The stomach hurts at the 23rd week of pregnancy due to the influence of external negative factors and the development of the disease. Timely diagnosis is required to prevent the threat of miscarriage and early birth. This is done by the attending gynecologist.
How long have you had this pain syndrome?
- Several days (26%, 782)
- First day (21%, 634 Votes)
- Several months (13%, 382)
- Week (10%, 309)
- Several weeks (10%, 301)
- About a month (8%, 250)
- Chronic form (7%, 205)
- About a year (6%, 181)
Total voters: 3 045
Loading …
Use search Are you having a problem? Enter “Symptom” or “Name of the disease” into the form, press Enter and you will find out all the treatment for this problem or disease.
Why does my stomach hurt at 23 weeks of pregnancy?
After 3 months, the patient’s toxicosis disappears.
If it persists, the condition is accompanied by surges in blood pressure, and gestosis is formed. It is dangerous for the placenta, uterus, and baby. A large amount of protein is excreted in the urine, which indicates a dysfunction of the urinary system. By this time, most women's bellies begin to grow. If you use your old clothes, discomfort occurs. The painful sensations intensify when the girl sits. It is recommended to purchase special trousers with an elastic band that do not compress the stomach and the contents inside it.
Many pregnant women feel fetal movement already at this stage. If he moves his leg too much, it is perceived as painful. The condition passes quickly; after the cessation of active actions of the embryo, the discomfort disappears.
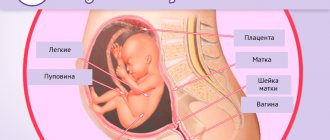
The reason is pressure on the areas of surrounding organs:
- bladder, kidneys;
- liver, spleen;
- intestines.
If mother and child have a Rh conflict (absence of the Rh factor in the mother, but presence in the baby), by this time it has been eliminated with the help of drug therapy and additional procedures.
But the condition is periodically accompanied by pain. The doctor is informed about this in order to prevent premature contractions due to increased immune activity.
By 4-5 months, doctors recommend limiting physical activity. Sports activities, active running, and other stress lead to increased pressure on the ligaments and muscles surrounding the uterus. The pain becomes nagging, aching.
Recommended lifestyle for pregnant women
At this time, expectant mothers should, first of all, take care to get the maximum positive emotions from this quiet time of pregnancy and minimize the associated inconveniences. In addition, it is necessary to ensure that the baby receives everything necessary for his development. Therefore, during this period, the pregnant woman should be provided with:
- A varied, balanced diet with the obligatory inclusion of fermented milk products. Kefir and natural yogurt help prevent constipation and promote better functioning of the gastrointestinal tract.
- Get enough sleep. At this stage, many expectant mothers cannot find a comfortable sleeping position. If caring relatives have already given you a special pillow for pregnant women, it’s time to use it.
- Physical activity should be feasible. In case of lower back pain, wearing a special bandage is a great help.
- It's time to pay special attention to breast care. A bra a size or two larger, made of natural cotton, is a necessary thing. It should be washed often, and the breasts should be washed daily with warm water.
- If pigmentation appears on the face, you should limit your exposure to the sun. The use of whitening creams is not only ineffective, but can also be harmful to the child.
Anything that brings positive emotions and helps bring mother and baby closer together is useful; for many, the “nesting instinct” awakens - women are happy to clean the house, plan the arrangement of the nursery, and do handicrafts. So that the future dad does not feel out of place, take him with you to a family photo session in order to leave memories of this wonderful time.
What causes nagging, aching pain during pregnancy?
It is visually impossible to identify the true cause during a general examination. A woman complains of emerging negative symptoms that worsen her health and well-being.
The following diagnostic tests will be needed to determine the diagnosis:
- laboratory tests of blood, urine, feces, vaginal discharge;
- Ultrasound of the abdominal cavity, pelvis, fetus;
- CTG;
- ECG, ultrasound of the heart.
Examinations such as radiography and MRI are prohibited. They use radiation that has a detrimental effect on embryonic cells. Using tests, the condition of internal organs and systems is determined.
Determine the disease leading to negative symptoms:
- sexually transmitted infections spreading through the placenta, amniotic fluid (infection of the fetus will lead to impaired growth and development);
- dyspeptic disorders, heartburn (it is believed that it appears if the child’s hair is actively growing);
- neurological disorders leading to convulsions, numbness of the limbs, pain;
- spasm, narrowing, damage to blood vessels that deliver nutrients to the placenta (patients with coronary artery disease, diabetes mellitus, atherosclerosis are predisposed);
- increased tone of the uterine muscles.
If a disease is detected, treatment is prescribed. The course of pregnancy becomes more difficult. Therefore, the expectant mother must undergo tests to determine the functionality of the body. If a threat appears, she may be admitted to a hospital for therapy under the supervision of a doctor.
Problems in the twenty-third week of pregnancy
Despite the established opinion about the stability of the expectant mother’s well-being in the second trimester, unpleasant “surprises” may well lie in wait for her.
Nausea at 23 weeks of pregnancy
Nausea during pregnancy is most often characteristic of the first trimester, but if it bothers you up to 23 weeks, this may indicate pathologies. In addition, sometimes nausea is not due to the fact that the woman is pregnant, but due to the presence of gastrointestinal diseases.
Short-term, intermittent nausea can be caused by:
- food poisoning;
- taking antibiotics;
- traumatic brain injury;
- long exposure to the sun.
If the causes of nausea are unclear, you should consult a doctor.
Preeclampsia
Often toxicosis of the first trimester is replaced by late toxicosis - gestosis. It is more typical for the third trimester, but it is also quite capable of appearing at the end of the second. What is it?
In the international classification of diseases ICD 10, gestosis is designated as a complication of a normal pregnancy and is classified as follows:
- Hypertension complicating pregnancy, childbirth and the period after it.
- Hypertension with proteinuria (detection of protein in the urine).
- Edema and proteinuria without increased blood pressure.
- Eclampsia is a significant increase in blood pressure that threatens the life of the mother and fetus.
All these symptoms can manifest themselves to varying degrees, and this is the basis for the classification of gestosis according to the severity of its manifestation. The severity is calculated based on the table data. To do this, points are calculated based on the clinical picture, and the patient’s condition is assessed based on the results of their total number.
| Symptoms | Points | |||
| 0 | 1 | 2 | 3 | |
| Edema | none | in the shin area | shins, stomach | all over the body |
| Protein in urine | absent or slightly exceeded | 0,03-0,13 | 0,12-1,0 | above 0.1 |
| Systolic blood pressure (millimeters of mercury) | up to 130 | 130-150 | 150-170 | from 170 |
| Diastolic blood pressure (millimeters of mercury) | up to 85 | 85-95 | 90-110 | from 110 |
| Time of onset of symptoms | no symptoms | after 36 weeks | after 30 to 35 weeks | after 20 weeks |
| Intrauterine growth restriction | absent | absent | for 1-2 weeks | more than 3 weeks |
| Accompanying illnesses | none | were before pregnancy | appeared during pregnancy | were before pregnancy and are during it |
Result:
- 0-7 points - mild degree of gestosis;
- from 8 to 11 - average degree of gestosis;
- 12-21 points - severe gestosis.
In any case, regardless of the number of points, for any manifestations of gestosis, you must consult a doctor.
Diarrhea and constipation
Any changes in stool during pregnancy are a reason to reconsider your diet. Diarrhea occurs due to the consumption of low-quality, expired food, as well as a large number of “laxative” foods (prunes, fermented milk products, fresh vegetables, and so on). Diarrhea can signal both food poisoning and an intestinal infection. In this case, you will be worried about: abdominal pain, dizziness, vomiting, nausea.
Constipation is most often caused by physiological reasons specific to pregnancy: the effects of hormones, compression of the intestines by the uterus. Constipation can cause the development of hemorrhoids, which is why it should not be allowed to become chronic. Prevention of constipation is a proper diet rich in dietary fiber and sufficient fluid intake. If prevention does not help, you can use approved medications: rectal suppositories (glycerin and others), microenemas (such as Microlax), a remedy (for example, Duphalac).
Heartburn
During pregnancy, the enlargement of the uterus inevitably leads to the fact that the position of the stomach changes somewhat: it rises slightly and flattens. The esophagus also undergoes similar metamorphoses: the lower esophageal sphincter is stretched, and its valve, which acts as a barrier against eaten food and gastric juice, begins to work intermittently. This is how heartburn occurs: stomach acid and food from the stomach are thrown back into the esophagus.
The situation can also be aggravated by the extra pounds that many expectant mothers gain, following their grandmother’s saying: “You need to eat for two.” And also food that is conventionally classified as “harmful” provokes heartburn: smoked meats, marinades, spicy and salty foods.
Flatulence, which many pregnant women experience from time to time, also contributes to heartburn. Gases from the intestines and stomach push gastric juice into the esophagus, hence the feeling of burning and bitterness. Malfunctions also occur in the autonomic nervous system, which is responsible for coordinating the work of the digestive organs, and disturbances occur in the process of moving food through the esophagus.
Heartburn also serves as a marker of certain diseases:
- gastritis;
- stomach ulcers;
- diaphragmatic hernia;
- diabetes mellitus
Normalizing nutrition and eating food often, but in small portions, significantly improves the condition of the pregnant woman. If your health does not change for the better, the doctor may prescribe prokinetic drugs (Duspatalin, Trimedat - only for strict indications) or antacids (Rennie, Gastal, Maalox and the like), as well as drugs that activate the gastrointestinal tract (Motilium, Motilak and some analogues) .

Stomach hurts and pulls
When your stomach hurts at 23 weeks of pregnancy, it is important to identify the cause of the pain. It could be:
- eating disorder;
- constipation;
- physiological pain caused by changes in the body (pressure of the uterus, sprained ligaments, movements of the baby, and so on);
- abdominal trauma;
- threat of premature birth.
If the first two reasons can be corrected by dietary adjustments, and the third can be tolerated, then the last two require immediate consultation with a doctor.
Bleeding at 23 weeks of pregnancy
Vaginal bleeding during pregnancy is not normal, but it is not always dangerous. It is worth distinguishing spotting from bleeding. “Smearing” may well be due to erosion or polyps. The doctor should warn you about this if such problems are identified. But heavy bleeding is a dangerous symptom; it is a direct threat to the life of the baby and mother. Bleeding may be the onset of premature labor or a manifestation of diseases of the internal genital organs.
Premature birth
If labor begins this week, it will be considered premature without using the term “miscarriage.” Premature birth begins at 22 weeks, and the baby is considered viable, but it only has a chance to survive with medical help. Doctors are obliged to make efforts to save the baby if its weight exceeds half a kilogram and the newborn shows signs of life.
Premature birth is divided into:
- threatening;
- beginning;
- started.
In the first two cases, if timely measures are taken, labor can be stopped and pregnancy can continue.
Why does premature birth occur? There are many factors, these are:
1. maternal:
- previous abortions or premature births;
- surgical intervention on the uterus and its cervix;
2. caused by real pregnancy:
- low socio-economic standard of living of the mother (poor nutrition, living conditions, etc.);
- bad habits;
- maternal age up to 18 and after 35 years;
- infections;
- placenta previa;
- premature opening (rupture) of the amniotic sac;
- other pathologies.
Predicting premature birth is almost impossible, since the mechanism of its occurrence has not yet been studied. There is a special test that determines the content of fibronectin, a special substance found in vaginal discharge. Normally, fibronectin is released only before birth. But such a test is not available in our country.
In addition, there is also an ultrasound method (transvaginal) to measure the length of the cervix. So far this is the only available method for diagnosing preterm birth.
Frozen pregnancy at 23 weeks
A frozen pregnancy can occur at any stage, including at 23 weeks of pregnancy. The main reasons for the cessation of development are genetic pathologies or infection of the fetus. With such a diagnosis, urgent removal of the dead fetus from the uterine cavity is necessary; delay can cost the mother her life.
In most cases, the prognosis for further pregnancies is favorable. However, the woman and her partner should undergo a detailed examination and begin the next attempt to conceive no earlier than six months later.
Colds. ARVI, fever, flu. Can I take antibiotics?
Getting a cold at 23 weeks is less dangerous than in the first trimester. The formation of the embryo is complete, and antibiotics are not so scary for the baby. However, their use is justified only under strict indications, and the choice of antibiotic should be made by the doctor. Not all antibiotic drugs are allowed during pregnancy.
If the temperature rises, it is allowed to take paracetamol or ibuprofen without consulting a doctor. Inhalations and saline solutions will help relieve nasal congestion. The doctor can select vasoconstrictor drops, which can be taken only when absolutely necessary.
Under no circumstances should you be vaccinated against influenza during pregnancy!
Food poisoning - what to do?
Food poisoning is caused by poison that enters the body through food. Poison may contain bacteria, toxins in poor-quality food, and the food itself (for example, mushrooms or vegetables with pesticides). The symptoms of food poisoning are obvious: vomiting, abdominal pain, diarrhea. If poisoning is caused by food, symptoms may not appear immediately, but within 48 hours.
You should immediately seek medical help, as such intoxication threatens the life of the mother and child. Before the ambulance arrives, it is necessary to rinse the stomach and, if possible, provide bed rest for the victim.
Toxoplasmosis at 23 weeks of pregnancy
Many expectant mothers are afraid of toxoplasmosis, and with the onset of pregnancy they try to get rid of pets and cats, since these animals are considered the main carriers of toxoplasmosis. However, infection can also occur through meat products, soil, and water.
Most people do not suspect that Toxoplasma has already been in their body. If a person’s immunity is fine, the disease proceeds, masquerading as an acute respiratory viral infection. Therefore, during pregnancy, not all mothers become infected, since they already have antibodies to toxoplasmosis.
To determine whether a pregnant woman is at risk, a blood test is prescribed for toxoplasmosis. And only if antibodies are not detected, should you worry. But there is reason for concern. If in the 1st trimester toxoplasmosis can lead to miscarriage, in the second the infection is milder, because intrauterine infection occurs in 1/3 of cases of mothers. There are also drugs against toxoplasmosis that are approved during pregnancy from the second trimester. But negative consequences for the fetus are still possible. They manifest themselves in malformations of the brain and nervous system, visual and digestive organs.
Low placentation (low placenta)
One of the reasons for pregnancy complications may be low placentation. This diagnosis is made when the distance from the lower edge of the placenta to the internal os of the uterus is less than 5 centimeters. Normally, the higher the placenta is attached to the fundus of the uterus, the better.
The danger of a low-lying placenta is that the baby receives less nutrition and oxygen. This can cause IUGR or hypoxia.
In practice, more than 90% of women with low placentation give birth to healthy children at term, but increased attention from doctors in this case will not hurt.
Short cervix
A short cervix is a potentially dangerous condition during pregnancy. If its length is less than 2 centimeters, as the fetus grows, it is difficult for the cervix to withstand the pressure from the uterus, it begins to open, which leads to premature birth.
Shortening of the cervix can be caused by external interventions (surgeries, abortions), hormonal changes or the anatomical characteristics of the woman herself.
With a short cervix, installation of a pessary or suturing is often practiced to maintain pregnancy. At the same time, a woman should avoid physical overload, give up sports and sex.
Thickening of the placenta
The baby grows, and the placenta grows accordingly. To withstand the fetus and the pressure of amniotic fluid, the placenta also thickens, and from about 34 weeks the thickening stops and begins to prepare for childbirth, or “age”, in the language of doctors.
However, it happens that thickening occurs more intensely, and at 23 weeks the thickness exceeds the norm (more than 32-33 millimeters). And this is very dangerous, because such a placenta will begin to age earlier, which means that childbirth will occur faster.
With a thick placenta, the baby receives less oxygen and nutrients. Therefore, it is necessary to promote uteroplacental blood flow, and the drugs “Actovegin” and “Curantil” have been developed for these purposes.
What does dull, pulling, point or cutting pain in the abdomen indicate?
Stomach pain during pregnancy is due to changes in the body, in organs associated with hormonal changes, changes in the position of internal organs, and obstetric pathologies.
Many types of these sensations do not pose a threat to the health of the mother or the condition of the fetus. Others cause significant harm and even death to the woman and the unborn child.
Pain is a reaction of the nervous system to stimuli. A symptom of many diseases, including obstetric pathologies during pregnancy. A pregnant woman experiences hormonal changes and a restructuring of many systems. They are also accompanied by this feeling.
If discomfort and pain occur, it is better to consult with your doctor about the nature of these sensations and appropriate treatment. During pregnancy, a woman is responsible not only for her own health, but also for the health of the baby.

Nature has determined that the mother’s body tries to protect the fetus from all negative influences. A plug formed from mucus in the cervix prevents pathogenic microorganisms from entering.
Umbilical cord nutrition is formed in such a way that harmful chemical compounds do not enter the fetus. The uterus itself protects the child from external mechanical influence.
At the same time, during the period of bearing a baby, the woman herself may regularly experience pain of varying intensity and nature. Each type of discomfort indicates the presence of different pathological conditions, with the exception of harmless obstetric ones associated with changes in the maternal body and preparation for childbirth.
Based on the nature, intensity of pain, and gestational age, we can talk about how dangerous the condition is.
For example, pulling, extending to the lower back and groin, may indicate a risk of miscarriage. An additional sign of the condition will be the presence of bloody discharge.
In this case, you should immediately seek medical help and undergo an examination. If you delay visiting a doctor, the frequency of contractions will become more frequent and spontaneous miscarriage will occur.
Uterine tone is dangerous regardless of how early it was diagnosed. The fetus may experience a lack of oxygen and incoming nutrients. The woman feels a sharp pain like contractions. The solid state of the uterus and lower abdomen is recorded.
In case of injury, late toxicosis, or stress, placental abruption may occur. The condition is accompanied by acute pain in the lower abdomen. Often there is internal bleeding without external manifestations in the form of discharge. Urgent hospitalization and surgical intervention are required. Without help, death will occur.
Cramps accompanied by dizziness at five to twelve weeks can be a symptom of an ectopic pregnancy. For a number of reasons, the egg was unable to enter the uterus and became embedded in the fallopian tube.
As a result of the rapid growth rate of the fertilized egg, severe pain occurs. The woman is sent for an ultrasound examination. An operation to terminate the pregnancy is prescribed. Lack of medical care will result in death for the pregnant woman.
A number of non-gynecological problems also contribute to the occurrence of unpleasant sensations in the lower abdomen:
- Disruption of the gastrointestinal tract. Additional symptoms: bitterness in the mouth, tingling in the lower abdomen, heartburn.
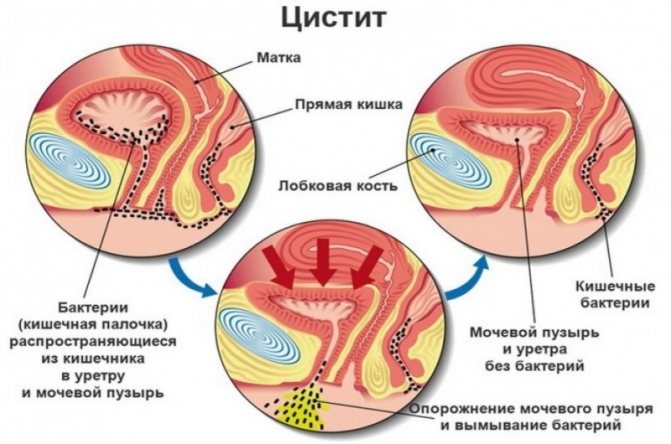
- Inflammation of the bladder and urinary tract. Symptoms: discomfort and burning when urinating, increased frequency of the urge to urinate, increased body temperature.
- Seasonal colds. They are accompanied by headaches, nasopharyngeal congestion, aching bones, and fever.
- Inflammation of the appendix (appendicitis). An acute condition in which severe vomiting occurs, weakness, and a strong increase in temperature are detected. Surgery is used to remove the inflamed area. This procedure is safe for a pregnant woman. Abdominal laparotomy appendectomy is used if peritonitis is suspected and less invasive laparoscopy is used if there are no signs of peritonitis. A course of rehabilitation therapy is prescribed.
It is possible to diagnose the pathology based on additional symptoms. Treatment should be supervised by medical professionals. It is prohibited to take pharmaceutical drugs on your own. If you aggravate your own condition through inept actions, this will inevitably affect the child’s development.
Ultrasound
At 23 weeks of pregnancy, parents will probably be able to determine with an ultrasound whether they should choose a girl’s or a boy’s name for their unborn child. The sexual characteristics of the fetus are now clearly differentiated, and ultrasound examination can tell about them, if, of course, the baby turns successfully. However, the main task of ultrasound at the 23rd week of pregnancy remains to exclude pathologies of fetal development and diagnose the child’s condition. During an ultrasound, the doctor will assess the size of the baby, the correspondence of these same sizes to the gestational age, listen to the heartbeat and assess the baby’s physical activity. There is also an examination of the internal organs of the fetus, assessment of the development of individual parts of the body and their relationship to each other. Corresponding indicators are necessary to exclude possible malformations of the baby and to ensure the absence of any chromosomal abnormalities. In addition, the doctor will assess the size and condition of the uterus and look at the location of the placenta. Just don’t be upset right away if, during an ultrasound examination, it turns out that the placenta is located too low. Very often, during the next weeks of pregnancy, due to further enlargement of the uterus, the placenta rises and takes on its “proper”, non-threatening position.
When do you need to see a doctor urgently, and which doctor will help?
Cases of pain where medical intervention cannot be avoided:
- Cramping attacks of a pulling nature (especially in the first trimester of pregnancy) - you need to immediately seek help. There is a high risk of miscarriage or placental abruption. The presence of mucous discharge mixed with blood is a reason to call an ambulance for immediate hospitalization of the patient.
- Shingles with a return to the lower back in the presence of a burning sensation at the time of urination - signs of the development of pyelonephritis. Long-term treatment may be required. Signs of illness should be reported immediately.
- In the later stages, accompanied by contractions and increased uterine tone - a sign of premature birth.
Regardless of the stage of pregnancy, the appearance of bleeding from the vagina with or without pain - you should definitely call an ambulance.

Consulting a pregnant woman and caring for the patient during pregnancy is the responsibility of the local obstetrician-gynecologist. They work in district antenatal clinics.
You can get an appointment with them in the following ways:
- through an electronic appointment system;
- by calling the registration number of the medical institution;
- Some consultations retained the journal recording system.
If the pain is not associated with the course of pregnancy and does not affect the development of the fetus, then you need to contact your local physician. It is important that treatment is selected taking into account saving the life and health of the mother and child.
Where does ARVI come from?
It's no secret that ARVI is a complex name for numerous infectious diseases that are caused by viruses and bacteria. Often, an infection can be contracted from another person, either through airborne droplets or through the use of household items (towel, clothing, dishes, etc.).

Often, a respiratory viral infection can be contracted through airborne droplets.
That is why pregnant women can be given the following recommendations to help prevent the disease:
- Limit communication with strangers on the street, at work, on public transport, especially during a flu epidemic.
- Wear a medical bandage if you are going to visit a clinic, where there are already quite a lot of people with ARVI, influenza and other infections.
- Do not take other people's household items.
- After going outside, be sure to wash your hands with soap.
- If you were near a person who coughed or sneezed, you should take measures to prevent ARVI so that the germs do not have time to spread inside the body.
We also recommend: ARVI in the last weeks of pregnancy
Top medications to reduce abdominal pain during pregnancy and breastfeeding, painkillers
Painkillers are not advisable during pregnancy. Especially in the first months, when the main formation of organs and tissues of the future person occurs. However, the process of experiencing discomfort caused by constant negative factors also does not bode well.
Before purchasing analgesics, consultation with a specialist is required. It is advisable to try non-pharmaceutical ways to cope with discomfort.
The least dangerous drug is Paracetamol. Suitable for use throughout the entire gestation period. Toxic components are in minimal concentration and are quickly excreted in the urine.
Ibuprofen is a non-steroidal anti-inflammatory drug. Prescribed with caution during the second trimester. Contraindicated for the first and third trimester. Use may cause a number of dangerous side effects. If your condition changes slightly for the worse while taking an analgesic, you should inform your doctor.
Indomethacin also belongs to the group of non-steroidal anti-inflammatory drugs. It is subject to the same restrictions as Ibuprofen. If taken continuously, there is a risk of damage to the child's kidney function.
For the first two trimesters, it is permissible to use creams and ointments based on:
- Diclofenac.
- Ketoprofen.
- Ketorolac.
In the third trimester, you can only use local products based on herbal ingredients. It is forbidden to apply them if they contain bee or snake venom.
Ointments with an irritating effect that stimulate increased blood circulation can also have a negative effect. There is a risk of developing uterine tone and high blood pressure.
The most powerful painkillers are classified as narcotic substances and are prohibited for free sale. Their use occurs only in a hospital with extremely severe pain. These are drugs based on morphine and codeine.
The list of chemical compounds for pharmaceutical use during pregnancy is extremely limited. Before you start taking it, you should read the instructions for use in detail and strictly follow the manufacturer’s recommendations on dosage and method of use.
It is important to familiarize yourself with the provisions on common side effects and contraindications.
It is possible to use folk and non-traditional methods of getting rid of suffering. For example, yoga for pregnant women, acupuncture, light massage, aromatherapy. Traditional methods are also used. But their use also needs to be discussed with a specialist.
Diet at the twenty-third week of pregnancy

During pregnancy, it is necessary to eat nutritiously and correctly, as both doctors and authors of books for expectant mothers say. But what does this mean - fully and correctly? How to eat at 23 weeks pregnant?
What you can't eat
A number of foods that are undesirable to eat: fast food, semi-finished products, all kinds of crackers and chips stuffed with harmful additives. They will be of no benefit to either mother or baby.
While waiting for the baby, you should give up foods and drinks that may be your mother’s favorite:
- coffee and strong tea, as they destabilize blood pressure;
- sushi and uncooked meat products are potential causative agents of intestinal infections and toxoplasmosis;
- blue cheeses - they affect the microflora of the intestines and vagina;
- citrus fruits are potential allergens;
- whole milk - it can cause constipation.
Do not overindulge in baked goods and sweets, carbonated drinks, salty and spicy foods.
What you can eat
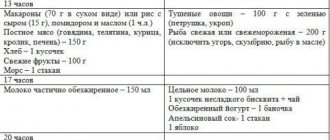
What does the approximate daily diet of an expectant mother look like at 23 weeks of pregnancy?
| Meal time | Products, dishes |
| first breakfast | glass of yogurt and banana |
| lunch | boiled egg and a portion of buckwheat porridge, tea |
| dinner | vegetable soup with chicken broth, stewed vegetables, steamed meat cutlet, compote |
| afternoon tea | fruit salad |
| dinner | cottage cheese casserole, tea with milk |
| snacks | nuts, fruits, dried fruits |
The calorie content of the daily diet should be about 3000 kilocalories, and when carrying twins or triplets - another 200-500 kilocalories more. The basis of nutrition at 23 weeks is complex carbohydrates (cereals, cereals, pasta), preferably vegetable fats, proteins (lean meat, legumes, nuts), as well as dairy products, sources of protein and calcium. Don’t forget about water: you need to drink about 1.5-2 liters per day, it’s not worth it anymore, it’s dangerous due to swelling.
Supplements, vitamins
A doctor can advise whether the expectant mother should take pharmaceutical vitamins. If a woman’s nutrition is complete, it is quite possible that her body does not experience a deficiency in vitamins and minerals. However, often, most pregnant women experience a lack of:
- gland;
- iodine;
- calcium.
The problem can be solved by taking vitamin and mineral complexes for pregnant women. Every pharmacy is ready to offer such supplements for every taste and budget.
Is it possible to drink alcohol?
If suddenly at 23 weeks the expectant mother drank a glass of wine, it will not cause much harm to the baby. However, this is true when alcohol is not a systemic phenomenon. With regular consumption of alcohol-containing drinks, a woman runs the risk of giving birth to a child with serious pathologies of internal organs, external deformities, disruption of the central nervous system and brain (even mental retardation).
When drinking even a small dose of alcohol, it is worth remembering: the single blood flow of mother and fetus will deliver “degrees” to the baby too!
In general, the 23rd week of pregnancy does not bring much concern to a woman. The baby is growing, actively reminding herself of herself with pushes, and the mother herself is still full of strength and energy. Good nutrition, adequate sleep, moderate physical activity and an abundance of positive emotions - all this will help make the period of waiting for the baby unforgettable and joyful.
Preventive measures to avoid abdominal pain
The basis of prevention is the correct lifestyle of a pregnant woman:
- No stress factors. The mental state of the mother is the key to the health of the child. The fetus inside a woman reacts sensitively to changes in the mother’s emotional background. He is not able to recognize the causes of depression or fears, but he is aware that adverse events are occurring. If the mother is very worried, there is a risk of pathological changes during the formation of the future person. Neurological and psychological problems are possible.
- Elimination of physical fatigue. Pregnant women are not recommended to attend training regularly. During active sports, blood pressure levels increase noticeably. This will provoke the development of uterine tone, which will inevitably lead to adverse consequences. You can go for walks in the fresh air.
- Properly designed diet and nutrition schedule. It must be balanced. You should not consume fast food products or preservatives; it is recommended to reduce the amount of tea and coffee. It should consist of vegetables, fruits, animal and plant protein. It is worth taking vitamins prescribed by a doctor for those who are pregnant. Weight control is required, since the percentage of subcutaneous fat outside the normal range negatively affects the functioning of the cardiovascular system and gastrointestinal tract. The feeding processes of the fetus are disrupted. With rapid weight gain, nutritional correction and a special diet may be prescribed. Excess weight contributes to decreased activity, bad mood, and additional pain in the back and joints. Make sure there is no overeating.
- Maintaining a sleep and rest schedule ensures that a woman is highly active. She does not feel tired and overwhelmed, which means she has a positive morale.
- Regular observation by an obstetrician-gynecologist according to the established schedule, passing mandatory tests, compliance with received medical recommendations. Undergoing developmental ultrasound examinations and other diagnostic measures.
- Tracking the development of chronic pathologies that were diagnosed before pregnancy.
- Prompt treatment of colds, bacterial and viral diseases acquired during pregnancy.
- Eliminate all bad habits, such as alcohol, smoking, and drug use. Failure to comply with this rule results in a developmental delay in the baby.
- Monitoring blood pressure for hypertension (high blood pressure) or hypotension (low blood pressure). Monitor your sugar levels if you are diagnosed with diabetes.
- Do not take a hot bath or shower, or a contrast shower. A sharp change in ambient temperature threatens a rise in pressure and disruption of the cardiovascular system.
Compliance with these rules will ensure comfortable and proper pregnancy. The pain will be considered obstetrically safe. But even if you follow all the recommendations, you need to carefully monitor your own condition and, if there are reasons, seek medical help.
Pain
By the 22nd week of pregnancy, when the center of gravity shifts due to an increasingly growing belly, a common problem is pain in the back and lower back, in the abdominal area, or more precisely, in the hip area. Again, due to a shift in the center of gravity and in the process of preparing the body for the upcoming birth, pain in the pelvic area is also possible - the hip joints begin to soften so that in the future the fetus can pass through the birth canal. To relieve back pain and reduce abdominal pain, wear a prenatal bandage, do not walk in heels, do not sleep on your stomach, do not stand for a long time, learn to lie and sit correctly.
More on the topic
Fetal development at 12 weeks of pregnancy
Brown discharge in early pregnancy
When can you feel the first fetal movement during your second pregnancy?
What to do if you have a small belly during pregnancy and it doesn’t grow?
Discharge during pregnancy
In the second half of pregnancy, if this has not been observed before, cramps of the calf muscles may occur from time to time. More often, leg cramps occur at the end of the day that a woman has spent on her feet. This is a symptom of tired legs and calcium deficiency. To reduce the risk of cramps, it is advisable to massage your legs every night, regularly rest your legs during the day, and enrich your diet with calcium-containing foods.
But headaches at 23 weeks of pregnancy may already disappear into oblivion. Headache is a very common companion during the first trimester of pregnancy. And, if this symptom did not bypass you in your first weeks of bearing a baby, now that the riot of hormones has subsided somewhat, the headaches should go away.
What does sudden abdominal pain mean?
The suddenness of the development of pain is a sign of an acute form of pathology. If the sensation is localized on the right side, accompanied by nausea, vomiting, dizziness, there is a risk of developing inflammation of the appendix.
Immediate hospitalization and surgical intervention are required before perforation begins. Removing appendicitis is a common procedure for surgeons. It passes without complications.
During pregnancy, the operation is performed in compliance with all required patient safety criteria.
Non-obstetric types of pathological pain of a sudden acute nature include:
- intestinal obstruction;
- peritonitis.
As with appendicitis, acute pain accompanied by vomiting and general weakness. The syndrome extends to the lower abdomen, lower back, sacrum, and groin.
Unilateral, accompanied by bleeding from the vagina - a sign of ectopic pregnancy.
Additional signs of a dangerous condition:
- cramping character;
- increased symptoms in a horizontal position of the body;
- severe vomiting;
- shortness of breath at rest;
- frequent heartbeat, which in frequency goes above 100 beats per minute.
In the absence of medical attention, the fallopian tube ruptures. Internal bleeding begins.