Scarlet fever is an acute infectious disease with a characteristic rash, purulent-septic and allergic complications, as well as a disease of the larynx caused by streptococcus. Those who have had scarlet fever retain strong immunity to it.
When the manifestation of other symptoms is unclear, scarlet fever is often mistaken for a sore throat, and yet a patient with such a course of the disease is especially dangerous as a source of infection. Children aged 1 to 9 years are most often affected. The incidence increases in autumn and winter. Scarlet fever is much more dangerous than measles. During severe epidemics, without medical assistance, a large number of deaths are possible.
Scarlet fever is characterized by general intoxication, fever, inflammation of the tonsils, and pinpoint rashes throughout the body.
Scarlet fever has been known since ancient times. The name of the disease “scarlet fever” comes from the Latin word “scarlatum”, which means “bright red”. The disease received this name, obviously, because of its characteristic bright red rashes on the skin and mucous membranes.
This is an acute airborne infection that primarily affects children under 10 years of age; characterized by fever, general intoxication, sore throat and pinpoint rash. The incidence increases in the autumn and winter months.
Cause of infection. The causative agent of the disease is beta-hemolytic toxigenic group A streptococcus, which colonizes the nasopharynx and, less commonly, the skin, causing local inflammatory changes (sore throat, swollen lymph nodes). The exotoxin produced by streptococcus causes symptoms of general intoxication and exanthema (rash).
Where can a child become infected with scarlet fever?
Scarlet fever is a highly contagious infection. Children 2-7 years old most often suffer from scarlet fever. Newborns (thanks to maternal immunity) rarely get scarlet fever. In adults, scarlet fever is milder than in children. Children become infected with scarlet fever mainly in kindergartens or schools. Several types of transmission of the scarlet fever pathogen are known: airborne (with inhaled air), contact (through contaminated things, toys), food (if food products, for example, milk, are contaminated with an aggressive microbe). Cases of scarlet fever localized to wounds are extremely rarely reported. In such cases, streptococcus settles and develops directly on the wound surfaces. In an epidemiological sense, however, the most important are the first two types of transmission of the scarlet fever pathogen, which contribute to the occurrence of scarlet fever epidemics in schools and preschool institutions.
Infection in children spreads primarily through airborne droplets, with the source being a sick person or a bacteria carrier. Less common are contact and household transmission (both direct and indirect contacts - through toys, care items, etc.) and food transmission - through infected products. The child is contagious from the 1st to the 22nd day of illness. Most often, scarlet fever occurs in the autumn-winter period.
The incubation period lasts 5-7 days (minimum several hours, maximum period up to 12 days). The latent period of scarlet fever lasts from 3 to 7 days. The disease begins acutely with a sharp disturbance in the child’s well-being: he becomes lethargic, drowsy, and complains of severe headache and chills. Body temperature quickly reaches high numbers (38-40 °C depending on the severity of the disease). Nausea and vomiting are often observed in the initial stages of the disease.
After a few hours, a specific rash appears on the child’s skin in the form of small bright pink dots on reddened skin. The rash is more pronounced on the face, lateral surfaces of the body and in places of natural skin folds (inguinal, axillary, buttock). A characteristic sign of scarlet fever is the sharp contrast between bright red “flaming” cheeks and a pale nasolabial triangle, on the skin of which there are no elements of the rash. The child’s appearance also attracts attention: in addition to the color contrast, his face is puffy, his eyes sparkle feverishly.
A typical and constant symptom is tonsillitis, characterized by bright redness of the soft palate, enlarged tonsils, in the lacunae or on the surface of which plaque is often found. The upper cervical lymph nodes are enlarged and painful. The rash stays on the skin for 3-7 days, after which it disappears, leaving no pigmentation behind. After 1-2 weeks, peeling begins, first on more delicate areas of the skin (neck, axillary folds, etc.), and then over the entire surface of the body. Scarlet fever is characterized by peeling on the palms and soles, which starts from the free edge of the nails and spreads along the fingers directly to the palms and soles, where the skin comes off in layers.
The tongue is initially coated, from the 2-3rd day it clears and by the 4th day it takes on a characteristic appearance: bright red color, sharply protruding papillae (“crimson” tongue). In the presence of severe intoxication, damage to the central nervous system is observed (excitement, delirium, blackout). At the beginning of the disease, there are symptoms of increased tone of the sympathetic, and from the 4-5th day - of the parasympathetic nervous system.
The disease can occur in mild, moderate and severe forms, depending on which the recovery time varies significantly (up to 3 weeks). Usually, the use of antibiotics allows for a faster recovery of the child’s health, and scarlet fever no longer poses a threat to his life. Complications of the disease are currently caused mainly by allergization of the body by beta-hemolytic streptococcus of group A, therefore they are noted in the 2nd week of the disease in the form of damage to the kidneys and heart. They usually occur in older children.
In mild forms of scarlet fever, intoxication is mild, fever and all other manifestations of the disease disappear by the 4-5th day; This is the most common variant of the modern course of scarlet fever. The moderate form is characterized by greater severity of all symptoms, including intoxication; the febrile period lasts 5-7 days. The severe form, currently very rare, occurs in two main variants: toxic scarlet fever with pronounced symptoms of intoxication (high fever, symptoms of central nervous system damage - blackouts, delirium, and in young children convulsions, meningeal signs), all symptoms from the pharynx and skin are clearly defined; severe septic scarlet fever with necrotizing tonsillitis, violent reaction of regional lymph nodes and frequent septic complications; necrosis in the pharynx can be located not only on the tonsils, but also on the mucous membrane of the soft palate and pharynx.
Complications: glomerulonephritis (mainly in the 3rd week), synovitis, the so-called infectious heart, less often myocarditis. Pneumonia is possible. Recurrences of scarlet fever and relapses of tonsillitis are associated with streptococcal reinfection. In recent decades, the incidence of complications has decreased sharply. After scarlet fever, lifelong immunity is usually maintained.
Diagnosis of scarlet fever in children
The clinical manifestations of a child suffering from scarlet fever must be differentiated from the manifestations of other infectious pathologies that primarily affect the children's population, for example, measles, rubella, pseudotuberculosis, and drug-induced dermatitis. In a situation where a child develops atypical signs of scarlet fever, for example, the presence of fibrinous plaque on the tonsils, it is necessary to exclude diphtheria.
The fundamental differences between exanthema in measles are the accompanying pronounced catarrhal symptom complex, the presence of enanthema and the staged appearance of rash elements, which is not typical for scarlet fever in children. For rubella, unlike scarlet fever, the appearance of intoxication syndrome in the patient is uncharacteristic, and the elements of the rash are always located on an unchanged background with a predominant localization on the extensor surfaces.
A drug-induced allergic rash in a child, unlike scarlet fever, is located mainly on the anterior abdominal wall and thighs, and is also characterized by polymorphism (petechiae, papules and urticarial elements appear at the same time). In addition, with allergic exanthema, there are no other clinical signs characteristic of scarlet fever in the form of sore throat, lymphadenitis, or intoxication symptom complex.
Pseudotuberculosis, unlike scarlet fever in children, is accompanied by the appearance of signs of intestinal dysfunction, severe abdominal pain and arthralgia. In addition, pseudotuberculous exanthema has a pathognomonic localization in the distal parts of the upper and lower extremities, which is not typical for scarlet fever in children.
Among the nonspecific laboratory signs of scarlet fever in children, the appearance of neutrophilic leukocytosis with leukocyte shifts to the left, increased ESR, which is a reflection of the severity of intoxication syndrome, should be noted.
In a standard laboratory, it is possible to inoculate the patient’s biological material on a special medium (blood agar), and reliable signs of scarlet fever in this situation will be the appearance of abundant growth of beta-hemolytic streptococcus. Throat swabs can be used as such biological material.
As an express method, which is used in diagnostically difficult situations, RCA should be used, the principle of which is to determine the antigen of the pathogen.
Causes of scarlet fever
Scarlet fever is caused by the bacterium streptococcus, which produces an erythrogenic toxin.
The infection is transmitted from a sick person to a healthy person through small splashes of saliva when talking, coughing, sneezing, as well as through a third party (a person who has come into contact with the patient) and through objects (toys, dishes, etc.). The patient is contagious throughout the entire period of the illness, and can also be a carrier of the bacilli for another 1 month after the illness or more, especially if his nasopharynx and pharynx are inflamed or he suffers from complications with purulent discharge.
Children who have not had scarlet fever, but have been in contact with a sick person, are not allowed into preschool institutions and the first two grades of school for 7 days from the moment the patient is isolated.
Sources of infection can be both patients with scarlet fever and patients with tonsillitis.
Infection with bacteria occurs through airborne droplets.
Symptoms of scarlet fever
The incubation period lasts on average 5-7 days (up to 12 days). The disease begins acutely. Body temperature rises to 39-40°C and higher, severe malaise, headache, pain when swallowing, often vomiting, sometimes delirium and convulsions appear. There is a burning sensation in the throat and it is difficult to swallow. The glands under the lower jaw become swollen, it hurts to open the mouth.
A typical and constant symptom is tonsillitis, characterized by a bright red color of the soft palate, enlarged tonsils, in the lacunae or on the surface of which plaque is often found. The upper cervical lymph nodes are enlarged and painful. Vomiting often occurs, sometimes repeatedly. There may be abdominal pain similar to appendicitis.
On the 1st, less often on the 2nd day, a bright pink or red pinpoint rash appears on the skin of the entire body in the form of overlapping red spots 1-2 mm in size protruding above the surface of the skin, which quickly grows throughout the body, resembling red goose bumps. The rashes are most intense in the area of the skin folds of the elbows and armpits. Scarlet fever is often accompanied by itching. The nasolabial triangle remains pale.
The face of the sick person is very different: a pink rash is on the forehead and temples, a bright blush appears on the cheeks, and the nose, upper lip and chin turn pale. When the nasolabial triangle is pale, the lips become brighter. The uvula, palatine arches, tonsils and palate turn bright red. Pustules or small areas of pus accumulation sometimes appear on the tonsils.
Scarlet fever is characterized by the proliferation and soreness of compacted maxillary lymph nodes; they are enlarged in size, elastic, and not connected to each other and the skin.
The rash lasts from 2 to 5 days, and then turns pale, while the body temperature drops. In the second week of illness, peeling of the skin appears. The tongue is initially coated, from the 2-3rd day it clears and by the 4th day it takes on a characteristic appearance: a bright red color, sharply protruding papillae (“crimson” tongue).
From the fifth to sixth day of the disease, peeling of the skin appears at the site of the rash, which lasts 2-3 weeks. Complications in the form of purulent inflammation of various organs are possible. After suffering from scarlet fever, some patients develop rheumatism.
The symptoms of scarlet fever largely coincide with the symptoms of a sore throat, so an accurate diagnosis is not always possible and an infected person can become a carrier of the virus.
Symptoms and signs of scarlet fever in children
The period of incubation of the pathogen in the body during scarlet fever can vary widely and range from 1 to 10 days. The classic course of scarlet fever in children involves an acute onset of clinical manifestations, which begins with severe fever. The temperature during scarlet fever in a child, as a rule, rises sharply to hectic numbers and is accompanied by the development of a pronounced intoxication symptom complex in the form of malaise, headache, severe weakness, tachycardia, and sometimes moderate abdominal pain syndrome. A high temperature during scarlet fever in a child of a younger age group is accompanied by the development of pronounced psychomotor agitation, euphoria, and in some patients, on the contrary, it provokes the development of lethargy, apathy and drowsiness. At the peak of the intoxication syndrome, a child may experience a single vomiting.
The second most common pathognomonic clinical symptom of scarlet fever in children is pain when swallowing in the throat and at the root of the tongue. A child's tongue with scarlet fever acquires characteristic pathological changes in the form of severe diffuse hyperemia, spreading to the tonsils, arches, soft palate and the back wall of the pharynx. Some patients develop an atypical course of scarlet fever, manifested by the formation of signs of follicular-lacunar tonsillitis, in which there is a sharp increase and hyperemia of the tonsils and the appearance of mucopurulent, fibrinous and even necrotic plaques of a focal nature.
Inflammatory changes in the pharynx during scarlet fever are accompanied by the development of regional lymphadenitis, in which there is an increase, thickening and tenderness of the anterior cervical lymph nodes. The tongue of a child with scarlet fever at the onset of the disease is covered with a grayish-white coating, and after a few days it is cleared and the appearance of a change in its color to crimson, as well as hypertrophied papillae on its surface. The intoxicating effect of scarlet fever on the child's cardiovascular system is manifested by tachycardia with moderate arterial hypertension.
A rash with scarlet fever in children appears only on the second day of the disease, and the elements of exanthema are located, as a rule, on a hyperemic background, which is a pathognomonic clinical marker. Initially, a pinpoint rash with scarlet fever in children is localized on the skin of the face and neck, as well as the upper half of the body, after which further spread of the rash elements is observed on the flexor surfaces of the arms, the anterior abdominal wall and the inner surfaces of the thighs. The appearance of a scarlet fever rash is accompanied by the development of distinct white dermographism.
Another feature of exanthema with scarlet fever in children is the tendency to thicken the elements of the rash, which is manifested by the appearance of dark red stripes in the projection of skin folds. Some patients experience the appearance of abundant small pinpoint elements of a confluent rash in the form of continuous erythema. A typical localization of exanthema in scarlet fever is the skin of the cheeks and forehead. When short-term compression of the skin is performed at the location of the exanthema, a temporary disappearance of the rash elements is noted.
As a result of the toxic effect of the pathogen on the vascular wall of the microvasculature, increased fragility of blood vessels develops, the manifestation of which is the appearance of pinpoint hemorrhages on the skin. Objective signs in this situation are the appearance of positive endothelial symptoms of a tourniquet and elastic band. When examining a child suffering from scarlet fever, it should be borne in mind that the rash may be completely absent or appear minimally.
On the fifth day of scarlet fever, a clinical improvement in well-being is noted, primarily manifested by relief of fever. The elements of the exanthema first become less hyperemic, and by the end of the second week there is a complete disappearance of the rash, in place of which fine-scaly peeling of the skin remains for a long time. The intensity of the manifestation of exanthema, as well as the timing of its complete disappearance, can vary within significant limits, which determines the severity of scarlet fever in a child. Thus, a mild course of scarlet fever in children is accompanied by the appearance of a scanty rash, the disappearance of which may occur within a few hours after its appearance. The intensity of peeling of the skin after regression of the exanthema directly depends on the intensity of the preceding elements of the rash.
In the extrabuccal clinical form of scarlet fever in children, the gateway for infection is damage to the skin in the form of burns, wounds, and foci of streptoderma. The rash gradually spreads peripherally from the site of initial introduction of the pathogen. With extrabuccal scarlet fever in children, under no circumstances is damage to the mucous membranes of the oropharynx and regional lymphatic collectors observed.
Erased clinical forms of scarlet fever in children practically do not occur and are manifested by a weakly expressed general toxic symptom complex, catarrhal changes in the oropharynx, and the presence of a scanty exanthema of short duration.
The toxic-septic form of scarlet fever in children belongs to the category of a rare infectious pathology and is characterized by an acute onset and a lightning-fast increase in clinical symptoms with the development of cardiovascular failure, clinically manifested by dull heart sounds, a drop in blood pressure, a thready pulse, coldness and severe pallor of the skin on the extremities . This form of scarlet fever is characterized by an extremely severe course and a tendency to develop complications of an infectious-allergic nature with damage to the heart, large joints and kidneys, and in the case of septic spread of the infectious substrate, the development of specific lymphadenitis, necrotizing tonsillitis, and otitis is noted.
a child has scarlet fever: photo of the throat
Treatment of scarlet fever
Treatment for scarlet fever is usually carried out at home, in the same way as for people with tonsillitis. Patients with severe and moderate forms of the disease, as well as patients whose family includes children from three months to seven years and students in the first two grades who have not had scarlet fever, are subject to hospitalization. Also, a person sick with scarlet fever must be isolated in a separate room; he must be provided with separate tableware, a towel and a set of bed linen.
Isolation of the sick person stops after complete recovery, but not earlier than ten days from the onset of the disease. Children who have had scarlet fever can visit preschool institutions and the first 2 grades of schools after additional isolation at home for twelve days after complete recovery.
Children who attend preschool institutions and the first 2 grades of school, who have not had scarlet fever and who have been in contact with a sick person, are not allowed into public places for seven days from the moment the sick person is isolated, and in the case of communication with an infected person during the entire period of the disease, are not allowed into the team for 17 days from the start of contact.
Traditional methods of treating scarlet fever in a child.
Bed rest for 7-10 days, taking antibiotics.
Patients with severe and complicated forms of scarlet fever are hospitalized; treatment is mainly carried out at home. Bed rest for 5-6 days (or more in severe cases). Throughout this time, treatment with antibiotics is carried out.
The need for inpatient treatment is determined by the doctor. Children with severe scarlet fever, as well as children from closed children's groups (if it is impossible to isolate them at home), are subject to mandatory hospitalization. For mild to moderate cases of the disease, treatment can be carried out at home. In order to prevent the development of complications throughout the entire period of the rash and another 3-5 days later, the child needs strict bed rest.
The diet should be gentle - all dishes are served pureed and boiled, liquid or semi-liquid, thermal irritation is excluded (neither hot nor cold is allowed, all food is served only warm). The child needs to drink more to remove toxins from the body. After acute symptoms subside, a gradual transition to normal nutrition is made.
Antibiotics play a leading role in the treatment of scarlet fever. Until now, streptococci remain sensitive to drugs of the penicillin group, which are prescribed in tablet forms at home, and in the hospital - in the form of injections according to age-specific dosages. If a child has intolerance to penicillin antibiotics, erythromycin is the drug of choice.
In addition to antibiotics, antiallergic drugs (suprasin, fenkarol, tavegil, etc.), calcium supplements (gluconate), and vitamin C in appropriate doses are prescribed. Locally, for the treatment of sore throat, rinsing with warm solutions of furatsilin (1: 5000), dioxidin (72%), infusions of chamomile, calendula, and sage is used.
The prognosis is favorable.
Does everyone get scarlet fever? Susceptibility to scarlet fever among children aged 2 to 7 years is about 40%. Adults and newborns, as mentioned above, get scarlet fever extremely rarely. The chances of getting scarlet fever are highest in children with reduced immunity, lack of vitamins, anemia (anemia), as well as in children exposed to stress and excessive stress (physical or mental). From here we immediately deduce the most effective measure for preventing scarlet fever - ensuring a balanced diet and proper rest for the child.
Is it possible to get scarlet fever again? After suffering from scarlet fever, a strong immunity usually develops, which makes the child immune to toxins (poison produced by a microbe). Recurrence of scarlet fever is very rare, but there remains a risk of developing other forms of streptococcal infections (otitis media, erysipelas, tonsillitis).
Tips for treating scarlet fever
Treatment with antibiotics is mandatory. The following tips will help relieve symptoms and alleviate your child’s condition.
- Give your child warm linden tea to drink.
- For a sore throat, place a warm compress on your neck. You can often rinse your mouth and throat with warm sage infusion.
- If your eyes are inflamed, apply a cold lotion constantly.
- If you have cramps, headaches, or lightheadedness, put a cool lotion on your head and pour cold water over it.
- If possible, give a laxative and a warm bath.
- For piercing in the ears, put a cotton swab soaked in vodka in the ear. You can moisten cotton wool with warm olive or some other vegetable oil. You can also use camphor oil, but it must be used carefully, since after using camphor it is easy to get a cold in the ear.
Folk remedies for scarlet fever
- Bedrenets saxifrage. One tablespoon of roots per 500 ml of water. Cook for 10-15 minutes. on low heat. Infuse, wrapped, for 4 hours, strain. Take 1/3-1/2 cup 3-4 times a day.
- Valerian officinalis. One tablespoon of dry rhizomes per 1 glass of cold boiled water. Infuse in a closed container for 12 hours, strain. Take 1 tablespoon 3-4 times a day before meals. Take powder from the roots for scarlet fever, 1-2 g per dose, no more than 3-4 g per day.
- Parsley. Brew one teaspoon of crushed roots with 1 glass of boiling water, take 1 tablespoon 3-4 times a day for scarlet fever.
- Mixture. Take 1 glass of lemon, cranberry or, better yet, lingonberry juice, heat and drink in small sips. Gargle with a second glass of warm juice every half hour. Pour 1 glass of alcohol into the squeeze, apply a compress to the throat.
- For scarlet fever, rinse your mouth and throat with an infusion of sage herb: pour 1 tablespoon of the herb into 1 glass of boiling water, leave, strain.
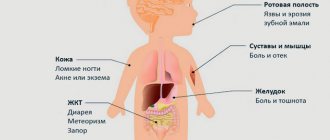
Complications and consequences of scarlet fever in children
In most situations, scarlet fever in children proceeds favorably, and a complicated course develops only in the hypertoxic form of the disease. When treating a child suffering from scarlet fever, the doctor should take into account that this pathology can be complicated both in the active clinical period and in the phase of distant convalescence.
Early complicated course of scarlet fever in children develops mainly with the spread of an infectious pathological process with the development of paraamygdal abscess, otitis media, acute pharyngitis, catarrhal and purulent sinusitis. A severe clinical form of scarlet fever in a child can act as a provocateur for the formation of secondary distant foci of inflammation, for example, in the parenchyma of the liver or kidney.
The toxic complicated effect of scarlet fever appears primarily on the functioning of the structures of the cardiovascular and urinary systems. Thus, on the seventh day of the disease there is a maximum risk of developing the so-called “toxic heart”, which is manifested by cardiomegaly, bradycardia and arterial hypotension. The characteristic complaints of a child in this situation are chest pain and progressive shortness of breath.
As a result of the action of the allergic factor in scarlet fever, complications develop in children in the form of transient damage to the kidneys, as well as the bloodstream. The damaging effect on blood vessels during scarlet fever is accompanied by bleeding in various internal organs, among which the greatest danger is intracerebral bleeding.
The development of late complications with scarlet fever in children is also in most cases due to the influence of long-term allergic mechanisms. The result of such aggressive sensitization of the child’s body is the development of a damaging effect on the body’s own tissues. The most common late allergic complication of scarlet fever in children is articular rheumatism, the symptoms of which develop two weeks after streptococcal tonsillitis. A manifestation of this late complication is pain in large joints, as well as in small groups of joints of the upper extremities. A characteristic pathognomonic criterion in this situation is the movement of the affected pathological changes from one joint to another. Changes in the joints after scarlet fever are accompanied by severe pain, local hyperemia of the skin, and a limited increase in skin temperature. Fortunately, this articular form of scarlet fever is short-lived and goes away without leaving a trace.
The development of valvular heart disease in scarlet fever also falls into the category of late allergic complication of the disease, which, unfortunately, is irreversible and requires surgical correction. Pathomorphological changes in the valve apparatus consist of thickening and rupture of the leaflets of various heart valves. The result of such valvular heart disease in scarlet fever is a violation of blood transfusion with the further development of heart failure.
Another complication of scarlet fever in children is the development of streptococcal glomerulonephritis, manifested by pain in the lumbar region, decreased diuresis, and nephrotic syndrome, which are reversible and extremely rarely provoke the development of renal failure.
The damaging effect of scarlet fever in children on the structures of the central nervous system is Sydenham's chorea, the development of which is usually observed in the third week after clinical recovery. Clinical signs of this variant of scarlet fever complication are the appearance of psychomotor agitation, impairment of cognitive functions and emotional state of the child. A pathognomonic clinical marker of Sydenham's chorea is the development of uncontrolled movements in the limbs, which become uncoordinated, unrhythmic, and erratic. Simultaneously with these signs, the child may exhibit speech impairment. The above clinical manifestations in most situations are short-term and reversible.
Most often, the development of a complicated course of scarlet fever is observed in the absence of timely drug correction of the disease or the selection of an inadequate treatment regimen.
Prevention of scarlet fever.
The patient is isolated at home or (if indicated) hospitalized. The wards in the hospital are filled simultaneously within 1-2 days, excluding contacts of those recovering with patients in the acute period of scarlet fever. Convalescents (recovering) are discharged from the hospital in the absence of complications on the 10th day of illness. Convalescents are admitted to the children's institution on the 2nd day from the moment of illness. Children who have been in contact with a sick person and have not previously had scarlet fever are allowed to enter a preschool institution or the first two grades of school after 7 days of isolation at home. In the apartment where the patient is kept, regular ongoing disinfection is carried out; under these conditions, final disinfection is unnecessary.