What is fluorography: description of the procedure
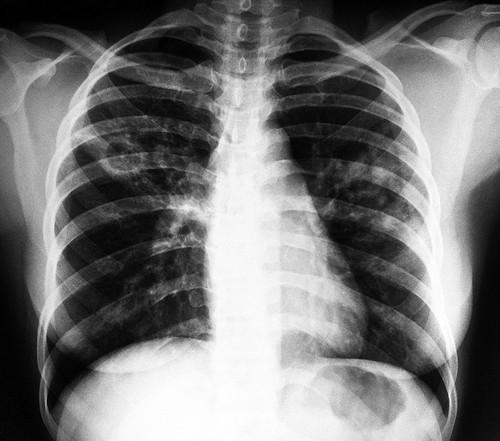
The technique is characterized by photographing the lungs using X-rays. The image is displayed on a fluorescent screen. Parts of the human body absorb radiation unevenly, so the bones are clearly visible in the picture, while other parts of the body are invisible (lung tissue) or translucent (large vessels, heart).
The film technique is common in clinics and hospitals, but recently it has been replaced by a digital one, in which the radiation exposure to the body is reduced. The test is carried out annually to prevent disease.
A fluorograph is used to exclude or detect diseases of the pulmonary system: bronchitis, pneumonia, tuberculosis, neoplasms.
Frequent X-ray radiation results in tumor formation many years and 10 years later, but this risk is thought to be very small (comparable to natural background radiation dose [5]). Thus, according to one Oxford University study, by age 75, X-rays increased the risk of cancer by 0.6-1.8% in 13 of the 14 countries examined, and in one country (Japan) which had the highest estimated annual exposure rate in the world, this figure is just over 3% [1].
The difference between fluorography and x-rays: radiation dose
Fluorography and radiography are procedures that examine the structure of the body using x-rays. Their main difference is in detail: x-rays display the image in full size and are used as prescribed by a doctor.
Characteristics of fluorography:
- radiation dose – 0.01-2.5 mSv [2, table. 6.1],
- the image is less clear, formations as small as 6 mm are visible,
- the purpose of the study is prevention (once a year),
- used to study the lungs,
- contraindications: period before conception, pregnancy, children under 14 years of age,
- the price of the procedure is 4-5 times less than an x-ray.
X-ray characteristics:
- radiation dose – 0.01-1.6 mSv [2, table. 6.1],
- the image is clear, pathological formations as small as 2 mm are visible (this allows for timely diagnosis of the smallest cancerous formations),
- the purpose of the study is to diagnose the suspected disease,
- used for any organs and systems,
- frequency of use - as needed (for bone fractures, repeated scanning is required),
- contraindications: period of conception, pregnancy, postpartum period, menstruation (contraindications are relative, there are exceptions),
- expensive procedure.
Since the first method is cheaper, it was decided to use it for preventive purposes annually. The second can be done as prescribed by a doctor; its cost increases with several projections of the body structure being examined.
The annual radiation dose , according to SanPin 2.6.1.2523-09 clause 1.4, should not exceed: for the skin - 50 mSv, for the lens of the eye - 15 mSv [3]. At the same time, the dose of annual natural radiation is 1-10 mSv (the global average is 2.4 mSv) [4].
Indications for fluorography during lactation
Is it possible to do fluorography while breastfeeding? The answer to this question is very ambiguous and depends on the purpose of the study. If a woman needs to undergo fluorography for preventive purposes, then it is better not to do this, since this is not an urgent examination. It is necessary to wait until the end of lactation and only then take a picture. Although it has not been proven that radioactive radiation accumulates in breast milk and can somehow affect the baby.

Fluorography of a nursing mother is mandatory if there are certain indications, such as:
- Suspicion of tuberculosis - prolonged cough, low-grade body temperature, weakness, sweating, weight loss. There are auscultatory signs of an inflammatory process in the lungs.
- Contact with a person suspected or diagnosed with tuberculosis.
- Having close relatives or friends who have been diagnosed with this infectious disease.
- Living in a communal apartment or dormitory, where a patient with tuberculosis has been identified in the neighborhood.
- Subject to contact with children who have a positive reaction based on the results of the Mantoux test.
- Suspicion of neoplasms of the chest organs, mammary glands, mediastinum, as well as inflammatory processes in the lungs, pleura, and diaphragm.
In this case, the fluorographic method of examining the chest organs is much lower than the risk of developing tuberculosis, which is a very serious infectious disease that requires long-term hospital treatment.

During the procedure, the person receives a minimal dose of radiation. It is enough to get an accurate result, but very little to cause significant harm to a woman’s body. Therefore, fluorography is an approved method of examining the lungs, the potential risk of which is much less than the expected benefit. And the effect of radioactive radiation ends immediately after the device is turned off.
Types of fluorography: differences
Before undergoing the procedure, you need to find out which device is installed in the medical facility. institution. They come in two types:
- Film - a screen is used on which the image is projected. The film on which the photograph is displayed has a certain degree of sensitivity, so the radiation dose cannot be reduced.
- Digital - radiation is carried out by a fan-shaped beam. The image is displayed on the monitor. The cost of the procedure is reduced; there is no need to purchase films. The amount of radiation is reduced by 10 times, this expands the consumer group, eliminating the risk of cancer. The high throughput of digital fluorography improves image quality, bringing it closer to an x-ray image.
Radiation with the film method (for cervical vertebrae) is 0.3 mSv, with the digital method - 0.03 mSv.
If possible, you should choose the digital method. It allows mothers not to worry about the question of how much time should pass after fluorography so as not to harm the baby with breast milk.
Why do you need to do fluorography?
If a doctor prescribes fluorography, everyone has the right to refuse. Even if there is no logical reason for this. An ordinary “no” is quite enough; they have no right to force people to undergo analysis, neither in antenatal clinics, nor in maternity hospitals, nor anywhere else.
All prevention should be carried out after breastfeeding is completed, or during the period when the baby can last a day or two without milk. This happens closer to six months of life. Delaying a preventive examination even by five months will not be as bad as the slightest effect on milk. There is no scientific data on the effect of fluorography on breast milk, and under no circumstances is it worth checking.
However, it so happened that fluorography is prescribed during breastfeeding. Don't say "no" harshly. The procedure is prescribed only if necessary. If the mother has had contact with tuberculosis patients, or feels some symptoms, be sure to undergo an examination and take a photo of the lungs.
Fluorography during breastfeeding: limitations
During the process of bearing a child, the immunity of expectant mothers does not fully function; there is a risk of contracting diseases that are hidden in nature, or cancerous formations in the chest or mammary gland. Pathology studies are carried out after childbirth. Fluorography cannot be performed during pregnancy due to potential risks [7]. Radiation affecting the fetus will cause more harm than to the mammary glands during lactation.
There is a risk of a child contracting tuberculosis through close contact with the mother. To avoid this, a chest scan is performed immediately after the baby is born. Breastfeeding mothers are allowed to undergo fluorography for the following reasons:
- the appearance of symptoms of lung disease: shortness of breath at rest, frequent cough with or without sputum, increased body temperature, chest pain during inhalation and exhalation, unnatural sounds when breathing (creaks, wheezing, whistles),
- contact with a tuberculosis patient,
- positive Mantoux test in close relatives,
- hospitalization of a nursing mother with her baby,
- exacerbation of a chronic disease of the maternal pulmonary system,
- mother and child live in unsanitary conditions.
There is no annual preventive procedure; fluorography of a nursing mother is a last resort. The examination is prescribed only by a doctor, who will determine whether the child can be fed after the examination. The sooner abnormalities are identified, the sooner treatment will be carried out.
Fluorography in the maternity hospital
Women are concerned about whether it is possible to do fluorography on a nursing mother. Nursing mothers undergo fluorography after childbirth in the first three days as prescribed by the doctor. The procedure is performed only at the request of the nursing woman. If she does not give her consent to undergo fluorography while breastfeeding, she must fill out a refusal form. Doctors do not force the mother to undergo examination without the desire of the mother, but must explain to her why women should undergo examination after childbirth.
Refusal does not affect discharge from the hospital. A woman is discharged if she and the child have no complications after childbirth or serious illnesses. However, in order to register with a children's clinic, fluorography is necessary, even when breastfeeding.
An X-ray of your chest, limbs or teeth is equivalent to several days' worth of background radiation, and the chance of cancer is less than 1 in 1,000,000 [5].
Effect of radiation on breast milk and baby
Does breast milk remain useful after fluorography, after what period of time is breastfeeding allowed? During the scan you will receive a small amount of radioactivity, some of which may pass into your breast milk. If your child drank this milk, he was also exposed to a small amount of radiation, the less the better.
How much radiation will my child receive? If you follow the specific advice given by the Department of Nuclear Medicine for the test [7], your child will only receive a tiny dose of radiation. However, even if you didn't follow this advice, your baby will only receive a radiation dose that is less than the natural background radiation we receive every six months.
When can you feed your baby after the procedure?
Why should you stop breastfeeding for a few hours? This is to ensure that the level of radioactivity your baby gets from the milk is very low. This is done in two ways:
- Wait a while: the amount of radioactivity in your milk will decrease over time.
- By expressing milk, you will get rid of radioactivity. [8]
When is it better to give up?
Although the radiation dose is minimal, the procedure is not recommended to be performed frequently. If you are asked to take an x-ray while breastfeeding, for example, during a medical examination or just in case, it is better to refuse. You always need to compare possible risks and the actual need for examination. You should always remember that x-rays are a source of radiation, albeit a minimal one.

- Temporary changes in blood composition after excess radiation.
- Cataracts are possible.
- Development of cancer (including leukemia).
- Rapid aging, premature death.
Dental examination during breastfeeding
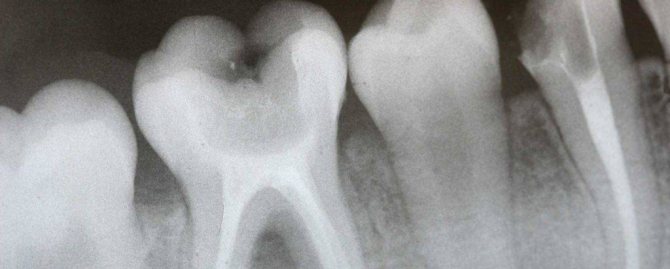
Most often, dental x-rays during breastfeeding are prescribed for:
- identifying the source of pain or the cause of curvature;
- viewing the location of the seal;
- detection of a focus of inflammation or cyst, as well as in diseases of soft tissues;
- clarifying the possibility of saving the tooth;
- diagnosis of caries.
Dentists assure that the procedure while breastfeeding is safe and does not affect breast milk in any way. But if there is an opportunity to conduct the study in a good clinic with modern equipment and a minimum dose of radiation, it is better to take advantage of it and not put yourself and the baby at risk.
In what cases is the procedure necessary?
Radiography is a study that modern medicine practices quite often. In some cases, you may not need to take an x-ray. But if a nursing woman feels unwell for quite a long time, then it is better to carry out the procedure in order to identify the exact cause of the malaise.
X-rays are justified in cases where:
- trauma and possible fracture or crack;
- signs of tuberculosis - a strong, suffocating cough with a possible increase in temperature for quite a long period of time;
- symptoms of sinusitis;
- signs of bronchitis;
- sharp, cutting pain in the stomach;
- toothache and dental complications.
Preparing nursing mothers for examination

There are no recommendations for breastfeeding mothers on how to take measures to protect the mammary glands. The doctors conducting the study answered the question: “Do I need to pump before the procedure?” - they answer negatively. The amount of radiation is so small that it will not cause negative effects in a woman’s body. If a woman is concerned about the condition of her milk after the examination, she can consult with a mammologist or therapist and find out whether fluorography can be done while breastfeeding.
Rules to help avoid excessive exposure to radiation:
- conducting examinations in extreme cases,
- examination that does not require urgency should be carried out after completion of breastfeeding,
- feed the child immediately before the examination and 3 hours after it,
- use of a protective apron during the procedure,
- choice of x-ray equipment before fluorography for hepatitis B: choose the one that uses less radiation.
The results of the examination are not affected by food consumption, exercise, smoking, or taking medications. The accuracy of the results is affected by:
- jewelry of any size and material, located below the collarbones,
- un-removed bra,
- hair below the collarbones.
When conducting the examination, you must follow the doctor's instructions: press your chest to the screen, do not move, do not breathe. If the conditions are not met, the image will be unclear.
Are lactation and x-ray examination compatible?
In recent years, a lot of scientific research has been carried out to determine how radiation affects mother's milk. It has been established that the quality of milk produced does not change after the procedure, so X-rays and breastfeeding are quite compatible and there are no prerequisites for refusing feeding. The mother can continue breastfeeding even after the test. For example, X-rays of the stomach using barium are considered safe. This substance does not settle in the female body, is not absorbed and does not have a negative effect on the quality and production of milk.
It is only necessary to wait a certain period of time after an x-ray if an examination of internal organs is being carried out. Since for this procedure other contrast agents are used, which help to see the picture of what is happening more clearly.
However, breastfeeding is not a contraindication for x-rays. This is rather a precautionary measure, which is reported by the manufacturers of X-ray machines, in order to in no case allow negative consequences of the procedure for both mother and baby.
Such a study is prescribed to identify the following pathologies:
Do I need to pump before fluorography?
Almost all women who breastfeed ask their health care workers whether there is a need to pump? Experts say that irradiation stops immediately after leaving the fluorography booth, and there is no residual amount of rays in the milk. You can express before the procedure if the baby is fed and the remaining milk will not be needed in the next couple of hours.
We recommend reading: Thuja Edas-801 – instructions, use of oil for adenoids, reviews, price
After diagnosis, many mothers prefer to dispose of expressed milk so that it does not harm the baby. If a woman is worried about this, doctors do not prohibit expressing milk once, but they do not advise taking the baby away from feeding for 2-3 days. This can affect lactation and teach the baby to suck the pacifier, which will put feeding at risk.
How is the procedure performed?
Fluorography during breastfeeding requires certain psychological preparation. After all, every mother worries about her baby. First of all, it should be remembered that this procedure is done when necessary. There are no restrictions before or after fluorography.
To reassure the mother before the study, certain measures can be taken. Immediately before going to the clinic, you need to feed your baby breast milk. After fluorography, it is better to refrain from feeding for about 3-4 hours, and express the milk formed during this time and pour it out. If the baby is only breastfed, you can pre-prepare some milk. This will allow you to feed your baby when he gets hungry.

Under no circumstances should you give up breastfeeding for a longer period. No formula or milk expressed in advance can replace breastfeeding. Moreover, the baby may get used to the nipple and refuse to take the breast.
Each fluorographic or x-ray diagnostic room has a special rubberized apron that a woman can put on before the procedure. Therefore, you need to focus the attention of medical personnel on the fact that you are a nursing mother, and you will definitely need it.











