Cow's milk protein allergy (CMP) affects 2 to 6% of children under one year of age. About 50% of children recover from ACM within the first year of life. 80-90% - within the first five years.
It should be noted that parents begin to suspect that their children have an allergy to cow's milk proteins approximately 4 times more often than it actually occurs. Thus, in many children, parents suspect ABCM based on symptoms such as skin rashes, sleep disturbances, persistent nasal congestion, seborrheic dermatitis, or positive results of nonspecific tests. In addition, parents often prescribe unnecessary diets to their children without adequate medical and dietary supervision.
These incorrect dietary restrictions can provoke nutritional imbalances, especially in the first year of a child's life. Therefore, accurate diagnosis of cow's milk protein allergy (CMAI) is important not only to avoid the risk of rickets, reduced mineralization rate, anemia, growth retardation and hypoalbuminemia, but also due to immediate clinical reactions or severe gastroenteropathy leading to malabsorption.
Allergy to cow's milk protein: when to suspect?
Children with an allergy to cow's milk proteins are characterized by a burdened atopic history.
An allergy to cow's milk should be suspected in children who experience immediate allergic reactions such as: acute urticaria/Quincke's edema, wheezing, rhinitis, dry cough, vomiting, laryngeal edema, acute asthma with severe respiratory failure, anaphylaxis.
Delayed-type allergic reactions (or so-called late allergy symptoms), which necessitate a diagnosis of ADCM, are: atopic dermatitis, chronic diarrhea, blood in the stool, iron deficiency anemia, gastroesophageal reflux disease (GERD), constipation, chronic vomiting, colic, low increase in height and weight (refusal to eat), enterocolitis syndrome, protein-losing enteropathy with hypoalbuminemia, eosinophilic esophagogastroenteropathy.
The diagnosis of “allergy to cow’s milk proteins” is based on detailed anamnestic signs (Fig. 1), the results of a skin allergy test (prick test) and the detection of serum specific IgE to cow’s milk proteins, the positive effect of the elimination diet and the reaction to a food challenge test.
The clinical manifestations of cow's milk protein allergy (CMAI) can be divided into IgE-mediated clinical reactions (symptoms appear within 30 minutes of ingestion of cow's milk) and non-IgE-mediated reactions (onset hours to days after ingestion of cow's milk). cow's milk), with a predominant reaction from the skin and gastrointestinal tract.
However, immediate and delayed allergic reactions can be combined in atopic dermatitis and eosinophilic esophagogastroenteritis. (Fig. 1) Fig. 1: Allergic reactions of immediate and delayed type in children with ABCM
Immediate allergic reactions:
| Delayed allergic reactions:
|
Treatment
If a child has an allergy to milk, only a doctor can prescribe treatment. Typically, therapy is based on the intake of sorbents. Such products free the body from allergens, which improves the baby’s condition and eliminates the symptoms of the pathology. Treatment is also prescribed depending on the area of manifestation of the disease.
Gastrointestinal system
Due to pathology, the baby often develops intestinal problems. The child begins to pull his legs towards his stomach due to pain in the abdominal area. This indicates the occurrence of dysbiosis. Probiotics help tidy up the intestinal microflora.
Parents also need to consult with a specialist on how to replace milk if you are allergic to milk protein, so that there are no problems with the gastrointestinal tract. In such a situation, doctors advise introducing fermented milk products into the baby’s diet.
Skin lesions
Epidermal therapy depends on the nature of the lesion:
- Milk scab. It is the formation of a crust on the epidermis of the child’s head. Therapy consists of regularly treating the rash with Vaseline or vegetable oil;
- Atopic dermatitis. With this pathology, plaques of different sizes appear, covered with white scales. Locations: lower and upper extremities. The rash becomes wet, and the child experiences itching in the affected area of the epidermis. Therapy is based on the use of antihistamines and treatment of the epidermis with zinc ointment;
- Hives. These are blisters that cause severe itching in the baby. Externally, the rash resembles a burn left by nettles. This is where pathology got its name. To get rid of the rash, the patient is prescribed antihistamine medications;
- Quincke's edema. This is a deadly manifestation of a milk allergy. The baby's mucous membranes in the throat and nose swell. As a result, the child begins to choke. If angioedema occurs, immediate hospitalization is required. Therapy is based on the use of hormonal medications.
Respiratory system
If the baby suffers from this pathology, then problems with the respiratory system rarely arise. If this does happen, the baby develops allergic rhinitis and wheezing. The child also finds it difficult to breathe. Lack of timely assistance can cause suffocation, so at the first signs of respiratory damage, it is recommended to call an ambulance.
Allergy to cow's milk protein: prick tests and food challenge test
Prick tests (skin tests) are one of the most accurate laboratory methods for confirming/excluding cow's milk allergy: approximately 60% of children with positive prick tests actually have an allergy to cow's milk proteins. The value of negative skin test results is considered even higher: over 95%. Additionally, a prick test with a diagnostic drug made from cow's milk replacer can be used.
However, a small proportion of children with negative results of prick tests and serum IgE still develop clinical reactions characteristic of an allergy to cow's milk proteins. Therefore, in such patients, despite a negative IgE test, if there is a strong suspicion of an allergy to cow's milk protein, it is necessary to conduct a food challenge test to prove the absence of clinical allergy.
Thus, a food challenge test, open or blind, remains the “gold standard” for verifying food allergy (including allergy to cow's milk proteins) when the diagnosis is in doubt. Food challenge testing should be carried out under medical supervision in the intensive care unit, especially in the case of a positive prick test or serum IgE to cow's milk and in infants, due to the risk of immediate allergic reactions.
Symptoms of goat milk allergy in children and adults
Parents often mistake allergic symptoms in children for diathesis, viral infection or indigestion. Symptoms most often appear before the age of three.
When introducing a new product into a small child’s diet (after all, goat’s milk is an allergen), you should pay close attention to the following symptoms:
- the appearance of rashes or hives throughout the body;
- restless sleep, excessive excitability, poor appetite;
- the appearance of redness of the eyelids, allergic conjunctivitis;
- swelling of the mucous membranes of the throat and mouth;
- flatulence, bloating;
- digestive disorders: loose stools or constipation;
- in severe cases: difficulty breathing, wheezing in the lungs, Quincke's edema.
Symptoms in an adult:
- abdominal pain, heartburn;
- attacks of nausea and vomiting;
- loose or poorly digested stools;
- skin rash localized on the bends of the limbs, abdomen, groin, and back;
- itching sensation;
- swelling and redness of the mucous membranes of the mouth, cheeks, eyes;
- hoarse and difficult breathing, rapid heartbeat, dizziness.

Hydrolyzed formulas and other milk substitutes: diet for MCM
To replace cow's milk in the diet of children with allergies to its proteins, mixtures based on hydrolyzed protein, soy, rice, and milk from other domestic animals can be used. Unfortunately, any of the listed products can also cause allergies.
Thus, about 10% of children with cow's milk protein allergy (CMPA) react to formulas prepared on the basis of hydrolyzed proteins (so-called hydrolyzed formulas).
Even more often, clinical manifestations of allergies in children under 6 months of age are caused by soy-based mixtures (in older children, the frequency of allergic reactions to hydrolyzed protein and soy proteins is comparable). Soy mixtures provoke mainly gastrointestinal symptoms.
Rice is also a fairly allergenic product and, according to available data from Australian researchers, often provokes enterocolitic syndrome in Australian infants. In addition to Australia, rice-based formulas were also used in Italy for feeding children with cow's milk allergies. Extensive long-term studies promise to bring final clarity to the question of whether rice-based formulas can be used for allergies to cow's milk as a complete alternative to this product. Today it is believed that rice mixtures can be used in individual cases, taking into account the taste and cost of the mixture.
The milk of other mammals is not nutritionally adequate. In particular, goat's milk causes clinical reactions in more than 90% of children with an allergy to cow's milk proteins. Donkey milk - 15%, and has a high cost.
Home-cooked food as an alternative to milk can be allowed for children from 4 months.
Special mention should be made of mixtures based on amino acids. Amino acid-based mixtures do not cause allergies, however, their use is limited due to high cost and extremely specific taste.
Nutritional Features
What to feed a child with a milk allergy? There are special mixtures that will replace this product. The hypoallergenic food mixture can be replaced with fermented milk products. Special age-appropriate products have been developed for children - kefir, yoghurt and others. For a child over 1 month old, the daily dose is calculated by a specialist.
During the diet, cow's milk should be excluded from the diet. It can be replaced with goat's milk. For better absorption of the product, it is recommended not to give it in its pure form, but to add it to tea. If a child is allergic to goat's milk, then it should be excluded.
It is impossible to structure the diet of children in such a way that it does not contain dairy products. Animal milk can be replaced with plant milk - oatmeal, soy, rice.
It is recommended to start consuming dairy products after three to five years of age. By this time, the child’s fermented and immune system matures and the body begins to accept milk protein normally. There is no need for a child to adhere to a special nutritional system all his life.
Algorithm for diagnosis and treatment for suspected allergy to cow's milk proteins
If an allergy to cow's milk proteins is suspected, pediatricians and parents are forced to solve the problem of not only confirming/excluding this diagnosis, but also the further feeding of the child. To facilitate this task, the Emilia-Romagna group proposed three different algorithms for diagnosis and further management of patients, according to the symptoms and type of infant diet. They are shown in Fig. 2,3,4
These approaches apply to children in the first year of life.
Children with mild or moderate signs of allergies (fed with cow's milk-based formulas)
Rice. 2. Children with mild or moderate signs of allergies (fed formulas based on cow's milk)
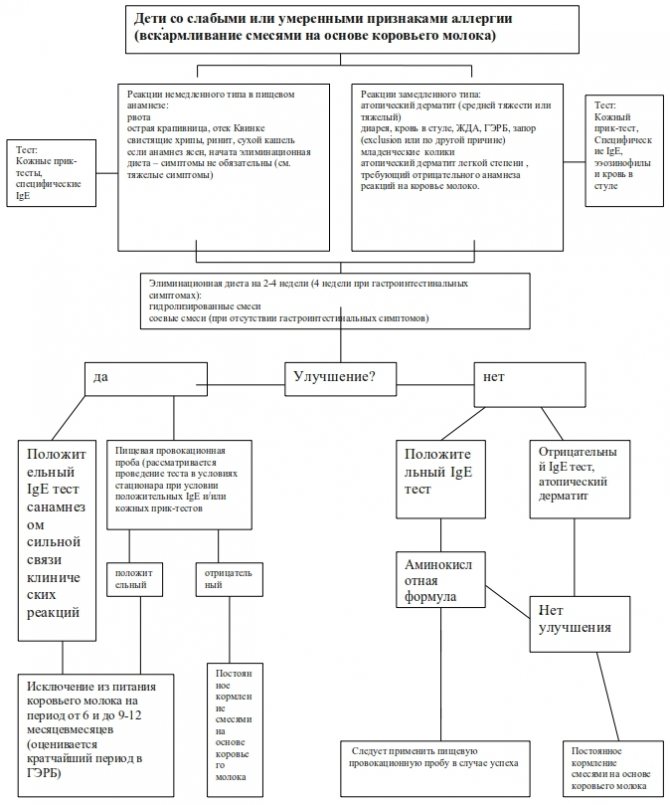
Algorithm for diagnosis and treatment for suspected allergy to cow's milk proteins: explanation for Fig. 2
The pediatrician should suspect an allergy to cow's milk proteins on a free diet only in the most severe cases. Mild allergic reactions can be difficult to interpret because they may result from causes unrelated to cow's milk protein allergy.
If the onset of gastrointestinal symptoms is relatively late, other pathologies (ie, infections) should be excluded before testing for allergic reactions is started. In moderate atopic dermatitis, suspicion of cow's milk protein allergy is not warranted unless there is a clear relationship between cow's milk consumption and the onset of symptoms. However, if any of the symptoms listed are clearly associated with cow's milk-based formula, it is recommended to eliminate cow's milk from the diet and follow the procedure for severe reactions (Fig. 3)
In infants with symptoms of allergic reactions of immediate type (vomiting, angioedema, wheezing, rhinitis, dry cough) or delayed type (moderate/severe atopic dermatitis, diarrhea, blood in stool, iron deficiency anemia (IDA), gastroesophageal reflux disease (GERD) , constipation), an allergy to cow's milk protein may be suspected. Additionally, this diagnosis should be considered in infants who are refractory to therapy.
If an allergy to cow's milk proteins is suspected, the infant is prescribed an elimination diet for 2-4 weeks, excluding cow's milk protein (for 4 weeks - in the presence of gastrointestinal signs). Infants should be fed hydrolyzed formula or soy formula (the latter recommendation is for children over 6 months of age in the absence of gastrointestinal symptoms).
If allergy symptoms subside, a food challenge test (FPT) with cow's milk proteins is necessary to verify the diagnosis. If the PPP is positive, the child must follow an elimination diet, after which the test can be repeated after 6 months (with GERD - a shorter period), and in any case, after 9-12 months of age. If the food challenge test is negative, a free diet is prescribed.
If there is a high likelihood of developing immediate IgE-mediated reactions in infants who do not respond to hydrolyzed protein formulas (hydrolyzed formulas) or soy, a food challenge may be performed after a 14-day amino acid formula diet.
Cow's milk replacers are used in children under 12 months of age. In older children with an allergy to cow's milk proteins, given the availability of an adequate diet, hydrolyzed protein or amino acid formulas are rarely required.
Infantile colic (more than 3 hours of crying per day, 3 days for three weeks) is definitely not considered a consequence of an allergy to cow's milk.
Children with severe allergy to cow's milk protein (fed with cow's milk-based formulas)
Rice. 3. Children with severe allergy to cow's milk protein (fed with cow's milk-based formulas)
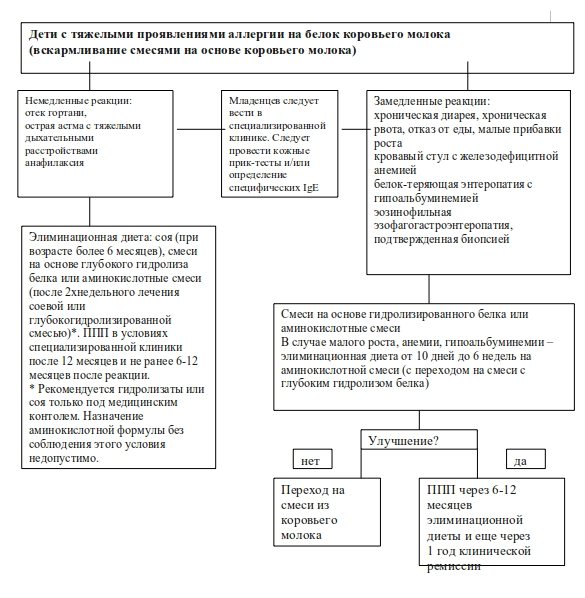
Algorithm for diagnosis and treatment for confirmed allergy to cow's milk proteins: explanations for Fig. 3
Immediate allergic reactions include: swelling of the larynx, acute shortness of breath with severe respiratory failure, anaphylaxis.
Delayed allergic reactions: chronic diarrhea or chronic vomiting with short stature, intestinal bleeding with iron deficiency anemia (IDA), protein-losing enteropathy with hypoalbuminemia, biopsy-proven eosinophilic gastroenteropathy.
If any of these symptoms occur due to a suspected allergy to cow's milk proteins, the infant is placed on an elimination diet to exclude milk. Soy formula (in children over 6 months), hydrolyzed formula or amino acid mixture can be used as a replacement. Initiation of treatment with hydrolyzed or soy formulas should be under medical supervision due to possible clinical reactions. If an amino acid-based formula is used, it should be used for 2 weeks, after which the infant should be switched to a soy or hydrolyzed formula.
In children with late-onset severe signs of gastrointestinal distress, low height/weight, anemia, hypoalbuminemia, or eosinophilic esophagogastroenteropathy, it is recommended that an elimination diet be started with an amino acid formula and then switched to a hydrolyzed formula. The effect of the diet should be tested within 10 days for enterocolitis syndrome, 1-3 weeks for enteropathy and 6 weeks for eosinophilic esophagogastroenteropathy.
In children with anaphylaxis and confirmed positive IgE tests or severe gastrointestinal reactions, a food challenge test is not needed to verify the diagnosis. It should be performed no earlier than 6-12 months from the last reaction. Children should follow an elimination diet until 12 months of age, and in case of enterocolitis syndrome - until 2-3 years of age.
Children with severe allergic symptoms of any type should be hospitalized in a specialized hospital.
Hydrolyzed protein formula or amino acid formula is used in children under 12 months of age and in older children with gastrointestinal symptoms. In children over 12 months of age with anaphylaxis, the need to use cow's milk substitutes in their diet does not always arise.
Why does intolerance occur?
Dairy intolerance can occur for two reasons:
- allergic reactions
- the body's inability to digest lactose.
Many people who do not have enough knowledge in medicine consider this to be the same phenomenon, although this is not entirely true.
Lactose can cause allergic reactions, but this does not mean that the body cannot absorb it.
In most cases, an allergy to goat's milk in a child is associated with the intake of the milk protein casein, the molecules of which can trigger the development of sensitization.
This causes the production of antibodies that contribute to the allergic reaction.
The reason for its occurrence in children may be as follows:
- heredity;
- early introduction of goat and cow milk into the child’s diet;
- non-compliance with the diet by the mother during lactation (consumption of foods with a high content of allergens).
Lactose intolerance is caused by a low level of lactase, the enzyme that is responsible for its breakdown in the body.
Undigested lactose accumulates in the intestines, causing gastrointestinal disorders.
Find out how to treat shortness of breath due to allergies. What should be the diet for allergies in adults? The answer is in this article.
Breastfed child with suspected cow's milk protein allergy
(Fig. 4) Algorithm of action in case of suspected non-IgE mediated reaction to cow's milk proteins in relation to breastfed children
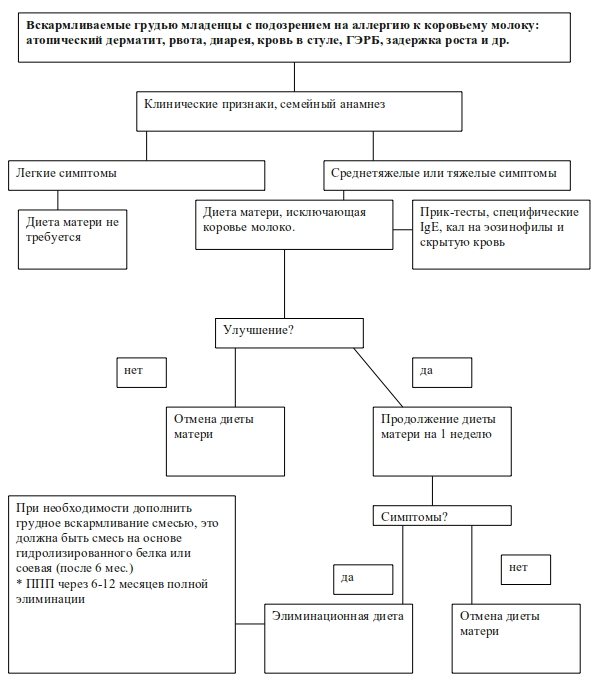
Algorithm for diagnosis and treatment of breastfed children with suspected allergy to cow's milk proteins: explanation for Fig. 4
In children who are fully breastfed, symptoms of allergy to cow's milk proteins (atopic dermatitis, vomiting, diarrhea, blood in the stool, GERD, etc.) are almost always not IgE mediated. Therefore, if the symptoms of these disorders are moderate, it is not recommended to exclude milk from the mother's diet. To date, there is no evidence of the importance of eliminating eggs or cow's milk from the mother's diet, for example, in infants with blood in the stool (proctocolitis).
Cow's milk protein, eggs and other foods should be eliminated from the diet of mothers whose children have moderate symptoms only if a clear clinical response is noted. In addition, the baby must be hospitalized in a specialized hospital. The maternal elimination diet should last for 4 weeks. If there is no improvement, the diet should be stopped. If the symptoms have decreased, it is recommended that the mother take large amounts of cow's milk for 1 week. If symptoms return, the mother should continue the elimination diet with additional calcium intake.
The infant can be weaned according to the same recommendations as healthy children, but cow's milk should be avoided until 9-12 months of age, and for at least 6 months after starting the diet.
If the volume of breast milk is insufficient, then a formula based on hydrolyzed proteins or a soy-based formula (after 6 months of age) is used for supplementary feeding. If, after the mother restarts taking cow's milk, the symptoms do not worsen, the excluded foods can be gradually introduced into the diet one by one.
Diagnosis of milk allergy
You should not diagnose your child yourself. You need to see a doctor who will diagnose and prescribe treatment for allergies. First, the doctor will examine the child and then prescribe tests:
- urine;
- feces;
- blood.
The specialist will also send you to take skin tests to rule out similar diseases. By the way, an allergy test is especially important, which allows you to identify immunoglobulin E to milk protein.

Sometimes allergies are diagnosed by excluding certain foods from the child's diet. If, after their gradual introduction, symptoms begin to appear, then it is possible to understand what exactly causes the body’s inadequate reaction.
Allergy to cow's milk protein in children: summary
- The definitive diagnosis of cow's milk protein allergy is based on a food challenge test, which is carried out after an elimination diet lasting 2-4 weeks.
- A diagnostic food challenge test (DFT) is not performed for immediate-type allergic reactions or delayed-type allergic reactions (gastrointestinal symptoms with anemia, decreased height gain, or hypoalbuminemia) if the causative role of cow's milk is obvious. If it is necessary to conduct a food challenge test, it can be performed no earlier than 6-12 months after the reaction and no earlier than 12-24 months of life, depending on the symptoms.
- Diets prescribed in baby food (including maternal diets during breastfeeding) must be balanced. Children with an allergy to cow's milk protein are additionally prescribed calcium.
- Children with mild atopic dermatitis and a negative history of reactions to cow's milk do not require a diet.
- Soy formula should not be used in infants younger than 6 months with allergic symptoms and in older infants with gastrointestinal symptoms.
- Children with gastrointestinal symptoms and anemia, short stature and hypoalbuminemia should receive amino acid-based formulas, followed by a transition to hydrolyzed formulas.
- Formulas based on hydrolyzed proteins and mixtures based on amino acids are used in children under 12 months of age, as well as in older children with severe gastrointestinal symptoms.
- Children over 12 months of age with anaphylaxis do not always need to use cow's milk substitutes.
The author of the translation is pediatrician Butriy Sergey Alexandrovich
How to properly introduce it into a child’s diet
Before you start feeding your baby the product, you should know whether there may be an allergy to goat’s milk and take into account the recommendations of specialists, which include the following:
- Buy natural products only from trusted sellers who can confirm the conditions under which the animal is kept.
- If you can only buy it at the market, then you should ask the merchant for a certificate from a veterinarian, which confirms that the goat is healthy.
- When buying in a supermarket, pay attention to the production date and expiration date.
Before introducing goat's milk into a baby's complementary diet, the liquid should be diluted with water approximately one to three, since it is very fatty. Otherwise, there is a high chance that your baby will have problems with bowel movements.
If there are no negative manifestations, then after 2 weeks you can dilute it in a ratio of one to two. Thus, after a month the child can drink pure, undiluted milk.
Children under three years of age and newborns should drink only boiled product, while older children can drink it raw.
As for storage, you should choose enamel, ceramic or glassware, since it quickly deteriorates in other containers.