The baby has just been born, and everything is no longer as colorful and fabulous as depicted in the pictures. Crying loudly, chin shaking, eyes rolling up. And the first thing parents do is show the baby to a specialist.
And in principle, the approach is correct, if not for one “but”. A specialist in our country cannot say that this will all go away on its own.
You came for a diagnosis, and not for the phrase that everything is fine with you and will pass with age. That’s why the doctor gives a popular definition for any unusual behavior in the baby – increased ICP.
How to determine whether a baby really has increased intracranial pressure (ICP), which symptoms are real, which are far-fetched, and how to treat it? And is it necessary to treat at all? Let's look into all the details of such a frightening diagnosis together!
What is intracranial pressure
To understand this term as it is, you need to know the basic anatomy and physiology of the brain. Or more precisely, to understand where this intracranial pressure comes from.
The spinal cord contains choroid plexuses that produce cerebrospinal fluid, also called cerebrospinal fluid. This fluid flows into the cavity in which the brain is located, washing the main “thinking” organ. It contains essential nutrients, hormones and other compounds that regulate brain activity and vital functions. Having done its job, the liquor must go somewhere. And it flows into the venous sinuses. As waste material to be recycled.
The flow and flow of cerebrospinal fluid into the cranial cavity, washing the brain along the way, forms normal intracranial pressure. This is an unstable value. Blood pressure can rise and fall within acceptable limits; such fluctuations do not affect the baby’s well-being in any way.
Increased intracranial pressure is a pathology . This diagnosis occurs when too much cerebrospinal fluid enters the brain cavity, or the cavity has decreased due to an increase in the volume of the “thinking” organ, or the normal outflow of fluid is somehow hampered. This is a serious diagnosis that requires immediate neurosurgical intervention.
If the child is active, eats, screams, is capricious, his lip is trembling, or there are some other nervous signs that worry the parents, an ordinary neurologist often diagnoses ICP. But in this case, it is a fictitious disease that has nothing in common with the definition described above. This is a diagnosis for parents, because if this were true, the child would be in intensive care in a completely different condition and with completely different clinical signs.
Why do children have increased intracranial pressure?
Intracranial pressure is more a symptom of another disease than an independent disorder. Anatomically, its cause lies in the level of cerebrospinal fluid (CSF) and its effect on parts of the brain. Liquor is constantly produced by the blood vessels of the brain and then absorbed into the blood. When this ratio is violated, then this pathology occurs.
It can appear in the womb or during childbirth:
- abnormalities of brain development, cerebrospinal fluid outflow tracts;
- intrauterine infections;
- early closure of the fontanel (normally it closes at 12-18 months);
- hydrocephalus;
- birth trauma, hematoma resulting from severe childbirth;
- acute hypoxia causing cerebral edema.
In such cases, pathology is detected during pregnancy or immediately after birth. If a disorder is detected in time, it can be corrected and gives the child the opportunity to fully grow and develop.
Pressure disorders in the brain may appear later in life due to:
- head injuries of varying severity, hemorrhage;
- tumors of any nature;
- inflammation in the brain (encephalitis, meningitis);
- bleeding disorders;
- severe intoxication causing cerebral edema (alcohol, drug, drug poisoning);
- consequences of brain surgery in the form of adhesions.
Sometimes it occurs as a temporary phenomenon in children under 2 years of age. Intracranial pressure decreases and increases within normal limits. It is caused by changes in cerebral vascular tone when:
- severe stress, prolonged crying;
- weather change;
- excessive physical activity.
Signs of intracranial pressure (ICP) in infants
Now we will analyze a set of real signs of increased ICP in infants. This is the case when pathology actually occurs. The main symptoms of this condition in infants are:
- divergence of the sutures of the skull;
- protrusion of the fontanel;
- a sharp increase in head circumference.
In addition, there is a whole complex of symptoms characteristic of increased intracranial pressure for children at any age, not only infancy:
- disorders of consciousness and behavior;
- Strong headache;
- constant nausea and vomiting;
- convulsions;
- visual impairment;
- swelling of the optic discs diagnosed by an ophthalmologist.

It is important to understand that each symptom in itself is not a sign of ICP in a child, even an infant or any other age. Only a complex of these phenomena can indicate the presence of such a serious pathology.
Intracranial pressure in children: signs and anti-signs
If some specialist in a clinic offers you to measure a child’s intracranial pressure using some kind of device, do not agree. In reality, modern medicine knows only 2 ways to measure intracranial pressure, and both of them involve opening the skull.
However, there are some external signs that may indicate that the baby has increased ICP (which in turn, as we have already said a good hundred times, may be a symptom of one of the dangerous diseases).
In infants and children up to one year old, the main signs of increased ICP are:
- Exceeding the norms for head circumference growth;
- “Bulging” of the fontanel (when it does not tighten as it should, but, on the contrary, bulges out);
- Divergence of the skull bones;
How to correctly measure the circumference of a baby's head?
To find out the true circumference of the baby's head, you should place a flexible ruler (a tailor's meter will do) strictly above the eyebrows - in front, and at the highest point of the back of the head - in the back.
Left: an example of how to use a ruler incorrectly - it should not lie on the hairline, and not on the forehead, but strictly above the eyebrows. Right: the correct position of the ruler on the back of the head - clearly on its most protruding area.
On average, the head circumference of newborn babies is 34 cm, and then increases (on average!) by 1 cm every month. That is, during the first year of life, the baby’s head gains about 12 cm.
It is very important to know: none of the listed signs of increased intracranial pressure are obvious reasons for making a diagnosis of “increased ICP.” Symptoms must appear in complex and be supported by subsequent studies - for example, ultrasound of the brain and others.
Remember, symptoms of increased intracranial pressure are NOT:
- Delayed closure of the fontanelle;
- Any developmental delays (“late” began to roll over, sit up or walk, is silent, does not speak, etc.);
- Walking on tiptoes;
- Nosebleeds;
- Trembling, shaking, or tremors (of arms, legs, or lips);
- Hyperactivity syndrome;
- Sleep or appetite disturbances;
Causes
High intracranial pressure itself is not a disease, but a symptom of it. An increase in ICP indicates that there is a failure in the flow of cerebrospinal fluid. This happens with pathologies such as:
- Brain tumors (benign and malignant). In this case, due to the appearance of a neoplasm in the skull, the pressure increases. After all, the intensity of the flow of cerebrospinal fluid does not change, as well as its outflow.
- Meningitis of any type. In this case, the volume of the brain increases due to swelling of its tissues. This also increases the pressure inside the skull. In the case of purulent meningitis, the density of the cerebrospinal fluid also changes, making its outflow significantly more difficult.
- Encephalitis of any etiology. In this case, we have inflammation of the brain, which is also accompanied by edema and increased ICP.
- Toxic cerebral edema. In this case, the main “thinking” organ swells due to the action of toxins, which also leads to high pressure on the skull.
- Hydrocephalus. This disease is also called hydrocele in newborns. In this situation, the outflow of cerebrospinal fluid is disrupted, but at the same time, the rate of its entry remains the same, which is why the pressure increases.
- Genetic abnormalities of the cerebrospinal fluid pathways. Because of this, hydrocephalus appears with all the ensuing consequences.
- Traumatic brain injuries. As a result of such damage to the skull, cerebral edema may occur, and hematomas may form, which also affect ICP.
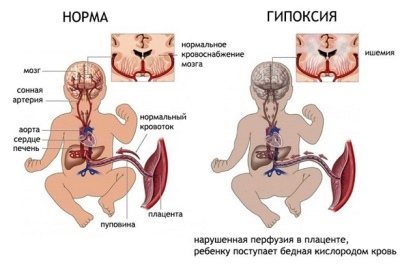
- Postpartum cerebral edema. In this case, the brain tissue swells due to birth pathologies. One of the reasons is acute hypoxia in newborns, which develops during prolonged labor.
- Early fusion of the skull bones. In this case, the bones of the skull have already fused together, while the “thinking” organ is only increasing its growth rate. There is not enough space for it, so the pressure inside the skull increases sharply.

Reasons for the increase
There are many provoking factors that contribute to increased cranial pressure. It is no coincidence that neonatologists are noting more and more cases of such a syndrome occurring after the birth of babies. Every day hundreds of babies are born around the world who have congenital intracranial hypertension.
The following reasons lead to increased cranial pressure in newborns and infants:
- Anomalies in the structure of the placenta. Through this vital organ, essential nutrients reach the baby throughout the 9 months of pregnancy. Defects in the structure of the placenta or feeding blood vessels lead to the development of venous outflow disorders in the fetus. After birth, this condition is manifested by the development of intracranial hypertension.
- Pathologies that arose during childbirth. Incorrectly chosen surgical tactics or unexpected complications can lead to traumatic brain injuries to the baby. Often such impacts also lead to damage and micro-tears of the meninges. If the cerebral ventricles or cephalic veins are damaged, the symptoms of intracranial hypertension in the baby increase several times.
- Intrauterine infection . The most dangerous are the 1st and 3rd trimesters of pregnancy. Viruses and bacteria that penetrate the body of the expectant mother at this time very easily pass through the hematoplacental barrier. Entering the child’s body through the bloodstream, they can cause damage to the brain, which in some cases contributes to the development of intracranial hypertension in the baby after birth.
- Traumatic injuries. When a child falls and hits his head, he often experiences various damage to the meninges, as well as injuries to the anatomically closely located cervical vertebrae. Such traumatic defects significantly impair the outflow of cerebrospinal fluid from the brain to the spinal cord. Ultimately, this contributes to the development of intracranial hypertension in the baby.

- Neoplasms. Occur no more often than in 1-2% of cases. Actively growing tumors in the brain significantly compress the cerebral ventricles. This leads to impaired outflow of cerebrospinal fluid and the development of hypertension syndrome.
- Hemorrhages in the brain. In newborn babies they often occur with massive traumatic brain injuries. In some cases, they can be congenital, resulting from increased fragility of the feeding vessels due to hemorrhagic vasculitis.
- Inflammatory diseases of the brain. Infectious meningitis leads to impaired venous outflow, which contributes to the development of intracranial hypertension.
All causes contributing to the development of intracranial hypertension cause severe hypoxia of the brain.
This condition is characterized by insufficient oxygen supply and increased carbon dioxide levels in the body. Prolonged oxygen deprivation contributes to disruption of brain activity and leads to the appearance of adverse symptoms characteristic of this condition.
Diagnostics
The only way to find out the exact readings of intracranial pressure in a baby is a spinal tap. Only this method provides digital confirmation of the diagnosis of ICP. The baby is first examined by a neurologist, studying the medical history and the current condition of the young patient. Then the child is examined by an ophthalmologist, examining the fundus of the eye using a special device. This is done to confirm the neurologist’s concerns.
Another diagnostic method is neurosonography. This is an ultrasound for the brain. Such a study allows us to identify the presence of any neoplasms in the baby’s head. However, such a study gives results only in newborns whose fontanelles are still open.
Remember , if a neurologist looked at your child with one eye, listened to your complaints and wrote “ICP” in the medical history, this does not mean anything.

Only a comprehensive and specialized examination of the baby by multidisciplinary specialists can confirm such a terrible diagnosis. If you are not sent anywhere else, it means that everything is fine with you and will pass over time, you don’t need to worry more than you should.
Treatment of intracranial pressure in infants
First of all, experts find out what caused the real increase in ICP in the baby. The further set of measures depends on success in eliminating this very cause.
If the pathology is caused by neoplasms in the skull (tumors, hematomas), these same formations are removed surgically. If the cause is excessive production of cerebrospinal fluid, an operation is performed to improve its outflow.
The second stage of treatment is aimed at eliminating the consequences of the pathology. ICP is adjusted:
- osmodiuretics;
- loop diuretics;
- hormone therapy;
- neuroprotectors.
The next step may be medical procedures to remove excess cerebrospinal fluid from the skull. For this purpose, punctures and craniotomies are used.
When the child’s condition is stabilized, the mother is recommended a diet in which she should consume less liquid and limit as much as possible the intake of salt into the body, and, accordingly, into mother’s milk.
In any case, treatment measures are complex. This pathology is eliminated exclusively in the operating room, often in intensive care, under the round-the-clock supervision of medical personnel.

Signs of intracranial pressure in infants Komarovsky
It is simply impossible to imagine a woman interested in children's health issues who has not heard of intracranial pressure - ICP.
A doctor’s attempt to approach the problem of intracranial pressure competently, in a modern way, and to treat it like in the best clinics in the world cannot be implemented. Because the epidemic of ICP treatment that has swept the CIS countries is limited to these countries. That is, our overseas friends are somehow disconnected from this topic - either they misunderstand and do not care about the neurological health of children, or they do not diagnose it, or their children are different?
There must be something wrong here: how can there be a disease that pediatric neurologists in our clinics detect in at least 50% of children (this is the most optimistic figure), and at the same time a disease that is completely absent outside the CIS .
No, the phrase ICP exists, its increase is discussed in scientific articles, moreover, tactics to combat this very dangerous phenomenon are being studied, but the list of conditions accompanied by an increase in ICP is very small, and these are increasingly such terrible horror stories that can be easily made conclusion: having an increase in ICP, you can sooner end up in the intensive care unit than wait in line for an appointment with a pediatric neurologist at the district clinic.
That is, globally, here and there, the approaches to ICP are fundamentally different: there it is a very rare, very dangerous (life and health threatening) condition, usually requiring hospitalization and emergency care, but in our country it is an extremely common disease, easily diagnosed, almost always easily treatable and almost always on an outpatient basis.
No, something is definitely wrong here. And it seems that we need to figure it out: either we don’t understand something, or we are being misled together, or our children are special - not like those in the rest of the world. Since the last statement seems extremely unlikely, and you don’t really want to be lost and misunderstood, let’s consider the topic slowly and in order.
So, what is ICP and where does it come from? What is the pressure on what and how does it all come out?
In the cranial cavity there is a brain, there is blood, there is a special fluid called cerebrospinal fluid (synonymous with cerebrospinal fluid). Liquor is formed from the blood in special choroid plexuses, circulates, washing the brain and spinal cord, after which it is again absorbed into the blood through special venous sinuses. Liquor performs a number of important functions; without these functions, normal brain function is simply impossible.
Liquor does not stand still, but just like blood, it moves all the time. There are vessels for blood movement. For the movement of cerebrospinal fluid, there are special anatomical cavities - the ventricles of the brain and the spinal canal.
This is, so to speak, elementary, or, to be more precise, superficially primitive anatomical and physiological information.
But now we can understand where intracranial pressure comes from. So, a certain liquid is constantly being formed and is constantly being absorbed. You probably already remembered school mathematics with problems about a swimming pool and two pipes - the same is true with liquor. It flows out of one pipe (choroid plexuses), and flows into another pipe (venous sinuses). While it flows, it puts pressure on the walls of the pool (the inner surface of the ventricles of the brain and the spinal canal).
That's all, actually.
Now for some obvious conclusions.
Another question is that a specific figure indicating the value of ICP in a specific period of time is not a stable concept, which, in fact, follows from the fact that ICP changes all the time. Both the formation of CSF, and the speed of its movement, and the activity of absorption depend on many factors: whether the child is sleeping or awake, lying, sitting or standing, silent or screaming, normal body temperature or elevated, and in general what the temperature around is - comfortable, or hot, or Cold. The connection between the level of ICP and all of the above parameters does not seem obvious at first glance, but an elementary illustration: if the room is hot and the child is actively sweating, blood thickening occurs, as a result, the rate at which the choroid plexuses produce cerebrospinal fluid decreases. It is clear that many manifestations of a wide variety of diseases will, in turn, affect the level of ICP - vomiting, coughing, prolonged crying, painful sitting on the potty due to constipation, and much, much more.
Consequences
It is important to understand that if ICP is not a far-fetched diagnosis, but a very real one, it absolutely cannot be ignored. This condition is unpleasant in itself, but if the problem is ignored, a sharp increase in pressure inside the skull is possible. Without qualified and timely medical care, this leads to death.
In addition, such a difficult diagnosis may subsequently be accompanied by other complications:
- Infringement of the cerebellum. This pathology is accompanied by impaired respiratory function, weakening of the legs and arms, and disorders of consciousness.
- An epileptic syndrome that can stay with the child for life.
- Decreased vision, blindness. This occurs due to pinching of the optic nerve.
- Mental dysfunction.
- Strokes of ischemic and/or hemorrhagic nature.

Prevention
This pathology can be prevented in infants only by proper preparation for pregnancy. If the mother is healthy, did not abuse anything during the process of bearing a new life, and behaved correctly during the birth process, the likelihood of such a pathology in the baby is minimal.
Screening studies for genetic abnormalities during fetal growth and development should not be neglected. Of course, you should not drink alcoholic beverages, smoke or take drugs, or any medications during pregnancy.
In addition, it is important to pay attention to the baby’s health after birth. Walk more, eat well, do children's gymnastics. Protect your child from hypothermia and overheating, viruses, and get vaccinated in a timely manner.
In essence, the prevention of ICP comes down to preventing the pathologies of which this condition is a symptom. But it is important to understand that no dietary supplements, homeopathic remedies or any other magic pills will help. Only a healthy lifestyle and proper attention to the child will protect against the arrival of such a disaster in your home.









