A prolonged runny nose in a baby means difficulty breathing, obstruction of the nasal passages and excess snot that does not go away for more than 2 weeks. In most cases this is not a disease. Most often, long-term nasal congestion in a newborn is a reaction to unfavorable microclimate conditions in the room, less often a reaction to various chemical compounds in the air that seem normal to adults and which they do not even notice. In this case, the baby’s runny nose does not go away until the irritants are identified and eliminated. All these problems with the nose cannot be solved with medication; it makes sense to fight them only through organizational measures.
If an infant has a runny nose that does not go away for a long time, then it is unlikely to be caused by an infection, since even severe rhinitis should go away in a week or two. Prolonged nasal congestion is usually the result of either inadequate treatment or a significantly weakened immune system. Depending on how long a runny nose lasts in an infant and what clinical picture is observed with it, not only its current cause is determined, but also the procedure for treatment.

If you have any doubts about the causes of a runny nose in a child, you should consult a doctor.
The task of parents in these cases is to distinguish the disease from a simple reaction of the child’s body to the microclimate, if necessary, normalize the microclimate parameters or consult a doctor. Note that if the problem is the microclimate, then improving it will relieve nasal congestion and sneezing in a day or two.
All the reasons for a prolonged runny nose in a baby
Based on the symptoms and clinical picture, you can often understand the cause of prolonged nasal congestion in a child and take appropriate measures:
- Immaturity of the baby's respiratory tract, their adaptation to new living conditions. For this reason, a typical physiological runny nose in newborns very often occurs. It occurs in almost all newborn children and lasts from birth until 1.5-2 months (sometimes up to 3 months or even more). It is characterized by the absence of copious liquid snot, the child feels well, has a healthy appetite, sleeps with his mouth open, and sniffles are normal for a baby. Clots of snot may accumulate in the nose, but in general the mucous membrane is normally moisturized and there are no dry crusts. Thus, if an infant’s runny nose does not go away, then it is quite possible that the airways are not formed;

With a physiological runny nose, a child may sleep with his mouth open, but this is not a cause for concern. - A reaction to unsuitable microclimate conditions - in this case, the baby’s nasal mucosa usually dries out, crusts appear, and when sneezing, dry pieces of flaking crusts fly out of the nose. For the same reason, rhinitis sometimes develops, and the child’s nose becomes blocked. This condition differs from all other causes of nasal congestion in the absence of liquid or thickened snot. With it, sometimes blood may flow from the nose if the crusts crack. A typical long-term dry runny nose in a baby is usually just such a reaction;
- The reaction to irritating substances in the air differs from the previous condition in terms of symptoms. When exposed to irritating substances, a child produces excess snot from his nose, the baby often sneezes, rubs his eyes and nose. Symptomatically, it is similar to allergic rhinitis in adults. In many cases, frequent sneezing in infants is just such a reaction to constant encounters with irritants;
- Infectious rhinitis is a disease caused by viruses or bacteria. It is rarely protracted, and if it is prolonged, it is either due to complications or due to improper treatment. Viral rhinitis differs from other types of rhinitis by an increase in the child’s body temperature and general severe malaise, lack of appetite, and bacterial by the presence of abundant thick green or purulent snot;

If your child's body temperature rises, you should immediately consult a doctor. - Drug-induced rhinitis is a consequence of illiterate treatment and violation of the rules for using medications. It is characterized by constant nasal congestion in the child, drying out of the mucous membrane and lack of response to the use of medications.
On a note
Physiological runny nose almost always goes away by 3-4 months. In a six-month-old baby, this condition will no longer be observed.
Allergic rhinitis in infants is extremely rare, unlike food allergies. We have already talked about this in more detail. For now, we just note that this is the disease that is least likely to be suspected in an infant. In any case, its symptoms are similar to those for the presence of irritants in the air - severe sneezing, tearing, an abundance of clear snot and a general normal state with good appetite and no fever. Often accompanied by rashes on the body.
It is important to understand that in many cases, a frequent or prolonged runny nose in an infant develops for several reasons and different symptoms may overlap each other. As a result, the clinical picture turns out to be blurred; only a doctor can reliably determine the causes of the disease.

For diseases of the respiratory tract, the doctor must listen to the lungs in order to detect or exclude bronchitis and pneumonia in time.
Summary
If the child does not have a fever, there is no profuse snot or dry nasal mucosa, and there is only some difficulty breathing in the first 2-3 months of life, these are the physiological characteristics of the baby, namely the immaturity of the respiratory tract.
If a constant dry runny nose occurs in a baby without an increase in temperature, the mucous membrane dries out and crusts appear in the nose - this is a reaction to the dry hot air in the room.
If a child sneezes frequently and has snot, but there is no increase in temperature and remains feeling normal, this is most likely a reaction to irritants in the air.
If the temperature has risen, the snot has become profuse, or has acquired a thick green or yellow color - we are talking about an infectious disease.
If a prolonged runny nose occurs after treatment for an infectious disease and abuse of vasoconstrictor drugs, then most likely it is caused by drug-induced rhinitis.
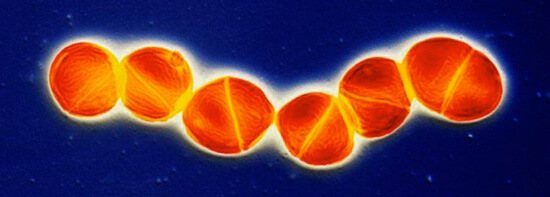
Pneumococcus, which causes rhinitis © Eye of Science / SPL / Barcroft
In any case, if a newborn’s runny nose does not go away, it is worth showing him to the pediatrician. The doctor will determine the cause of the disease and tell the parents what to do. If a child’s temperature constantly rises, and a runny nose is complicated by a cough or severe malaise, consultation with a pediatrician is necessary.
Types and symptoms of rhinitis in infants
The occurrence of a runny nose in newborns tires not only the child, but also the parents. The baby has not yet learned to breathe through the mouth, and a stuffy nose interferes with normal breathing. During this period, the baby is restless, sleeps and eats poorly, and often cries.

Typical symptoms of a runny nose include:
- thick discharge from the nasal cavity;
- possible increase in temperature;
- breast or bottle refusal;
- the appearance of difficulty breathing, shortness of breath;
- in the case of an allergic rhinitis, in addition to discharge from the nasal passages, itching, redness of the nose, and bouts of sneezing may appear;
- the child constantly pulls his hands from his face or nose;
- the baby shows anxiety, his daily routine changes (restless sleep, difficulty falling asleep, refusal to eat).
There are four main types of runny nose:
Physiological is a natural phenomenon in children under 3 months of age. This type of rhinitis does not need to be treated.
Viral or bacterial occurs when a viral or bacterial infection is attached. In this case, snot is the child’s protective reaction to infection.
Allergies occur after a baby comes into contact with allergens.
Vasomotor rarely occurs in children under one year of age. This type of runny nose is a consequence of problems with the vessels of the nasal mucosa.
Physiological runny nose
We discussed this topic in detail in a separate article. Now let’s just remind you what parents need to do so that the baby’s nose breathes normally as soon as possible:
- Ensure normal air humidity in the room - above 50%;
- Give drinks between feedings;
- Walk him outside more often.

A child always needs comfortable living conditions and walks in the fresh air, and even more so when he has a runny nose.
It is if these requirements are met that the baby’s nasal mucosa will be able to adapt to living conditions as quickly as possible and the runny nose will go away.
Types and symptoms of rhinitis in infants
The occurrence of a runny nose in newborns tires not only the child, but also the parents. The baby has not yet learned to breathe through the mouth, and a stuffy nose interferes with normal breathing. During this period, the baby is restless, sleeps and eats poorly, and often cries.
Typical symptoms of a runny nose include:
- thick discharge from the nasal cavity;
- possible increase in temperature;
- breast or bottle refusal;
- the appearance of difficulty breathing, shortness of breath;
- in the case of an allergic rhinitis, in addition to discharge from the nasal passages, itching, redness of the nose, and bouts of sneezing may appear;
- the child constantly pulls his hands from his face or nose;
- the baby shows anxiety, his daily routine changes (restless sleep, difficulty falling asleep, refusal to eat).
There are four main types of runny nose:
Physiological is a natural phenomenon in children under 3 months of age. This type of rhinitis does not need to be treated.
Viral or bacterial occurs when a viral or bacterial infection is attached. In this case, snot is the child’s protective reaction to infection.
Allergies occur after a baby comes into contact with allergens.
Vasomotor rarely occurs in children under one year of age. This type of runny nose is a consequence of problems with the vessels of the nasal mucosa.
Reaction to unsuitable microclimate parameters
It is because of this reaction that a constant runny nose most often develops in an infant. Since the child is in a room with an unsuitable microclimate most of the time, his nasal mucosa almost constantly swells or dries out. While the baby is on walks, she does not have time to return to normal. Nasal congestion and sneezing in infants does not go away until the conditions in the room return to normal.
To solve this problem, parents almost always need to:
- Humidify the air in the room. To do this, you can buy a humidifier, hang wet towels and special hanging cups of water on the radiators. You can even install plastic water bottles with the neck cut off inside heating radiators;

Maintaining air humidity and temperature within the limits recommended by the pediatrician will ensure normal functioning of the child’s nasal mucosa. The photo shows a humidifier. - Keep room temperature at the lower end of the limits recommended by your pediatrician. That is, if the doctor advised maintaining 20-22°C, you need to keep it at 20°C;
- Take your baby outside more often.
If the nasal mucosa of a child is dry, then to maintain it in a normal moist state, you need to instill saline into the nose or use special sprays based on sea water. The amount of saline solution must be strictly controlled, since it is difficult for infants to cough up and problems may arise if liquid gets into the throat. 1-2 drops in each nostril will be enough.
On a note
You can put oil in your baby's nose only in consultation with your pediatrician, only before bedtime, and only when the nasal mucosa is dry. If a child has liquid, even thick, snot in his nose, he should not be given oil.
Useful video: put drops in your baby’s nose correctly!
Reaction to stimuli in the air
Because of this reaction, a frequent runny nose usually occurs in infants. It seems to parents that the child gets sick every few days, which goes away in 2-3 days, but in fact the baby’s nasal mucosa becomes irritated due to the abundance of dust in the apartment, which accumulates between cleanings, or in response to the smell of cleaning products that Mom uses it once a week to clean the bathtub and toilet. Sometimes, when the effect of irritants is constant, swelling of the mucous membrane turns into a persistent runny nose in an infant.
In such cases, parents first need to find out what substances (or set of substances) the child reacts to by sneezing. Most often these substances are:
- Dust on carpets, under beds, on bookshelves, designer uneven ceilings and walls;
- Chlorine-containing cleaning products;
- Cigarette smoke (almost all infants react to it);
- Gasoline, vinegar, kerosene and other strong-smelling technical liquids;
- Animal hair and bird fluff in the air, the remains of chitinous coverings of insects.

Sneezing in children may be a reaction to pet hair.
Regardless of whether the irritant was found or not, in the room where the child spends most of his time (or better yet, in the entire apartment), excess carpets should be removed, and a thorough wet cleaning with special cleaning agents should be carried out at least once every two days, remove cages with birds and pets from balconies or loggias, and prevent cigarette smoke from entering the apartment.
On a note
The baby should not rinse his nose in an attempt to clear it of dust and other irritants. You can only remove excess snot from a child’s nose using an aspirator or bulb.
Infectious rhinitis
Let us repeat once again: a persistent infectious runny nose in an infant without immunity disorders and without complications is rare. The reason for this lies in the very mechanism of interaction of the body with infection. If the immune system is able to fight the disease, then in 5-7 days, sometimes longer, it produces the necessary antibodies and suppresses the infection. Nasal congestion and sneezing go away, and the child gains immunity.
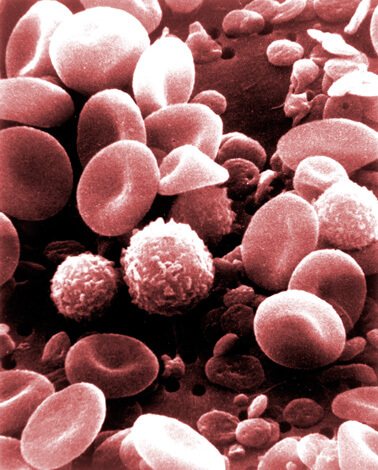
The photo shows blood cells, among which are leukocytes, which are responsible for immunity. If the immune system is normal, then the body can cope with a runny nose on its own.
If the immune system is not able to fight the infectious cause of a runny nose (usually this occurs in children with congenital immunodeficiencies or simply weakened after another illness), then the virus or pathogenic bacteria spread in the body, complications appear (laryngitis, pharyngitis, other respiratory tract diseases, otitis media and conjunctivitis).
The balance in which the infection in the nose will not be suppressed, but will not spread, cannot be maintained in principle. If a baby’s runny nose does not go away for a month, but is not complicated by anything, it is most likely not an infectious disease. This is confirmed by the fact that in infants infectious manifestations, such as high body temperature and purulent snot, rarely last more than two weeks.
On a note
A persistent runny nose is more common in school-age children. In them, it develops as a consequence of untreated rhinitis, the development of sinusitis and rhinorrhea.
In infants, the paranasal sinuses are not yet developed; getting rid of snot along with infectious agents is easier.
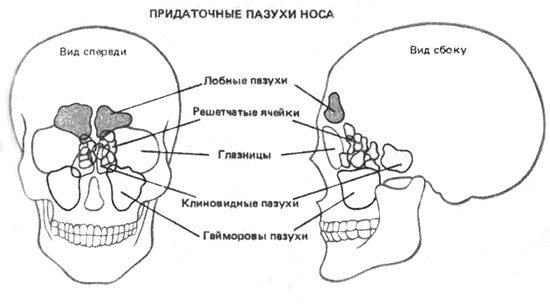
In infants, problems with the paranasal sinuses do not arise due to the absence of the sinuses themselves.
Frequent, sometimes passing, sometimes reappearing, a runny nose in an infant may well be of an infectious nature. This means that the child is easily susceptible to infection, is weakly tempered, and often meets in closed spaces with sick people (for example, his mother constantly drags him to clinics). In this case, parents need to take measures to harden the baby, walk him outside as often and as long as possible, and avoid communicating with sick people. On the advice of a pediatrician, the baby’s diet may be adjusted, and vitamin complexes may be prescribed.
On a note
For an infant, it is better to call a pediatrician at home. This costs more than showing the baby to a doctor in a clinic, but it protects him from encountering a huge number of viruses.
Treatment is usually carried out with the help of immunomodulators and symptomatic therapy (vasoconstrictor drops for severe forms of edema and complete nasal congestion, sputum thinners, antipyretics, antiseptics), and for severe bacterial infections - antibiotics.
Laferobion suppositories are sometimes prescribed to children for ARVI and viral rhinitis.
On a note
Taking immunomodulatory drugs in infants to prevent a runny nose is undesirable. The same interferon preparations - suppositories Laferobion, Viferon, Genferon - can only be prescribed by a doctor and only during the acute phase of an infectious disease. A large number of side effects make them undesirable drugs for the prevention of acute respiratory viral infections and bacterial infections.
General recommendations for the treatment of rhinitis in an infant
Treatment of a runny nose in an infant should begin with cleansing the nasal passages using special devices - aspirators, which are sold in pharmacies. For minor discharge, the nose is cleaned using flagella, making light rotational movements.
If the baby's body temperature is higher than normal, call a pediatrician immediately. Walking and swimming should be postponed. After normalization of body temperature, in the first days after illness, walks are taken only in good weather, and water procedures are started only on the 4th day of normalization of the baby’s condition.

Do not force your baby when he refuses to eat. If you have a runny nose, this refusal is justified. The body fights intoxication and removes all pathogenic microorganisms it does not need. Don't worry about this. With proper treatment and following all the pediatrician’s recommendations, the baby’s appetite will return to normal in a few days.
With a prolonged runny nose, it is necessary to direct all efforts to clear the nasal passages of mucus and normalize nasal breathing.
Infants who have already been introduced to complementary foods can increase the amount of fluid they drink through compotes, teas and juices. This will remove the virus faster and saturate the body with vitamins.
An integral part of the treatment of all forms of rhinitis in infants is ventilation and wet cleaning. The air in the baby's room should not be dry and stuffy, and its temperature should be maintained within 20 degrees.
In the good old days, wet diapers hung on radiators were used to humidify the air in the children's room. Now this issue can be solved more simply - purchase a modern air humidifier in the household appliances department.
How to treat rhinitis correctly
Drug-induced rhinitis and the consequences of improper treatment
Drug-induced rhinitis develops when vasoconstrictor drops - Vibrocil, Sanorin, Nazol and others - are instilled into the baby's nose for a long time. They contribute to drying of the nasal mucosa with disruption of its functioning, and after 5-6 days of use they lead to addiction. As a result, if you stop taking them, the baby’s nose becomes completely blocked, and instillation provides relief for only a few minutes.

Failure to comply with the dosage and timing of use of vasoconstrictor drops can lead to the development of drug-induced rhinitis and other complications.
Drug-induced rhinitis is a case when a baby’s runny nose does not go away for a very long time due to the use of vasoconstrictor drops.
The best thing to do in this situation is to stop taking vasoconstrictors. The child will breathe through his mouth for several days, and then his condition will return to normal. It is only important that during the period of discontinuation of the drops the baby’s throat is not sore.
Significantly worse advanced long-term runny nose. It can develop either due to completely ineffective treatment or due to the use of drugs that are dangerous to the child.
For example, if bacterial rhinitis in a weakened child is “treated” with homeopathic remedies and spells, an infection in the nose develops without proper counteraction and can lead to severe inflammation of the nasopharyngeal mucosa, involving the auditory tubes and throat. Even if the infection in the nose is suppressed, it can persist in the same Eustachian tubes during otitis and cause relapses of the runny nose.
Another situation is the use of pseudo-medicinal folk remedies, which only worsen the infection. For example, putting breast milk or honey in the baby’s nose. If, without such mistakes by parents, the child’s body itself would have overcome sneezing and nasal congestion in normal times, then on sugars from honey or milk, bacteria actively grow and multiply, the infection develops more actively and the body cannot cope with it.

Using honey, milk or other liquid containing sugar as nasal drops leads to the proliferation of pathogenic microflora and exacerbation of the disease.
It’s even worse when onion or garlic juices, celandine extracts, and various oils are dripped into the baby’s nose for a runny nose. The same onion juice burns the mucous membrane and leads to the development of ulcers, which greatly complicates rhinitis. And, for example, oils in the presence of snot in the nose block the work of the epithelium of the mucous membrane, inhibit the removal of snot with bacteria and their remains from the nose and lead to complete blockage of the nose with snot and further advancement of the infection deeper into the nasopharynx.
If a prolonged runny nose develops in an infant precisely after treatment with folk remedies, then treatment should be stopped immediately and the child should be shown to a doctor. Depending on the severity of the disease, he will choose the means and treatment tactics. If chronic nasal congestion and sneezing developed after “civilized” treatment prescribed by a doctor, then it makes sense to show the baby to another pediatrician and describe in detail all previous treatment. In such situations, it may be necessary to use a variety of means, including antibiotics and balms that promote mucosal regeneration.
In any case, if a child requires treatment, only a doctor should prescribe it. You can’t try different remedies on your own on your baby, trying to guess the diagnosis and hit the nail on the head. Moreover, if a baby’s runny nose does not go away for more than 2 weeks, this means that the body cannot eliminate the cause, and the measures taken by the parents either do not produce results or contribute to the progression of the disease. If the symptoms do not go away after the treatment prescribed by the doctor, then it makes sense to additionally consult with another specialist.
Remember that frequent infectious rhinitis can always be complicated by bronchitis, otitis media and pneumonia, and it is the doctor who will be able to listen to the child and diagnose these diseases at those stages when they are most treatable. So take care of your baby, don’t worry in vain, but if necessary, immediately contact specialists.
Such a different runny nose in a newborn! How to treat?
A runny nose is an unpleasant illness. Outwardly one of the most harmless. But untreated can lead to serious consequences. After all, the sinuses communicate with the respiratory organs, vision, and even the brain. And the sensations themselves are not very good. What to say if a baby has a runny nose. He can’t blow his nose, and he can’t complain or describe symptoms yet.
Free nasal breathing is very important for a newborn. When a baby sucks on a breast or bottle, he breathes through his nose. When he sleeps, too. When children have a runny nose, their appetite is spoiled and sleep is disturbed. That is, it becomes difficult to create conditions for normal growth and development. Therefore, mothers strive to quickly learn how to treat a runny nose in a baby.











