15% of young children admitted for hospital treatment develop an infection caused by the herpes virus type six.
Since a viral infection, namely roseola, sixth disease or sudden childhood exanthema, is complicated by convulsions, timely testing for type 6 herpes becomes important in terms of preventing subsequent complications.
Comprehensive therapeutic measures can prevent recurrence of seizures, as well as encephalitis.
The virus is considered one of the provoking factors of chronic fatigue syndrome, so a blood test for herpes type 6 is also relevant for diagnosing disorders of higher nervous function in adults, as well as in comprehensively identifying the causes of hepatitis, myocarditis, thrombocytopenic purpura, eosinophilia, and drug hypersensitivity syndrome.
Scientific information about herpes virus type 6
Human herpes virus 6 (HHV-6) is the sixth discovered herpes infection.
It was isolated during attempts to find new viruses in patients with lymphoproliferative diseases (characterized by the proliferation of lymphocytes) in 1986. Interesting. HHV 6 includes 2 forms: A and B. As of 2012, HHV-6A and HHV-6B are officially considered separate species, not type 1 variants. HHV-6B causes the childhood disease roseola, whereas HHV-6A is isolated primarily from immunocompromised children.
The specific manifestations of HHV-6A infection are still unclear. However, both HHV-6A and HHV-6B can be pathogenic in the setting of transplantation and AIDS.
Primary HHV-6B infection usually occurs in infants. After primary infection, HHV-6 remains latent unless immunity is compromised. HHV-6 remains latent in lymphocytes and monocytes and is found at low levels in tissues and cells. Children who are able to mount an immune response are not affected by this persistent infection.
Research shows that HHV-6 affects approximately 90% of children under 2 years of age. When HHV-6 is acquired in infancy, symptoms usually appear and medical evaluation is required. But only a small number of patients with primary infection developed roseola or febrile seizures (convulsions due to fever).
Primary HHV-6 is rare in adults. However, reactivation is possible at any age.
Diagnostics
Before choosing the right therapy, it is necessary to determine what caused the disease. A general analysis should show how much the number of lymphocytes has increased, as well as the presence of mononuclear bodies and band neutrophils. After a biochemical blood test, the doctor will be able to make a diagnosis, since it will determine whether ALT and AST levels have increased in case of liver damage. A visual and contact examination of the lymph nodes and the locations of the liver and spleen is also required. In addition, there will be a survey about the first signs and pain scale.
The most important thing in diagnosis is ELISA and PCR studies, which will help determine the presence of antibodies and DNA fragments of the strain to the Epstein-Barr virus. In addition, the patient must be tested for HIV three times (at the height of the disease, and then after 3 and 6 months), since their primary symptoms are similar to each other. Other studies will be prescribed based on the remaining symptoms. For example, an ultrasound of organs that are suspected of enlargement may be required. If nasopharyngeal carcinoma or Burkitt's lymphoma is suspected, a biopsy of the abnormal tissue will be necessary. In addition, consultation with an infectious disease specialist may be required.
Causes of herpes type 6 in children
Herpes type 6 in children most often appears after a decrease in the level of maternal antibodies in the blood. This usually occurs between six months and 3 years of age (average 9 months).
Unlike other infections of viral origin, herpes type 6 in children occurs throughout the year without any seasonal changes.
Some of the possible ways of infection with herpes virus type 6 are presented below.
Infection from an infected person
If your child comes into contact with an infected person, he or she is at higher risk of contracting the infection.
Virus shedding by an infected person

HHV-6 spreads through tiny droplets that come out of an infected person's nose and throat when they laugh, talk, sneeze or cough.
Also, herpes type 6 in children can be spread from infected people who do not show symptoms of the disease.
The incubation period for infection between the period of exposure to the virus and the onset of symptoms is nine to ten days.
Treatment
For recovery, restorative therapy should be carried out with methods aimed at alleviating symptoms. To begin with, antiviral drugs are prescribed, which should stop the growth of the virus and its effect on the cells of the body. The most popular: Ganciclovir, Acyclovir.
To relieve swelling of the inflamed larynx, you will need to take hormonal medications (glucocorticoids) for a short time: Hydrocortisone, Orazon.
After a bacterial infection is associated with the disease, antibiotics are prescribed, such as Metronidazole or Fluconazole.
Treatment also requires the use of immunomodulators and immunoglobudins: Sandoglobulin, Viferon.
The patient should drink a lot to prevent dry throat. Rinsing the area with antiseptic solutions is also recommended. If the disease is accompanied by pain (and in children this is an almost obligatory symptom), then to remove it, you need to make a mixture with 2% lidocaine.
Taking antipyretics is recommended only if the temperature rises above 39 oC.
At the stage of intoxication, it is necessary to use water-salt solutions, as well as glucose intravenously.
They may also offer vitamin therapy to strengthen the immune system.
If tumors begin to form in the area of the nasal passages, chemotherapy and radiation treatment are prescribed.
There are also traditional methods for combating the disease, but their use is also possible after consultation with a doctor.
Forecast
HHV-6 infections are generally uncomplicated and resolve spontaneously in most cases.
They are usually asymptomatic. Even when HHV-6 leads to roseola, it is a mild disease for children with strong immune systems.
Usually the disease goes away without treatment. However, in certain rare cases, patients with an excessive immune response develop additional symptoms, including respiratory failure, seizures.
One infection usually provides lifelong protection, although HHV-6 is sometimes activated in immunocompromised patients.
Rarely, herpes virus type 6 in a child is associated with a fatal outcome; 8 deaths were reported. The causes of death were encephalitis, hepatitis, sudden death in infancy, and extensive infections.
HHV-6 is associated with various complications.
- HHV-6B infection is the most common cause of febrile seizures in childhood (6–24 months).
- Children with HHV-6 may develop encephalitis.
- HHV-6 plays a role in CNS infections.
- HHV-6 infection may increase the severity of cytomegalovirus infection in people with weakened immune systems.
- HHV-6 plays a possible role in lymphoproliferative syndromes.
Why is it dangerous?
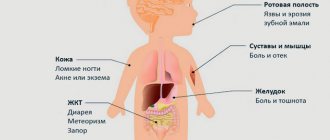
This virus affects the entire lymphatic system and also contributes to the development of cancerous tumors of various organs. This herpes is also dangerous because its activation provokes the appearance of other diseases and complications, including:
- sore throat of the herpetic type;
- hepatitis;
- Infectious mononucleosis;
- genital herpes;
- lymphogranulomatosis;
- sclerosis, etc.
Against the background of type 4 herpes and the associated consequences, a person develops chronic fatigue syndrome, accompanied by apathy, nausea, general malaise, insomnia and a simultaneous desire for constant sleep.
If you are reckless about your health and this virus, and do not take any measures, then soon the damage will reach the brain and nervous system, which in most cases leads to death.
Symptoms of herpes type 6 in children
Symptomatic manifestations occur primarily after primary infection in infants and after primary or reactivation disease in immunocompromised adults.
Approximately 20% of HHV-6 cases present as roseola.
Common symptoms of roseola in children are as follows.

- Fever. The child suddenly develops a high fever. The fever lasts 3-4 days depending on the severity of the infection. In addition, your baby may have enlarged lymph nodes along with other secondary symptoms, namely a sore throat, runny nose and cough.
- Rash. Another significant symptom is the appearance of a rash on the surface of the skin after the fever subsides. The skin rash appears as pink colored raised spots. They may be flat or have a white outline. The rash appears on the back, neck and abdomen. These rashes do not necessarily itch. Those that do not itch remain visible for several hours or even several days before finally disappearing.
HHV-6 infection also sometimes occurs as a rash without fever.
Also not excluded:
- irritability;
- symptoms of ear diseases, otitis media;
- symptoms of upper respiratory tract disease;
- symptoms of bowel dysfunction;
- febrile seizures;
- bulging fontanel;
- symptoms of meningoencephalitis.
Diagnosis of herpes type 6
The characteristic clinical picture of the sudden onset of high body temperature and the development of a typical rash after a decrease in temperature usually allows for the rapid diagnosis of HHV-6 without laboratory tests. However, in some cases additional diagnostic procedures will be required.
Blood analysis
For unusual symptoms, several types of blood tests can help make a diagnosis.
- HHV-6 can be diagnosed by viral culture, serology (antibody test), or polymerase chain reaction (PCR).
- HHV-6 can be isolated from the blood during the first 5 days, and then detected intermittently or constantly in saliva, stool, and less often in urine.
- In a detailed clinical blood test, leukocytes and platelets may be reduced, and anemia is possible.
- On serologic testing, primary infection will be demonstrated by the absence or presence of immunoglobulin G (IgG) and the presence of immunoglobulin M (IgM) to HSV-6. Active HSV-6 disease (primary or reactivated) is demonstrated by a 1.6-fold increase in IgG. Distinguishing primary infection from reactivation can be difficult.
It should be noted that an increase in the number of antibodies to HHV-6 was observed with other herpes viruses. Cytomegalovirus antibodies may cross-react with HSV-6 antibodies. Therefore, exclusion of cytomegalovirus infection is required.
X-ray and computed tomography
A chest x-ray or computed tomography (CT) scan should be performed in patients with respiratory symptoms.
To exclude other diseases, a CT scan of the head should be done with and without contrast.
Indications for these and other diagnostic procedures depend on the clinical situation, especially in immunocompromised patients.
Other tests used to diagnose HHV-6 include bronchoscopy, lumbar puncture, and tissue biopsy.
Diagnosis and treatment
To establish a final diagnosis in children, a diagnostic examination is prescribed, which helps to identify the virus in the body, determine its activity, and establish indirect signs of the disease.
- Complete blood count – neutrophilic leukocytosis, lymphocytosis.
- Blood biochemistry – increased concentration of liver enzymes (AST, ALT).
- Immunological analysis - determination of antibodies to herpesivirus type 4.
- PCR – detection of the genetic material of the pathogen in the blood and other biological fluids.
- Ultrasound of the liver and spleen.
Symptoms and treatment of infection are interrelated. For mild cases of the disease, symptomatic and supportive therapy is prescribed. In severe cases of the disease, etiotropic treatment is carried out aimed at destroying the pathogen. Modern antiviral drugs cannot eliminate the carriage of the virus if it persists in the body. Antiviral antibiotics are prescribed for primary infection or exacerbation of the disease with a severe course.

The treatment regimen for mononucleosis in children is similar to the treatment for respiratory viral infections.
Conservative therapy for infectious mononucleosis:
- bed or semi-bed rest;
- drink plenty of fluids – herbal teas, infusions of medicinal herbs, fruit drinks;
- gargling with a decoction or infusion of chamomile, calendula, a solution of furosemide, orasept;
- antipyretics – panadol, paracetamol;
- immunostimulating drugs - interferons, immunoglobulins;
- antiviral drugs – famciclovir, acyclovir, valacyclovir.
If a secondary infection occurs (staphylococci, streptococci) in the nasopharynx and upper respiratory tract, broad-spectrum antibiotics (macrolides, cephalosporins, penicillins) are prescribed. It is necessary to treat infectious mononucleosis at the first manifestations of infection, which reduces the risk of complications and the disease becoming chronic.
Herpesvirus type 4 causes infectious mononucleosis, erased forms of the disease, and, less commonly, generalized infection in children. After recovery, persistence of the pathogen in the lymphoid tissue can lead to exacerbation of the disease and the development of long-term consequences, including the development of malignant tumors when the immune system is disrupted.
Tweet
Pin It
Tags:Children
- Why does recurrent herpes occur and how does it manifest?
- Enlargement and inflammation of the lymph nodes with herpes
- Interpretation of blood test results for herpes type 1 and 2
- Medicines for the treatment of herpes on the eye and eyelids
What diseases can roseola be confused with?

Primary infection with HHV-6 usually causes fever, which can be difficult to distinguish from other common childhood viral infections. This difficulty also applies to the early stages of roseola, before the rash develops. When the rash appears, roseola may be confused with other childhood skin diseases, especially measles and rubella.
Children with rubella often have preexisting symptoms such as febrile fever, sore throat, joint pain, and bowel complaints, which is not the case with roseola. Additionally, a rubella rash usually starts on the face and spreads to the chest.
Symptoms of measles virus infection include cough, runny nose and conjunctivitis, a high fever that coincides with the development of a rash, unlike roseola.
Roseola can also be confused with scarlet fever, although the latter rarely appears before age 2 and causes a characteristic pinpoint rash. The skin becomes like sandpaper, and a fever appears at the same time.
Roseola can be confused with an infection of enterovirus etiology, especially in summer and autumn.
Drug hypersensitivity reactions can also be difficult to distinguish from roseola. Antibiotics are often given to children with fever due to roseola before the rash appears. A rash after a decrease in temperature may be mistakenly regarded as an allergy to the medication.
How and with what to treat herpes type 6 in a child?
Treatment for herpes type 6 in children varies depending on the clinical situation. Therapy is usually not needed for primary infection in children with healthy immune systems. In infants with roseola, mostly supportive treatment is recommended. Infants who have other manifestations of HHV-6 infection (eg, febrile seizures or central nervous system involvement) should be hospitalized. Overall, about 13% of children with acute HHV-6 infection require hospitalization.
Treatment of children with acute HHV-6 infection should be supervised by a specialist.
Please note that HHV-6 infection cannot be prevented; there is no vaccine.
Children with roseola are advised to rest until the fever subsides and the rash appears.
Consult your pediatrician to evaluate any unusual findings.
Once the rash appears, no additional outpatient care for roseola is required (if this is a typical picture).
Maintenance treatment
Supportive care includes lowering the temperature, ensuring adequate fluid balance, and providing rest.
If the child's fever does not cause discomfort, it should not be reduced. But if the fever is too high, the doctor will suggest medications to reduce the temperature.

Paracetamol can be used. The interval between doses is four hours. Ibuprofen can be used instead of Paracetamol every six hours. Both families of medications are equally effective in reducing a child's fever. There is no medical benefit to alternating Paracetamol and Ibuprofen.
Aspirin should never be used to reduce fever in children or teenagers.
A child with a fever should be kept comfortable and away from exertion. Overloading may cause the temperature to rise. Swimming in cool water (29.5˚C) will help reduce fever by 1-1.5 degrees. If your child develops tremors during bathing, the water temperature should be increased.
Never rub your child with alcohol. Alcohol vapor can be inhaled, causing a variety of problems.
What to do if you develop febrile seizures
A sudden and rapid increase in temperature can cause an attack (convulsions). Febrile seizures are common in 3% of children 18 months to 3 years of age. They occur in 5-35% of children with roseola.
The most difficult thing is to remain calm while helping a child.
- Loosen any clothing around the neck.
- Remove sharp, potentially traumatic objects and turn the child on his or her side to allow saliva to drain from the mouth.
- You can put a pillow under your head, but don't put anything in your baby's mouth. It's best to just wait. Most febrile seizures (associated with roseola or other viruses) last less than five minutes.
- Do not leave your child unattended. Children are often lethargic and sleep after a seizure. This is fine.
- After an attack, it is better to consult a specialist to examine the child.
The attack may look very scary, but it is usually quite harmless. Febrile seizures are not associated with long-term nervous system problems or brain damage. Anticonvulsants are rarely prescribed to treat or prevent febrile seizures.
Antiviral drugs
Specific antiviral therapy is not recommended for routine cases of primary HHV-6. Unusual or severe manifestations of primary or suspected reactivated HHV-6 infection (such as encephalitis, especially in immunocompromised patients) may benefit from treatment.

Ganciclovir, Foscarnet and Cidofovir demonstrate inhibitory effects against HHV-6 under artificial conditions. Case analysis suggests that all three drugs, alone or in combination, can reduce HHV-6 viral DNA doubling, as evidenced by reductions in viral load in plasma and cerebrospinal fluid.
However, clinical data on effectiveness are inconsistent and contradictory.