Perinatal encephalopathy is a group of diseases associated with damage to the brain, often of hypoxic-ischemic origin. Pathology is detected in newborns, which means that damaging factors affect the nervous tissue during intrauterine development, childbirth, or in the first week of a baby’s life. In 90% of cases, mothers of newborns with diagnosed PEP have a complicated medical history (threat of miscarriage, toxicosis in the first and second trimesters, premature birth).
Characteristic
Encephalopathy is a medical term that means damage to the brain substance of non-infectious origin. Perinatal is a word that means that this period of time includes the period from the 22nd week of gestation to the 7th day of the baby’s life. The perinatal period includes antenatal (from 28 weeks before birth), intranatal (childbirth), neonatal (from birth to 7 days of life) periods. During the neonatal period, the newborn adapts to new external conditions.
Perinatal encephalopathy (PEP) in children is a pathology that reflects damage to the brain matter, which occurs against the background of various pathological processes. PEP in newborns is a group of diseases that imply structural, morphological or functional disorders of the brain.
The disease perinatal encephalopathy is not identified as a separate code in ICD-10. However, a similar diagnosis is found in pediatric practice for children under one year of age who have neurological disorders, including motor and mental disorders. After 1 month of the newborn’s life, a neurologist, based on neurological symptoms and based on the results of an instrumental examination, makes an accurate diagnosis indicating the etiological nature of the pathology.
The prevalence of perinatal encephalopathy reaches about 700 cases per 1 thousand newborns. Infants receiving hospital treatment are given a primary or concomitant diagnosis of PEP in 90% of cases. Clinical studies show that in most cases the diagnosis is not true. The doctor often indicates this pathology if he has not found out the causes of the syndrome of motor and other neurological disorders.
Studies by foreign authors provide other figures that more objectively reflect the prevalence of the disease - about 6 cases per 1 thousand full-term newborns, about 33-70% of cases among premature infants. Diseases combined into the AED group are presented in ICD-10 under the codes “G51.0, 51.8”, “G90.9”, “G91.0-91.2”, “G91.8”, “G93.2”.
Causes
The intrauterine development of the brain and nervous system as a whole is influenced by various unfavorable factors, in particular the health of the mother and the state of the environment.
Complications can also arise during childbirth.
- Hypoxia. When a child in the womb or during childbirth lacks oxygen, all body systems suffer, but primarily the brain. The cause of hypoxia can be chronic diseases of the mother, infections, incompatibility by blood group or Rh factor, age, bad habits, polyhydramnios, malformations, unsuccessful pregnancy, unsuccessful childbirth and many others. More about hypoxia→
- Birth trauma causing hypoxic or mechanical injuries (fractures, deformations, hemorrhages). Injury can be caused by: weak labor, rapid labor, poor fetal position, or obstetrician error.
- Toxic lesions. This group of reasons is associated with bad habits and the intake of toxic substances during pregnancy (alcohol, drugs, some medications), as well as with environmental influences (radiation, industrial waste in air and water, heavy metal salts).
- Maternal infections - acute and chronic. The greatest danger is posed by infection of a woman while carrying a child, since in this case the risk of infection of the fetus is very high. For example, toxoplasmosis, herpes, rubella, and syphilis rarely cause symptoms of an infectious disease in the fetus, but cause serious disturbances in the development of the brain and other organs.
- Developmental and metabolic disorders. These can be congenital diseases of both mother and child, prematurity of the fetus, and developmental defects. Often the cause of PEP is severe toxicosis in the first months of pregnancy or gestosis in the last.
The above factors can cause various types of disease. The most common are the following:
- hemorrhagic form, caused by bleeding in the brain;
- ischemic, caused by problems with blood supply and oxygen supply to brain tissue;
- dysmetabolic is a pathology of metabolism in tissues.
Classification
Classification of perinatal encephalopathy in newborns is carried out taking into account etiological factors. Depending on the dominant damaging factor, the following forms are distinguished:
- Hypoxic, caused by oxygen deficiency.
- Traumatic, associated with mechanical damage to the fetal brain.
- Toxic-metabolic, correlating with metabolic disorders and toxic effects.
- Infectious, caused by infectious and inflammatory processes.

Hypoxia plays a leading role in the structure of the causes of PEP. Toxic effects and infectious processes, in addition to direct damaging effects on nervous tissue, provoke disruption of the uteroplacental circulation, which leads to the development of intrauterine hypoxia, which occurs in a chronic form. Against the background of oxygen starvation, ischemia of the nervous tissue develops.
Injuries received by the fetus during labor are associated with mechanical damage to brain structures and often lead to impaired blood circulation in the vertebrobasilar system, which affects the aggravation of hypoxic-ischemic processes. In case of unfavorable course of pregnancy and childbirth, hypoxia becomes a universal damaging factor that provokes the development of PEP.
Diagnostic methods
Perinatal encephalopathy in children is a serious problem. To make a diagnosis, the presence of symptoms is taken into account during a routine examination or taking into account the stories of parents.
The diagnosis is made based on:
- Assessment of the mother's life history and the child's existing illness. They also collect information about all unfavorable factors that could affect the fetus during intrauterine development.
- Symptoms and syndromes that indicate this group of diseases.
- Movement disorder syndrome in the form of increased or decreased muscle tone.
- Increased neuro-reflex excitability.
- Suppression of the functions of the Central nervous system.
- Increased pressure inside the skull. In this case, the fontanel enlarges and bulges, the head circumference increases, and the cranial sutures diverge.
- Convulsive attacks.
- Prenatal diagnosis, which includes ultrasound to determine umbilical cord entanglement, abnormal fetal position, Doppler ultrasound to determine vascular abnormalities and abnormalities in cardiac development.
- Neurosonography, during which ultrasound is used to identify the location of hemorrhages.
- Encephalography. The procedure is necessary to evaluate pathological waves and disturbances in brain activity.
Based on the information received, the doctor selects the appropriate treatment method. At home, parents should also continue restorative procedures.
Causes
PEP in newborns is a diagnosis that is characterized by damage to the brain matter, which negatively affects the functions of the central nervous system. The main causes of the disease are associated with the damaging effects of pathological factors and processes:
- Fetal hypoxia (oxygen deficiency) – intrauterine, intrapartum.
- Mechanical injuries to the fetus during childbirth.
- Infectious and viral lesions of the fetus.
- Toxic effects on the fetus.
- Hereditary predisposition.
PEP of mixed origin is more often diagnosed, which suggests the participation of several factors in the pathological process. Perinatal pathology of hypoxic origin is a common form, which is characterized by damage to the tissues of the nervous system due to oxygen starvation.
Hypoxia is accompanied by a complex of disorders that affect the rheological properties of blood, hemodynamics and microcirculation, and affect metabolic processes. As a result, damage to the nervous tissue occurs due to hemorrhagic infarction and ischemia.
Against the background of ischemic processes, leukomalacia subsequently develops - damage to the white brain matter. Perinatal encephalopathy is a pathology that occurs against the background of diseases and adverse effects aimed at pregnant women, which is often associated with the following reasons:
- Somatic diseases accompanied by the effects of intoxication suffered by the mother during gestation.
- Infectious diseases (new forms or exacerbation of chronic infections) suffered by the mother during gestation.
- Immaturity of the body of a woman carrying a fetus.
- Poor nutrition, causing a deficiency of vitamins and other nutrients.
- Hereditary diseases in the mother.
- Metabolic disorders.
- Unfavorable environmental conditions, harmful external influences (air and water pollution with toxic substances, ionizing radiation).

Among the factors that provoke the development of perinatal hypoxic-ischemic encephalopathy, it is worth noting the pathological course of pregnancy (threat of miscarriage, toxicosis) and childbirth (injury to the child due to the use of auxiliary instruments, slowdown of labor, rapid labor).
What is perinatal encephalopathy?
Medical literature gives the following definition:
Perinatal encephalopathy, or PEP, is a group of brain lesions of various etiologies and development mechanisms that occur during the perinatal period.
In more understandable terms, perinatal encephalopathy is a group of brain diseases caused by various causes. PEP occurs during the perinatal period, that is, from the 28th week of pregnancy to the 7th day of life in full-term babies, and up to 28 days in premature babies. Depending on the mechanism of occurrence, specific types of AEDs are distinguished - hypoxic, traumatic, toxic-metabolic or infectious.
According to statistics, from 3 to 5% of newborns are born with signs of perinatal encephalopathy. Perinatal encephalopathy is a common pathology. It is not a sentence at all; you can and should work with it.
Why does the disease develop?
The main and most common cause of perinatal encephalopathy in newborns is the negative impact of various harmful factors on the mother’s body during pregnancy. These factors include the following:
- acute infectious diseases of the mother during pregnancy, as well as chronic diseases of the mother with exacerbation during pregnancy;
- violation of the mother's diet during pregnancy and breastfeeding;
- pathology of labor (weakness, rapid labor) or trauma during childbirth (fractures, atypical position of the fetus);
- toxicosis (both early and late);
- insufficient maturity of the mother’s body, too young age;
- threat of miscarriage;
- various hereditary genetic diseases, as well as congenital metabolic disorders;
- adverse effects of harmful environmental factors - toxic substances, radiation, harmful substances in food, heavy metal salts, exhaust gases, harmful factors at work, industrial waste in water and air;
- prematurity and immaturity of the fetus, congenital malformations;
- bad habits of mother and father: smoking, drinking alcohol, drug addiction, coffee abuse.
As you can see, the reasons can be any adverse effects, so future parents need to prepare in advance for the conception and birth of a child - take care of their own health first.
Types of perinatal encephalopathies
Perinatal encephalopathies are classified according to the causes that cause them. Accordingly, the following groups of PEP can be distinguished:
Hypoxic . Occurs as a result of lack of oxygen in the peripheral blood or asphyxia at birth.

Traumatic . Develops as a consequence of fetal injuries during childbirth: incorrect position, obstetric error, incorrect conditions during childbirth, pathology of labor.
Toxic-metabolic – occurs due to malformations of fetal organs, inflammatory processes in the mother during pregnancy.
Infectious , of course, implies the presence of infection.
Depending on the severity, PEP is classified into mild, moderate and severe perinatal ecephalopathy.
Depending on the mechanism of development, perinatal encephalopathies can also be hemorrhagic, ischemic and dysmetabolic. Simply put, brain damage caused by hemorrhages (hemorrhagic), lack of blood supply and oxygen (ischemic) and disturbances in metabolic processes in tissues and cells (dysmetabolic).
How to recognize perinatal encephalopathy?
Usually, obstetricians and pediatricians almost accurately recognize the symptoms of perinatal encephalopathy. But even in the absence of a qualified specialist, one can suspect PEP in a child already in the first hours after birth.
What you should pay attention to in the behavior of a newborn:
- weak or late cry;
- problems with the state of the cardiovascular system at birth - arrhythmia, absence of heartbeat, tachycardia, bradycardia;
- excessive weakness or increased muscle tone;
- inadequate reactions to stimuli (light, sound);
- reflex voluntary shudders;
- lack of newborn reflexes (sucking, swallowing, searching, etc.);
- causeless anxiety, nervous behavior;
- frequent, hysterical, hysterical-like, with frequent voice breakdowns, difficult to stop crying;
- lesions of the oculomotor nerve (strabismus, exophthalmos);
- throwing back the head when lying on the back;
- frequent regurgitation, vomiting, digestive disorders related and not related to food intake;
- sleep disorders (difficulty falling asleep, frequent awakenings).
Unfortunately, symptoms of perinatal encephalopathy often appear at a later age. This greatly facilitates diagnosis, but complicates the treatment of AEDs.

At older ages, you may notice the following symptoms:
- disorders of mental processes (memory, attention, sensation, perception, etc.);
- passivity, lack of interest in everything that is happening, apathy, lack of initiative;
- constant signs of depression - lack of appetite, depressed state, reluctance to participate in the game, make contact, fatigue, confusion, absent-mindedness, irritability, tearfulness, weakness, poor sleep, depression;
- signs of VSD – dizziness, headaches, low blood pressure;
- inability to express one's thoughts;
- lack of interest in cognitive activity (narrowing the range of interests);
- speech disorder.
As you can see, all these disorders can be combined into two groups - deterioration in general well-being and delayed mental development.
Diagnostics
Often, the diagnosis of perinatal encephalopathy is made by pediatricians who accidentally discovered symptoms during a routine examination of the child, or based on the stories of parents.
In general, a doctor will make a diagnosis of PEP based on the following indicators and studies.
- Anamnesis of the life of the mother, child and anamnesis of the disease - the presence of unfavorable factors before and during pregnancy, pathological labor.
- Clinical picture - symptoms and syndromes characteristic of this group of diseases:
- Syndrome of movement disorders - muscle hypotonia or hypertension.
- Syndrome of increased neuro-reflex excitability.
- Central nervous system depression syndrome
- Intracranial hypertension syndrome - the large fontanel is enlarged and bulging, the head circumference is increased, the cranial sutures diverge.
- Convulsive syndrome.
- Prenatal diagnosis - ultrasound (umbilical cord entanglement, abnormal fetal position), Dopplerography (pathologies of the development of the heart and vascular bed in the fetus).
- Neurosonography - ultrasound of the brain - reveals areas of hemorrhage.
- Electroencephalography – pathological waves or disturbances in brain activity.
Clinical manifestations
Perinatal encephalopathy is a pathology that manifests itself in characteristic syndromes, which suggests a similar clinical picture regardless of the leading etiological factors. Clinical syndromes:
- Increased neuro-reflex excitability.
- SDN is a complex of motor disorders (paresis - weakness of central and peripheral muscles, extrapyramidal disorders, cerebellar disorders).
- Convulsive (sudden attacks of uncontrolled muscle contractions).
- Hydrocephalic (impaired cerebrospinal fluid dynamics against the background of increased production and deterioration of absorption of cerebrospinal fluid with a subsequent increase in intracranial pressure values).
The diagnosis of PEP (stands for perinatal encephalopathy) in a child is a pathology that leads to a slowdown in mental and physical development, which is manifested by slow growth and weight gain, impaired formation of pre-speech and speech skills, and deterioration in the development of cortical functions.
Symptoms of PEP in newborns appear depending on the nosological form of the pathology. For example, with a mild form of cerebral ischemia, excitation or depression of the central nervous system is observed, which lasts no more than 7 days.
With moderate cerebral ischemia, the clinical picture is supplemented by signs: convulsions, increased intracranial pressure, disturbances in the functioning of the autonomic part of the central nervous system (impaired respiratory and cardiac activity). If cerebral ischemia is severe, the depression of central nervous system activity is progressive and lasts longer than 10 days. Severe ischemia variably leads to the following consequences:
- Going into a comatose state.
- Transformation into an excited state, accompanied by a stable convulsive status.
- Convulsions followed by coma.
It is possible to develop status epilepticus with subsequent disruption of the activity of brain stem structures that regulate vital functions (breathing, heart function). The processes of decortication and decerebration reflect destructive and atrophic changes in the nervous tissue. Symptoms of perinatal encephalopathy, which develops against the background of intracranial hemorrhage associated with hypoxia, depend on the degree of damage to the brain. With a mild form of the disease, the pathology may not manifest any signs.
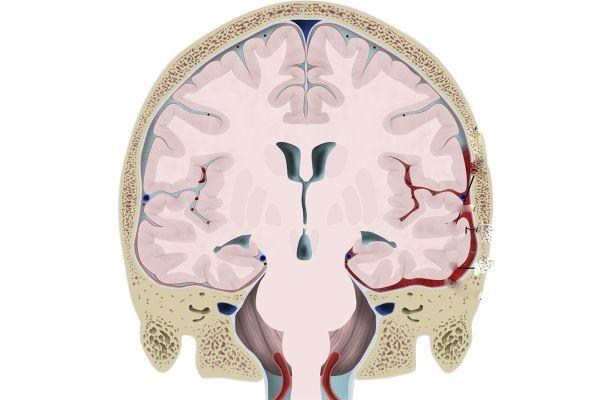
In a moderate form, signs are observed: shock, apnea (short-term stops in breathing), convulsive syndrome, confusion, depression of consciousness, development of a coma, increased intracranial pressure. Symptoms can be observed constantly or be transient (transitory) in nature. The appearance of hemorrhagic foci in the brain against the background of perinatal posthypoxic encephalopathy is accompanied by the following symptoms:
- Deterioration in general well-being, which manifests itself suddenly and leads to the development of a state of depressed consciousness, often alternating with periods of psychomotor agitation.
- Protrusion of the fontanel.
- Oculomotor disorders (abnormal movements made by the eyeballs).
- Thermoregulation disorder (hypothermia - hypothermia, hyperthermia - overheating of the body).
- Disturbances in the functioning of the autonomic system (frequent regurgitation, tachycardia - increased heart rate, tachypnea - rapid, shallow breathing, flatulence, stool upset).
- Pseudobulbar disorders (dysarthria - impaired pronunciation, dysphonia - decreased strength and sonority of the voice, dysphagia - impaired swallowing function, forced crying or laughter).
Posthypoxic encephalopathy, which occurs against the background of intracranial hemorrhages, is accompanied by anemia (hemoglobin deficiency), hypoglycemia (low glucose concentration), acidosis (a shift in the acid-base balance of the blood towards increased acidity) and other metabolic disorders. Often, somatic diseases - pneumonia, sepsis, heart failure - are associated with disturbances in the functioning of the central nervous system.
Severe clinical manifestations are a reason for inpatient treatment. If there are signs of mild damage to the brain, the child is discharged from the maternity hospital, he is at risk and is subject to medical supervision once a month. This approach often leads to a lack of therapy in the acute period. Treatment is carried out with a delay, during the period when complications of AEDs appear, which reduces the therapeutic effect.
Clinical manifestations of PEP, ICD code
According to the International Classification of Diseases (ICD), perinatal encephalopathy has code G93. Clinically, the disease is characterized by the appearance of several syndromes.
| Specific symptom complexes | Symptoms |
| Central nervous system inhibition | Lethargy, weak reflexes, lethargy, drowsiness. |
| Coma | Decreased vital functions (breathing, heartbeat), lack of consciousness, the patient’s condition is severe, there is an absence of sucking and swallowing reflexes, and convulsions. |
| High nervous excitability | Strengthening the reflexes of newborns, inhibition of motor activity, long periods of wakefulness, difficulty in putting the baby to bed, poor quality of sleep, frequent crying, screaming, twitching of the arms, legs, chin, muscle hypertonicity can be replaced by weakness. Often the clinic goes away on its own after 1 year of the child’s life. |
| Convulsions | Newborns: twitching, shuddering, muscle tension in the limbs, convulsions. |
| Hydrocephalus | An increase in fluid in the ventricles of the brain due to impaired outflow or secretion of cerebrospinal fluid. The baby has poor sleep, frequent regurgitation, an increase in head size (the norm for a newborn is 34-35 cm, normal head growth per month (in the first 6 months of life) is 1.5 cm), convulsions, screaming, pulsation, bulging of a large fontanelle . |
| Vegetative-visceral dysfunction | Poor weight gain, frequent, heavy regurgitation, arrhythmia, changes in temperature (usually newborns have poor temperature control, the reading after birth is less than 36°), change in skin color. |
| Epilepsy | Attacks of seizures during activation of a focus of hyperexcitation in the brain. There is an opinion that the lesion is more often formed due to hypoxia in utero or during childbirth, or infection. |
| Impaired mental function | Delay in the formation of skills as the baby develops (late walking, walking, speaking). Speech dysfunction in patients after 2-3 years of age. |
| Movement disorders | Decreased or increased muscle tone, hyperkinesis, tics, increased motor activity. |
Cerebral palsy may occur in the postnatal (after birth) period. The baby develops a focus of damage, which provokes the development of tonic-clonic seizures, hypertension of the flexor or extensor muscles, and atrophy of the antagonist muscles. There is a delay in speech and mental development. The disease is difficult to treat.

One of the most serious complications of PEP is cerebral palsy.
Hypoxia during childbirth or in utero can provoke hyperactivity syndrome and attention deficit in children under 5 years of age. It can be detected immediately after birth or after some time. In children, speech formation is disrupted and they lack perseverance and attention. Children are often irritable and have trouble sleeping. Over time, these symptoms may go away on their own.
Diagnostics
Immediately after birth, a physical examination of the baby is performed and an Apgar score is given. A poor prognosis correlates with persistence of an Apgar score of less than 3 points for more than 5 minutes. Unfavorable prognostic criteria: the appearance of seizures in the first 8 hours after birth, a persistent decrease in muscle tone.

Such children often subsequently develop cerebral palsy, epilepsy, and mental retardation. The diagnosis is made by a neonatologist or perinatal neurologist. Diagnostic examination and treatment are carried out in pediatric neurology departments. Basic instrumental examination methods:
- Neurosonography (ultrasound examination of tissues of the central nervous system).
- Dopplerography (determining the state of the circulatory system that supplies the brain).
- MRI, CT (study of the morphological structure and features of the functioning of the central nervous system).
- Electroencephalography (study of bioelectrical activity of the brain).
Ultrasound diagnostics in DEG format shows signs of hypoperfusion (deterioration of blood flow through the nervous tissue). An MRI study shows the presence of focal damage to nerve tissue. In severe cases, a decrease in the density of the brain matter is detected. Perinatal neurology requires a thorough differential diagnosis.
For example, hypothyroid encephalopathy develops as a consequence of hypothyroidism - a decrease in the production of thyroid hormones. The disease is manifested by symptoms such as delayed physical and mental development, decreased muscle tone, lethargy, and refusal to eat. The baby retains a large diameter of the fontanel for a long time. Such symptoms can be mistakenly interpreted as signs of PEP of a different origin.
Treatment
Modern medicine does not provide precise clinical recommendations regarding AEDs. For example, Dr. Komarovsky argues that a treatment protocol for perinatal encephalopathy cannot be developed because such a diagnosis does not exist in the civilized world. To eliminate the symptoms that appeared in a child during the postpartum period, you need to find out the exact causes of the disorders and carry out the correct therapy.
Treatment of posthypoxic encephalopathy in children and adults involves adherence to the regimen, including reducing exposure to light and sound stimuli, and organizing a nutritious diet. Regular measures are aimed at preventing hypothermia and overheating of the baby. If the newborn has no appetite, he refuses to eat, parenteral (via intravenous) nutrition is prescribed. Vital functions are constantly monitored.

Newborns who exhibit cerebral edema and a comatose state are connected to a ventilator (hardware ventilation). They are prescribed Phenobarbital (has an anticonvulsant, antiepileptic effect). In the absence of intracranial hemorrhage, diuretics (Mannitol, Lasix) are indicated. If cerebral edema progresses, diuretics are combined with corticosteroids (Dexamethasone).
In parallel, antihypoxants (Piracetam, Cocarboxylase) and antioxidants (Alpha-tocopherol acetate) are prescribed. If there are movement disorders or changes in muscle tone after the end of the acute period, massage, therapeutic exercises, physiotherapy, and water procedures are prescribed. The duration of the recovery period is 1-12 months; in premature infants, the duration of rehabilitation can reach 24 months.










