism is. In the summer, these animals grow, feed and reproduce, with the onset of cold weather they become lethargic, lose their appetite, cease to be interested in the opposite sex, etc.
Insects, spiders, fish and reptiles are cold-blooded animals. The body temperature of the tarantula, grasshopper, perch and crocodile is almost equal to the ambient temperature.
The climate of planet Earth is characterized by the fact that most territories are subject to significant daily and seasonal temperature fluctuations. Nature (or the Creator) was not at all satisfied with this state of affairs, when the intensity of life is determined by the weather. Well, what good is this - in winter there’s no one to even talk to! And then warm-blooded animals appeared - birds and mammals.
The fundamental feature of warm-blooded animals in general and humans as a classic representative of warm-blooded animals in particular is that their body temperature is constant and very stable, it does not depend on the ambient temperature, and even if it fluctuates, it is within very small limits, usually not exceeding 1–2 ℃.
Each specific species of birds and mammals has its own normal body temperature.
Normal body temperature is the temperature that is characteristic of the vast majority of individuals of a given biological species in a state of health.
Normal temperature:
• for chicken – 40.5–42.5 ℃,
• for a rabbit – 38.5–39.8 ℃,
• for pigs – 39.0–40.0 ℃.
The normal human body temperature is considered to be 36.6 ℃.
Why 36.6? Where did these numbers come from? The answer to this question is found in the very, very distant year of 1868. It was then that the German doctor Wunderlich (CRA Wunderlich) carried out about 1 million body temperature measurements on 25,000 patients. The temperature was measured in the armpit, and the average was 36.6. This is how things have happened since then...
Normal body temperature
Despite the well-known “standard” temperature – 36.6 °C – not everything is so simple in this matter.
For example, body temperature standards vary depending on the patient's age.
It is worth noting that it is necessary to take a comprehensive approach to assessing the baby’s condition - if a child at a normal temperature exhibits lethargy, poor appetite and other signs of deterioration in health, it is necessary to consult a doctor.
The norms of temperature measured in different parts of the body also differ:
- The temperature in the anus is 0.6-1.2 °C higher than the temperature under the armpit;
- The temperature in the mouth is 0.3-0.6 °C higher than the temperature under the armpit;
- The temperature in the ear is 0.6 - 1.2 °C higher than the temperature under the armpit.
Thus, if an infrared thermometer shows a temperature in the ear slightly exceeding 37 ° C, then this is completely normal.
WHAT IS THIS?
Fever is an increase in normal body temperature. The norm ranges from 36.5 to 37.5 ºC. Typically, fever is a reaction of the immune defense system to an attack by an infectious pathogen (bacteria or viruses) or to any foreign object. Therefore, it is a beneficial natural reaction that helps us get better.
HOW TO MEASURE?
The actual body temperature is the so-called “core temperature”, in other words, the temperature of the internal organs. The ideal location for measurement is the pulmonary artery, but this method is inconvenient and invasive.
Temperature can be measured in different parts of the body both internally (orally, rectally, in the ear canal) and externally (in the armpit, forehead and temples). On average, the temperature in the armpit is half a degree lower than in the rectum, mouth or ear.
Moreover, body temperature can:
- fluctuate throughout the day (lower in the morning and higher in the evening);
- vary (each person has their own normal body temperature);
- vary depending on where on the body it was measured. Also, the temperature may not be the same on the left and right sides of the body.
Various instruments (infrared or electronic) are used to measure temperature:
Is temperature 37.5 normal or to sound the alarm? When we see readings above 37 degrees on the thermometer, we begin to panic. However, you should not immediately make diagnoses and take antipyretic drugs. In fact, the normal body temperature for an adult is in the range from 35.9 to 37.5 degrees, often depending on a number of individual characteristics.
Babies have normal body temperatures that differ from adults. In the first months of life, babies have a temperature close to the temperature in the womb. This is approximately 37.7-38.2 degrees. Further up to a year, the temperature may be elevated, since the child has not yet developed thermoregulation.
The most technologically advanced type of thermometers today are infrared thermometers.
Infrared thermometer B. Well Swiss WF-1000 is an accurate, fast and reliable assistant for the whole family. Its unique 2-in-1 design allows you to measure temperature in two ways: in the ear or at the temples. To select the measurement method, simply put on or remove the cap.
Measuring temperature in the ear is convenient and fast. Thermometer B. _ Well Swiss WF-1000 will measure the temperature with one touch in 1 second! In order to carry out the procedure, it is necessary to remove the cap from the device and insert the sensor into the ear canal. Next, press the measurement enable button once and wait for the sound signal. Then remove the sensor from the ear canal. The result will be displayed on the screen.

The thermometer is made of safe plastic and does not contain mercury or glass. It has a waterproof sensor that can be easily treated with a disinfectant solution.
It is important to know that we have different temperatures in different parts of the body. For example, the temperature in the mouth or ear will be higher than the temperature in the armpit. This is due to the fact that the temperature of the mucous membranes is higher than the temperature of the skin.
The normal temperature in the ear is 35.5-37.5 degrees!
Remember that the thermometer must be in the room where the temperature will be measured for at least half an hour, and the patient for at least 10 minutes. Otherwise, the results may not be accurate.

Despite all its advantages, an infrared ear thermometer has several cases when it is not suitable for use.
- During an inflammatory process in the auricle , for example, otitis media.
Inflammation distorts the thermometer readings. In such cases, the device gives inflated results. If only one ear is inflamed, measure the temperature in the other for comparison.
- You cannot measure the temperature in the ear if there is an injury , for example, a damaged eardrum.
It is important to keep the thermometer sensor clean, as buildup of wax and dirt can also reduce the accuracy of the readings.
Measuring temperature in the ear is one of the most modern, fast and convenient methods. In addition, this is the most gentle way to measure temperature in babies. It is painless and does not take much time. The B.Well Swiss WF-1000 thermometer is an excellent choice for the whole family. Thanks to the combined measurement method - both on the forehead and in the ear canal - you can always easily control the temperature.
Share this article with your friends
Temperature measurement axillary (in the armpit):

BEHIND:
- Convenient and non-invasive measurement method.
AGAINST:
- Takes a few minutes.
- Patient assistance is required for proper placement of the thermometer.
- Can detect fluctuations in core body temperature after only 1 hour.
External factors can affect body temperature. Be careful when placing the thermometer in the armpit. Make sure your armpits are dry and hold your child while they take their temperature.
To make the process easier, use thermometers with specially adapted sensors for children or quick-release thermometers (60 seconds). Remember, thermometers that measure axillary temperature for less than 60 seconds cannot be considered reliable.
Measuring temperature rectally (in the rectum):
Using an electronic thermometer:

BEHIND:
- Ideal for babies.
- Fast.
- Reliable.
AGAINST:
- May be a little annoying for baby.
- Risk of local (local) damage.
- Inconvenient.
- Not suitable in case of diarrhea or inflammation of the rectum.
- Can detect fluctuations in core body temperature after 1-5 hours.
Lubricate the tip of the thermometer with Vaseline or olive oil. When taking the temperature, try to hold your baby and do not place him on his back. The result cannot be considered reliable for diarrhea or inflammation of the rectum.
When measuring temperature rectally, the indicator may be half a degree higher compared to the axillary method. To make the process easier, use thermometers specifically designed for taking children's rectal temperature (short flexible tip).
normal temperature for a child
Good afternoon. Help me figure it out. On Wednesday 9.10 I took a snotty child with red cheeks from the garden, in the evening the temperature rose to 38.7 and gave Nurofen syrup, before that only suppositories, and since suppositories were forbidden I had to give Nurofen syrup, with screams or shouts instead of 5 ml they were able to pour in at most 1-2 ml, but no less, the child fell asleep, sweated, the temperature dropped to 37.4, in the morning it rose again to 38.5, they called a doctor to the house, there was no wheezing, but a red, loose throat, treatment: Orvirem, Nurofen / paracetamol, Meramistin in the throat, Aqualor in the nose, in the evening the temperature rose 39.7 paracetamol suppository did not give any effect, we also spat out the syrup, we decided to call a doctor, there was also no wheezing, a red throat without plaque, a preliminary diagnosis of sore throat, they suggested going to the infectious disease clinic, but I refused, the emergency doctor gave an injection, after the promised 15 minutes the injection it didn’t work, and even after 1/1.5 hours the temperature remained at 39.7, they were able to lower it to 38.6 by wiping it with water, in the morning the temperature rose again, they inserted cefekon, it dropped to 38.5, the doctor came at the request of the ambulance and looked at the throat , listened and suggested two developments of sore throat or Roseola because the temperature does not go down, she suggested waiting until Sunday for a rash to appear, and in the meantime bring down the temperature and spray the throat, if on Sunday the temperature does not subside, start giving amoxiclav, on Saturday morning the temperature is 37 , in the afternoon 36.8 in the evening again 38.5, nothing brought it down on Sunday morning 36.6 on the lower back, forehead and chin I saw a rash, after lunch the temperature was 38.4 they decided to start taking antibiotics, all night the temperature was 37.8 in the morning 36.5, the rash went all over the back, behind the ears and a little bit on the stomach, we went to donate blood, called a doctor at home, the doctor who came on the very first call came, the temperature was normal, the throat was good, the rash was nothing to worry about... the diagnosis was ARVI + Allergy.. Blood tests came, the temperature was no longer rose, the rash became lighter, and in some places completely disappeared. See the doctor only on Monday, tell me what happened? Or is there? How to evaluate the blood result? She continues to take antibiotics, the child is screaming like a beluga, it’s a pity to torment her voice is already hoarse... When can I retake the test, the doctor did not answer anything (Blood test, everything is normal except: *Leukocytes 4.4 with a norm of 6.0-17.0 *segmented neutrophils 16 with a norm of 28-48 * Neutrophils (total number) 17 with a norm of 29.0-54 * Lymphocytes 74 with a norm of 37.0-60 * ESR 17 with a norm of <12
Measuring body temperature on the forehead or temples

Using an infrared thermometer.
Two measurement methods are used: contact and non-contact.
Usually, when measuring temperature at the temples, a contact method is used, and at the forehead, a non-contact method is used.
BEHIND:
- Comfortable.
- Very fast.
- Non-invasive.
- Reliable indicators of core body temperature (a few millimeters below the temporal region is the temporal artery, which carries blood from the heart to the brain).
AGAINST:
- The influence of external factors and problems with blood circulation.
- The thermometer must be used correctly to get reliable results.
Allow the thermometer to adapt to the temperature of the child's environment for 20-25 minutes. If the child comes from outside, wait at least 5 minutes before taking the temperature. To understand whether a child has a fever, compare the reading on the thermometer with the baby’s normal body temperature, measured with the same thermometer. On average, the temperature in the temporal region is higher than in the armpit.
Take temperature measurements at the same temple to obtain valid and reliable readings that can be analyzed and compared.
Temperature norms for children of different ages
There are different ways to measure body temperature in children. The first of them is in the armpit, but it is not suitable for infants and young children. For them, you can use rectal or oral methods. The second is preferable, but it will require an electronic thermometer made of plastic, harmless to the child. It is also worth considering that indicators differ in different areas. Thus, the temperature in the armpit, although indicated in most tables, is 0.5-1 degrees lower than rectal or oral. In addition, measurements in the mouth should be taken one hour before or after a meal, since the temperature of the food can also affect the result.
Normal indicators change with age. Since metabolic processes in infants and young children proceed faster, their temperature will be higher. As you grow older, it gradually decreases and at 7 years of age it no longer differs from the measurement results in an adult. There are also individual characteristics that depend, among other things, on a person’s height, constitution and type of temperament. The average norm values for children of different ages are presented in the table. They are valid when measuring temperature in the armpit.
Age Temperature is normal, CO
Up to 1 year
37,7
1 year
37,1
5 years
37,0
7-9 years
36,7—36,8
10 years and older
36,6
It is recommended to measure temperature at rest. The most informative measurements are taken in the morning, as well as after a long rest at any time of the day. After intense physical activity, walking or eating, the indicators may differ upward by 0.5-1 degrees.
Temperature measurement in the ear canal
Using an Infrared Thermometer.

BEHIND:
- Very fast.
- Comfortable.
- A reliable indicator of core body temperature (the eardrum has the same blood flow as the hypothalamus).
AGAINST:
- Good practice is required.
- The correct placement of the sensor affects the reading (if the sensor is not accurately aimed at the eardrum, there is a risk of getting lower readings).
- The influence of local factors (otitis media, earwax).
For an accurate measurement, move the earpiece back slightly to straighten the ear canal and very carefully insert the sensor. The goal is to obtain the most accurate data.
Children under 2 years old need to gently pull the ear back.
Children over 2 years old and adults need to pull the ear up and back.
Measure your child's body temperature when he feels well to determine normal and recognize hyperthermia later. Remember that you need to measure your temperature under the same conditions, using the same thermometer, body area, method and time.
Body temperature may be higher or lower after drinking a hot or cold drink, running, taking a bath or changing location (from a hot place to a cold place), or prolonged crying. In these cases the result cannot be relied upon.
Take your temperature in the morning after waking up or late at night. Do not take your temperature during digestion or in the evening. She will be taller.
At elevated temperatures, let your child drink more liquid at room temperature (water, tea, chamomile infusion). Don't cover it too much, feed it small portions and easily digestible food. Continue breastfeeding.
The child should take antipyretic drugs only with a doctor's prescription and when the temperature measured rectally is more than 38.5 ºC (38 ºC in the armpit). And also if the child is very depressed.
Otitis media, or inflammation of the ear canals, is a disease that often occurs in childhood. Doctors say that by the age of three, 90% of children experience this disease at least once. Otitis has a number of characteristic symptoms, one of them is fever, which is very worrying for parents of sick children. How long does the fever last for this disease and how to alleviate the child’s condition?
An infectious-inflammatory process in the ear canal occurs as a complication of viral and bacterial infections of the respiratory system and nasopharynx. The causative agents of the disease are usually adenoviruses, influenza viruses, Haemophilus influenzae and pneumococci
. Due to the fact that the functioning of the immune system in childhood is not very well established, otitis often accompanies diseases characterized by difficulty in nasal breathing - sore throat, sinusitis, rhinitis, laryngitis, etc.
In infants, the reason for the development of the disease lies in the special structure of the hearing organs. A small tube, called the Eustachian tube, passes close to the pharynx in infants, which allows pathogenic microorganisms to easily penetrate the ear. In addition, children under the age of one year are constantly in a horizontal position, which is why mucus flows into the Eustachian tube, causing inflammatory processes. With age, the auditory tube becomes longer, narrower and located at a greater angle to the pharynx, as a result of which mucous secretions practically do not enter the ears.
Important!
Otitis has a number of characteristic signs by which it is quite easy to recognize the disease: ear pain, weakness, dyspeptic symptoms (nausea, vomiting) and increased body temperature, but in general the baby’s condition depends on the form of the disease.
Table. Main forms of otitis.
| Form of otitis | Symptoms |
| Lethargy and apathy, constant crying and irritability in infants, the appearance of purulent discharge from the ears, increased body temperature. Suppurative otitis is characterized by severe hyperthermia (from 38 degrees and above), and the temperature drops only for a short time, after which it rises again. | |
| Severe pain in the ear, which radiates to the head and teeth, decreased hearing, deterioration of general condition. Fever is one of the symptoms of this form of otitis, but the numbers on the thermometer depend on the functioning of the immune system. | |
| Gradual hearing loss, tinnitus. In most cases, exudative otitis media occurs without hyperthermia; sometimes low-grade fever is possible (not higher than 37-37.5 degrees). |
In addition to the above classification, otitis media is divided according to the localization of the inflammatory process, which can occur in the outer or middle ear, in acute or chronic form, etc.
On a note!
The most difficult to diagnose is exudative otitis media, since it is practically asymptomatic, and children and parents practically do not pay attention to slight hearing loss and tinnitus.
It also causes some difficulties in identifying the disease in infants who cannot talk about their condition. Signs of otitis media in this case include moodiness and restlessness, breast refusal, constant crying for no apparent reason and hearing loss (the child does not respond to the parents’ voices or extraneous sounds). You can diagnose the disease in infants using a simple test - just lightly press on a small protrusion (tragus) next to the baby's ear. If the child cries a lot after this, it means that this movement caused an increase in pain, which is typical for otitis media.
Normal temperature indicators
What temperature a child should and can have at 4 months depends on the baby’s living conditions, type of feeding and many other factors.
Usually, up to six months, a child rarely suffers from infections caused by viruses, since social contact is limited. It is still possible to catch the disease during a routine examination by a pediatrician or if one of the family members carries the disease. The temperature varies between 36-37.5 degrees.
Indicators of normal temperature and methods of measuring it
Starting from six months, the risk of getting sick increases: complementary feeding is introduced, the baby is in active contact with other children and adults, and can catch chickenpox, rubella, and ARVI.
You should monitor the child’s condition and seek the help of a specialist if the following symptoms are detected:
- the baby is lethargic and weakened – this is a sign of the onset of an infectious disease;
- a runny nose appears, the color of the snot is yellowish-green - an allergic reaction or a cold;
- dry cough – the onset of bronchitis, pneumonia, colds or allergies;
- hoarse voice - this happens in the case of measles, tonsillitis, influenza, diphtheria, asthma, pneumonia;
- vomiting began - a consequence of food poisoning, gastrointestinal diseases, encephalitis, meningitis;
- diarrhea – the presence of an intestinal infection;
- headache – a consequence of ARVI, influenza, sinusitis, thermoneurosis, intoxication;
- abdominal pain - the onset of acute respiratory infections, poisoning, tonsillitis, whooping cough, measles, the presence of a foreign body in the stomach.
Additional Information. If a child's infectious disease is not treated, it can cause complications: pneumonia, bronchitis, tonsillitis and sinusitis. Therefore, it is important not to miss its onset, which usually manifests itself in an increase in body temperature.
Low-grade fever is normal
The normal temperature of a 4-month-old baby can be completely different at different times of the day. The most important thing is that the baby should be active, cheerful and cheerful, and have a good appetite.

If the baby is active and cheerful, there is no reason to worry
If the measurements are accurate, then if the readings are elevated, the fact of teething or vaccination that was done the day before should be excluded, since in these cases the temperature can be kept around 37.2-37.6. You should wait a while, a few days.
In addition, low-grade fever is a consequence of imperfect thermoregulation of the infant, which does not require any intervention. You should contact your pediatrician if your baby has chills, sneezing, lethargy and moodiness.
Note! Low-grade fever persists after taking antibiotics and suffering a serious illness. In this case, treatment is not necessary, but the situation should be kept under control. If a repeated runny nose or cough appears, then this may be a relapse, the appearance of a new infection.
Why does the temperature rise with otitis media?
An increase in temperature is a natural reaction of the body to inflammatory and infectious processes in the body. The numbers on the thermometer for this disease depend on the clinical course, the state of immunity and the age of the child - infants tolerate the disease much more difficult than older children.
Most often, a high temperature occurs with a purulent form of otitis, and the fever lasts until the pus comes out of the ear, on its own or after appropriate medical procedures. The duration of the hyperthermic stage can be from 3 to 7 days, after which the temperature drops to normal limits.
Another reason for the increase in temperature during otitis is complications of the disease that develop as a result of improper treatment. The most dangerous consequences of ear inflammation are mastoiditis (damage to the tissue of the mastoid process, accompanied by the development of osteomyelitis), meningitis and otogenic sepsis. The development of complications is characterized by the following clinical picture: the patient’s condition improves for several days, after which ear pain, fever and other manifestations of the disease reappear.
Can otitis media occur without fever?
Otitis is not always accompanied by an increase in temperature - there are several forms of the disease for which fever is not characteristic. Most often, this course of the disease is observed during an inflammatory process caused not by infectious infection, but by mechanical damage to the skin of the ear canal. A wound forms at the site of damage, causing a burning sensation and pain, which intensifies if microbes enter the wound, and an abscess forms in its place.
In addition, if ear pain occurs without hyperthermia and other general symptoms, a differential diagnosis of otitis should be made with otomycosis (damage to the structures of the hearing organs by fungal microorganisms), eczema of the ear canal. Fungal ear infections can be distinguished from inflammatory processes by the presence of itching, which is characteristic of fungal infections. There is no increase in temperature in diffuse external otitis and atypical course of the inflammatory process.
In what cases should you consult a doctor immediately?
Temperature with otitis media causes a lot of discomfort for both the baby and his parents. In any case, this symptom requires contacting a doctor, but in some situations the child needs medical attention immediately. You need to call an ambulance when the temperature is high:
- observed in a child under six months of age;
- is not affected by conventional antipyretic drugs;
- accompanied by dyspeptic disorders (nausea, vomiting, diarrhea) or skin rash, severe headache, weakness.
The above signs may indicate not only otitis media, but also other dangerous diseases, so it is best to consult a doctor as soon as possible.
What to do if your child has a high fever
To reduce your child's fever, you should take the following steps:
- Create comfortable conditions for the baby. The temperature and humidity in the room should be normalized. Provide regular ventilation, but without creating drafts.
- You cannot wrap your baby in warm blankets if the temperature in the room is maintained.
- Inform your local doctor that your child is sick and has a fever.
- In extreme heat, it is necessary to give the child fluids regularly: juices, compotes, water. This will eliminate the dangerous consequences of extreme heat - dehydration.
- Carry out wraps from a vinegar solution. The forehead and legs should be moistened.
- Resort to the use of antipyretic drugs: suppositories and syrups.
- If your baby begins to show signs of seizures, you should open his mouth. In case of severe convulsions, it is necessary to urgently call an ambulance.
- It is necessary to feed the baby if he has an appetite. If the child does not want to eat, then you should not stuff him. At high temperatures, symptoms of vomiting, nausea, and diarrhea may appear.
In children under one year of age, the normal temperature readings have their own characteristics. Every mother should know what the optimal body temperature is for her child. It is necessary to control not only body temperature, but also monitor the baby’s condition. And remember that the normal temperature of a child aged 5 months will never correspond strictly to one value. This is due to the physiology of the child’s body.
Treatment of otitis media with fever
It is recommended to lower the temperature only in cases where it exceeds 38-38.5, and in children suffering from convulsive syndrome, cardiovascular disorders or other concomitant diseases, the permissible figures are 37-37.5. If the fever is not too severe and the child feels well, the use of antipyretics is not recommended in order to give the body the opportunity to fight the infection on its own. In order to bring down the temperature, it is better to use drugs containing ibuprofen or paracetamol in the appropriate dosage - they will not only eliminate the fever, but also reduce pain in the ear.
The main component of the treatment of otitis accompanied by fever is antibacterial agents, which can be local (used at the site of inflammation) or systemic. In cases of mild disease - the disease is accompanied only by pain in the ears and low-grade fever - the fight against the pathological process is usually limited to the use of local drugs. If such treatments are ineffective, you should switch to systemic therapy.
For purulent otitis, the use of antibiotics (Amoxicillin, Flemoxin Solutab), which are prescribed by a doctor, is indicated. An increase in temperature during otitis plays another important role - it helps to evaluate the effectiveness of the chosen treatment regimen. With proper therapy, an improvement in condition and a decrease in temperature is observed within the first day. If the fever remains unchanged for several days, it is necessary to select other drugs. With proper treatment, catarrhal otitis takes an average of a week, purulent otitis – in two weeks.
Fever in children - causes
In most cases, fever in all people is caused by infections or viruses. We are talking about influenza, acute respiratory infections or ARVI. And in this case, you need to fight the hotbed itself. But the critical levels of the latter should also be brought down.
Although infection is what we most often blame as the cause of high fever in our children - and some of us, unfortunately, without any doctors or tests - it is not always the true cause of the fever.
Other founders of hyperthermia include:
- immunization - when a slight increase in temperature in a child is observed due to the action of such vaccines, and this is a normal process (up to certain levels of increase);
- teething may cause a slight increase in body temperature in children at the appropriate age;
- overheating or sunstroke - the first occurs more often in very young children who are not yet capable of internal thermoregulation, and the latter for children of any age and even adults.
General principles of treatment of otitis media in children
In order to get rid of the disease and its symptoms as soon as possible, it is necessary to adhere to the general rules for the treatment of ear diseases.
- Antibiotics for oral administration are prescribed exclusively by the attending physician. As a rule, therapy includes cephalosporins and penicillins, and in the presence of allergies, macrolides.
- It is not advisable to use drops containing antibiotics in the first stages of the disease - drugs with an analgesic and decongestant effect are better suited. They are used in the acute phase of the disease in the presence of perforation, as well as in cases of chronic otitis.
- In case of acute otitis media, it is recommended to instill vasoconstrictor drops for rhinitis into the child’s nasal passages, which will restore normal communication between the nasal passages and the middle ear.
- If the child does not have a fever or purulent discharge from the ears, warming compresses can be applied. They are not placed on the auricle itself, but around it - a hole is made for the ear in a piece of bandage or gauze folded several times, after which the fabric is moistened in diluted alcohol or vodka, and a compress is applied to one side of the head. It is covered with polyethylene on top, insulated with cotton wool and secured with a scarf. The duration of the procedure is at least two hours.
- You can warm sore ears using a medical reflector with a blue lamp or a bag of salt, but such activities can also be carried out only in the absence of fever and pus.
- Using traditional recipes to treat otitis in children, especially without consulting a doctor, is strictly not recommended - self-medication can complicate the course of the disease and provoke serious complications.
You should not bathe a child with otitis media - it is better to rub it with warm water. Meals should include light but nutritious meals with sufficient vitamins. Walking is allowed only after the temperature has returned to normal, and ear pain and purulent discharge have disappeared, and the baby needs to wear a hat while he is outside.
Prevention of otitis
The development of otitis media in children can be prevented with simple preventive measures. First of all, it is necessary to avoid colds and increase immunity: take vitamin complexes, eat fresh vegetables and fruits, and harden the child. If the baby does get sick with a cold or acute respiratory viral infection, treatment should be carried out in a timely manner and under the supervision of a doctor. Under no circumstances should you clean out earwax with objects not intended for this purpose - pins, matches, bobby pins. Children under three years of age require constant adult supervision - children of this age often insert foreign objects into their ears, as a result of which purulent otitis media develops.
0
Infants
What should be the temperature of babies under one year old? The average temperature up to 3 months is 37.5 degrees. These are standard indicators that are also typical for six-month-old children. At one year of age the thermometer drops to 37.1. After a year, normal body temperature is usually established - 36 and 6. However, a temperature of 37 is normal for a one-year-old child: this depends, first of all, on the individual structure of the body.
Such indicators may also be typical for children under three years of age, and this is also the norm. Until what age can a thermometer show 37? Up to 5 years, and this is also considered the norm. Low-grade fever can last up to 7 years, and nothing bothers the baby. The table of body temperature values for children gives approximate results - you should always focus on the baby’s well-being.
Note! Rectal temperature differs from readings taken in the armpit.
According to medical observations, low-grade fever is considered a normal characteristic if the body feels well. In recent decades, the norm of temperature in people has changed, and this is written about in medical articles. If previously the mark of 37 degrees caused alarm, now it is considered to be a common occurrence even among adults.











