Jaundice (also known as hyperbilirubinemia) is the cause of the yellow discoloration that appears on the skin and eyeballs of newborn babies in the first week or two. Jaundice occurs because babies are born with more red blood cells than they need. When the liver breaks down these extra cells, a yellow pigment called bilirubin appears. Since the immature liver of a newborn cannot quickly dispose of bilirubin, excess yellow pigment is located in the eyeballs and skin of the newborn. This type of jaundice is called physiological jaundice because it is part of a normal process in the body. As the newborn's bilirubin elimination system matures and the number of excess red cells decreases, the jaundice will subside (usually within a week or two) and will not harm the baby. Jaundice is more common in prematurely born babies, who are less able to cope with excess bilirubin.
In some cases, with certain blood types or Rh incompatibility, jaundice may result from problems that go beyond simply having too many red blood cells. Very rarely, bilirubin levels can rise so high that they affect the baby's brain. For this reason, if the healthcare provider suspects that the cause of the baby's yellow skin is something more than normal physiological jaundice, then bilirubin levels should be monitored more closely using special blood samples. If bilirubin levels become too high, your doctor may try to lower them using phototherapy, which breaks down extra bilirubin in the skin, helping it to be eliminated from the body in urine.
In a biochemical quirk not yet fully understood, jaundice tends to be worse in breastfed infants, with bilirubin levels 2 to 3 milligrams higher than in formula-fed infants. The differences, it seems, are associated with an as yet unidentified factor of the influence of mother's milk, which stimulates increased absorption of bilirubin by the intestines, as a result of which it returns to the blood circulation better than it is excreted by the liver. Higher rates of jaundice in breastfed infants may also be associated with decreased milk intake in the first days after birth due to infrequent or ineffective feedings. It is normal for breastfed babies to have jaundice for a little longer, sometimes until the third week after birth. This difference in bilirubin levels between breastfed and formula-fed infants is small, but jaundice phobia may lead some parents and physicians to avoid breastfeeding. Watch out for what we call yellow flags that signal an overreaction to jaundice in a breastfed baby. Dismiss any suggestion that your milk is somehow not good for your baby, or that your baby should receive supplemental water or formula when bilirubin levels are relatively low (less than 20 milligrams). Instead, try the following techniques to reduce your baby's bilirubin levels and your anxiety levels:
– To start, follow the suggestions, i.e. early, frequent, unrestricted breastfeeding with an effective latch technique. The more breast milk a baby receives, the faster bilirubin will be removed from his intestines. Bilirubin is excreted in the baby's stool and therefore breast milk has a laxative effect and those babies who eat frequently tend to soil their diapers frequently and therefore will have lower bilirubin levels.
– Don’t worry, produce milk. If your baby has jaundice, make sure you understand what type of jaundice your baby has. If this is normal physiological jaundice, then you have absolutely nothing to worry about. If this jaundice is due to medical reasons, such as blood type incompatibility, make sure you understand that it is easily treated and will not affect breastfeeding. Anxiety can cause your milk supply to decrease and compromise your ability to breastfeed your baby. This interferes with breastfeeding success.
– Remember that jaundice sometimes makes the baby drowsy, so he eats less enthusiastically. The higher the bilirubin level, the sleepier the baby. Babies need to be fed to get rid of bilirubin, but they tend not to wake up often enough or eat long enough and may need help.
– If phototherapy is necessary due to high bilirubin levels, make sure your doctor is on your side so that treatment for jaundice does not affect breastfeeding. It is not at all necessary to tear the child away from the mother and place him in a hospital room under the light of phototherapy. Most children do well with photooptic bilirubin blankets (phototherapy light that wraps the baby). You can hold and feed your baby at home while the light breaks down the bilirubin.
– Offering bottles of sweet water to the child in the hope of lowering bilirubin levels has shown to be ineffective. Research suggests they may even worsen jaundice because babies whose stomachs are full of glucose solutions may eat less frequently, reducing their milk intake and ability to excrete bilirubin in their stool. The water doesn't push the chair forward; and food (milk) – yes.
– If your doctor advises giving your baby a supplement to provide more calories and reduce intestinal absorption of bilirubin, ask about using your milk instead of formula if your baby is still too sleepy to eat effectively. Work with a lactation consultant to provide these supplements through baby supplement systems, syringes, or finger feeding.
In some breastfed infants, bilirubin levels may exceed 20 milligrams, and jaundice may last until the third week of life or longer. It was previously thought to be caused by another type of jaundice called breast milk jaundice, which was found in a small number of mothers whose milk contained a substance that can interfere with the absorption of bilirubin. Treatment for this type of jaundice involves weaning for twenty-four to forty-eight hours. At the same time, the level of bilirubin decreases, but the course of breastfeeding is sabotaged. More recent studies have shown that high bilirubin levels or persistent jaundice, but otherwise healthy breastfeeding, are just a normal variation of run-of-the-mill physiological neonatal jaundice.
There may also be a substance in mother's milk that prevents the intestines from absorbing bilirubin, but whether the baby will have mild or severe jaundice depends largely on individual differences between mothers and babies. However, some doctors may suggest temporary weaning (twenty-four to forty-eight hours) to lower bilirubin levels. Discuss with your doctor whether there are other alternatives, such as phototherapy, that will allow you to breastfeed without restriction. If you decide to try bottle feeding for a day or two, be sure to express milk every two or three hours so that you can continue to produce milk and avoid breast infections. Artificial supplements can be given through finger feeding or cup feeding to avoid nipple problems when baby returns to the breast.
The concept of bilirubin
Bilirubin is a bile pigment that is formed during the breakdown of proteins containing heme, in particular hemoglobin, in the body. The latter is found in the blood in red blood cells. After birth, some of the hemoglobin in the blood breaks down and bile pigment is formed. Almost all newborns have increased bilirubin.
The newborn's liver removes the end products of hemoglobin processing. If pigment levels are very high, the baby’s internal organs cannot cope with the load and medical attention is required.
The child turns yellow as the bile pigment increases. First, the color of the face, neck, and then the whole body changes. This does not bother the baby in any way if the indicators are elevated within the age norm. If bilirubin is above 300 in a newborn, there is a risk of brain intoxication and severe consequences for the child.
Bilirubin in the blood can be total, direct or indirect. The total is the sum of the last two indicators. Direct bile pigment is excreted from the body on its own, it is not dangerous and easily dissolves in water.
Medical personnel pay the greatest attention to indirect bilirubin in a newborn. Its volume in the blood is 2/3, it dissolves only in fats and requires measures to reduce it. In any case, within a month the indicators should return to normal, and if this does not happen, then we are talking about pathological jaundice.
Why is elevated bilirubin dangerous in newborns?
An increase in bilirubin levels in a newborn for more than 1 month of life is extremely dangerous for the baby’s life.
If the pigment level significantly exceeds its norm, at the time when it should return to normal, bilirubin passes through the blood-brain barrier.
This phenomenon is extremely dangerous for the functioning of the child’s nervous system. If you do not diagnose the disease that has led to such consequences in time and do not begin to treat it, thereby lowering the level of pigment, then this subsequently threatens the child with dementia, as well as paralysis or hearing loss.
Normal for a newborn
After the birth of a child, the level of bile pigment increases. It reaches its highest value on the third day and subsequently decreases. The best option is to increase the total pigment within 50 µmol/l. A value of 250 µmol/l on day 3 is acceptable, but requires treatment. In premature babies, the increase reaches 170 µmol/l. Bilirubin in a newborn 300 is considered critical and requires urgent hospitalization of the child.

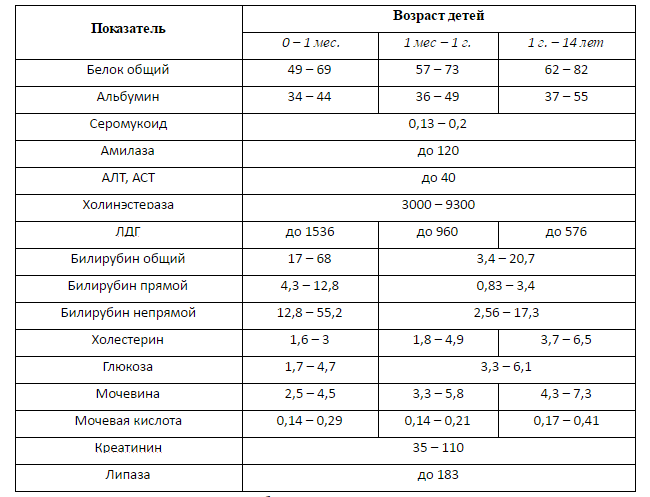
The norms of bilirubin in the blood, depending on age, are as follows:
- 1 day - less than 32 µmol/l;
- 2 days - up to 150 µmol/l;
- 3-5 days - no more than 200 µmol/l;
- 6 days and older - up to 21 µmol/l.
Normally, indirect bile pigment should not exceed the values presented in the table.
| Child's age | |||
| 1 day | 23,1 | 8,7 | 14,4 |
| 54,2 | 8,7 | 45,5 | |
| 4 days | 90,1 | 7,9 | 82,3 |
| 6 days | 72 | 8,7 | 63,3 |
| Day 9 | 53 | 8,7 | 44,3 |
| 1 month | 3,4-13,7 | 0,85 | 2,56-10,3 |
What is the normal level of bilirubin in a newborn?
Bilirubin in the blood is presented in two fractions:
- Indirect (free), which is formed as a result of the fact that the rate of breakdown of red blood cells is higher than the ability of the liver to bind bilirubin. Free bilirubin is a substance that tends to dissolve only in lipids (fats). Due to its inability to dissolve in water, the pigment is very toxic, accumulates in the bloodstream, causing characteristic staining, and can disrupt the normal functioning of cells, easily penetrating into them.
- Direct (bound) bilirubin is formed directly in the liver. After biochemical interaction with the organic acid of the uronic acid group and liver enzymes, which reduce the toxicity of the pigment, it becomes soluble in water and is easily excreted from the body along with bile and urine.
The indicators of the two fractions add up to the total concentration of bilirubin in the blood, with direct bilirubin accounting for no more than 25% of the total volume.
In order for free bilirubin to become bound and soluble, it must be transported to the liver by certain proteins that newborns lack. As a result, the level of bilirubin in the blood increases, and physiological jaundice occurs.
The table shows the norms of bilirubin levels in infants (table of bilirubin in newborns by day)

Jaundice develops in newborns if bilirubin levels are above 50 µmol/l and is expressed, in addition to the concentration of pigment in the blood, by changes in the condition of the infant’s skin: initial color, capillary tone, the extent of the pigment distribution area.
To assess the intensity of changes in indicators, the Cramer scale is used, which can be used to assess the severity of the child’s condition:
- The head area turns yellow (eye sclera, face, palate, tongue below) - 100 µmol/l.
- Yellowness descends to the upper area of the body above the navel - 150 µmol/l.
- The area below the navel is added, including the buttocks and thighs - 200 µmol/l.
- The upper and lower extremities are painted with pigment - 250 µmol/l.
- Skin changes color throughout the body, including fingers, toes, palms and feet - over 250 µmol/l.

The higher the indicator, the more serious the reason to assume that the child has jaundice of various types and degrees of severity and such complications as gallbladder dyskinesia.
For full-term infants, the critical indicator will be the concentration of bilirubin in the bloodstream above normal and up to a limit of 250 µmol/l, for those born prematurely - 200. Infants born prematurely have a greater risk of being in the group diagnosed with “jaundice” due to underdevelopment of body systems and increased sensitivity to adverse conditions.
Indirect bilirubin toxins can cause damage to the deep structures of the anterior part of the brain, which are responsible for motor activity and coordination, and cause bilirubin encephalopathy (kernicterus). This condition provokes:
- increased drowsiness or extreme agitation;
- decreased sucking reflex;
- increased muscle tone in the back of the head.
Important! Parents should know that excessive readings negatively affect the functioning of the brain and biliary organs. If the skin of a newborn suddenly turns yellow-brown, you should seek medical help without delay. Only a decrease in bilirubin levels will help avoid toxic poisoning with bile pigment.
In the absence of pathology, within 2-3 weeks from the moment of birth, the level of direct bilirubin gradually decreases and returns to normal; it is during this period that the physiological jaundice of the baby disappears completely and does not return.
Why does bilirubin increase?
A condition in children and adults in which there is an increase in the amount of bilirubin is called hyperbilirubinemia. The breakdown of hemoglobin in the blood occurs with the appearance of bile pigment, direct and indirect. The latter must be removed from the body so that it does not accumulate in the tissues. There is a protein in the blood called albumin, which captures toxic substances and delivers them to the liver for further disposal. After processing by the liver and glucoronic acid, indirect bilirubin becomes direct and is easily excreted in bile and urine.
Liver enzymes work differently in a newborn than in an adult. It takes time for ripening to occur and for the body to cope with bilirubin itself. But until this happens, the indicators are rising, the jaundice is increasing. The higher the toxic levels, the yellower the child will be. Sometimes the palms and soles become yellow.
If a newborn has a bilirubin level of 300 on the 5th day, then medical attention is required to exclude brain intoxication. The yellowing of the child after the maternity hospital or increased jaundice should alert the mother and become a reason to contact a pediatrician. Unusual behavior of the newborn, drowsiness and lethargy require urgent hospitalization.

What is bilirubin and what is its normal level?
In the body of every person there is a special yellow-brown pigment - a product of the breakdown of blood cells (erythrocytes). Every adult has seen how bilirubin appears when bruises on the body heal: the color of the bruised area changes from blue to yellow. This occurs as a result of the destruction of protein elements in the blood - then the amount of bilirubin increases. But over time, the level of bilirubin returns to normal - the pigment is excreted from the body along with natural human waste.
In a newly born baby, bilirubin is always higher than normal. Here's what explains it. In the mother's tummy, the baby cannot breathe on its own; oxygen is delivered by the mother's blood cells, saturated with hemoglobin. When a child is born, the parental hemoglobin preserved in his body is destroyed as unnecessary. As a result of this process, the first bilirubin in a little person’s life is formed.
Babies who were born prematurely often have physiological jaundice for the reason that the mechanisms for its removal from the body are not yet so perfect, and bile pigment is excreted much more slowly.
What tests indicate jaundice?
After the baby is born on the 1st day in the maternity hospital, blood will be taken from a vein for analysis. One of the indicators will be bile pigment. The laboratory technician will evaluate the level of direct and indirect bilirubin.
One way to determine the level of bile pigment is blood from the umbilical cord. After 2 days, the analysis is repeated to assess how much the indicator has increased. If the indicator is within the normal range, then most likely it will not increase critically, but will decrease in the future. If a newborn’s bilirubin level is 300, then an experienced doctor will determine by the child’s appearance that the bile pigment is increased and will send it for tests.
In many maternity hospitals, a digital bilirubinometer is used to determine the level of total bilirubin. The measurement is taken in the area of the forehead or chest; the procedure is absolutely painless for the child and takes a few seconds.
Causes of jaundice
Physiological jaundice in newborns increases the considered indicator within normal limits and goes away on its own within 2-4 weeks. Pathology is indicated if it persists for a long period of time or if bilirubin in newborns is increased to 300. The reasons may be different:
- a conflict of Rh factors was detected in the mother and child;
- consequences of genetic diseases;
- the woman took medications during pregnancy that affected the fetus;
- albumin protein deficiency;
- congenital or acquired hepatitis;
- liver or gallbladder diseases;
- intestinal obstruction.
Of course, bilirubin 300 in a newborn is a lot. If a baby has a bile pigment level of 200, then the reasons may be the following:
- prematurity of the child;
- difficult childbirth;
- difficult pregnancy with threat of miscarriage;
- hypoxia of the child during pregnancy or childbirth;
- maternal diabetes;
- injury to the child during childbirth.
Untimely treatment of extremely high bilirubin can cause the development of encephalopathy and mental disorders in the child.

Causes of high bilirubin in newborns
It is impossible to diagnose increased bilirubin immediately after birth. Its level rises sharply 3-4 days after birth.
Here are the main reasons for increased bilirubin in infants:
- Mismatch of blood groups or Rhesus of mother and newborn.
- Premature birth.
- Hemorrhages in the child’s body (even minor ones).
- Problems with the outflow of bile.
- Digestive disorders.
- Infections.
- Genetic predisposition.
- Pathologies of the endocrine system.
- Consequences of exposure to drugs that stimulate labor.
- Liver diseases.
For each baby, the reasons for increased bilirubin are individual. Only a specialist can determine the exact cause. If you know that you also had elevated bilirubin at birth, be sure to inform the doctor who is caring for your pregnancy about this.
Consequences of increased bilirubin
The lower threshold for an extreme value is considered to be bilirubin 300 in a newborn. The consequences of such an increase can be fatal. Measures to reduce it must be taken immediately.
Fat-soluble bilirubin takes a long time to be eliminated on its own. With small indicators there is nothing terrible about this. But at high levels, bilirubin is deposited in the cerebral cortex and leads to kernicterus. Intoxication of the entire body occurs and there is a risk of developmental abnormalities. In severe cases, death is possible.
Symptoms of kernicterus:
- long continuous crying;
- yellowness of the skin and sclera;
- drowsiness, lethargy;
- the baby sucks poorly;
- the child tenses and stretches his neck muscles.
Signs indicating that a child has physiological jaundice:
- the child is active;
- sucks well;
- the pigment appears from day 2 and intensifies on days 3-4;
- the yellowness gradually subsides and disappears within a month;
- no changes in stool or urine.
The degree of yellowness can be determined by the skin:
- face and neck painted;
- yellowness is visible up to the navel;
- the color of the upper limbs changes;
- the skin is all yellow.
When bilirubin is 300 in a newborn, how long this indicator will decrease depends on the child’s body and the therapy performed. It may take several days, in some cases 3-6 weeks.
Medical assistance for elevated bilirubin
How to reduce bilirubin in a newborn? If physiological jaundice is diagnosed, no special measures are needed other than observation. Usually the disease subsides after a few weeks.
Sunbathing will help reduce bilirubin in a newborn faster. If you have a “spring” or “summer” child, then during walks you can move the hood of the stroller, exposing the baby’s face and arms to the sun. Winter and autumn sun are more difficult to catch. But if it’s a clear day, go out onto the balcony with the baby and let the rays shine on the baby’s face.
The baby should not be in the sun for more than 10 minutes. In this case, it is necessary to ensure that the sun does not fall into the open eyes. In late spring and summer, keep your child out of direct sunlight from 11 a.m. to 5 p.m.
Phototherapy is the most effective way to treat pathological jaundice. It can be carried out in a maternity hospital if it has the necessary equipment. Otherwise, mother and baby are transferred to a children's hospital. The baby is placed under a special blue lamp.
With the help of light, bilirubin is converted into lumirubin, which quickly leaves the body. You need to lie under the lamp for a total of 96 hours, with breaks for feeding.
Children are put on a special bandage or a cap over their eyes, since the light from the lamps is harmful to their eyesight. The procedure is painless and effective, but it can also have unpleasant side effects: drying and flaking of the skin, loose stools, which will go away after completion of the therapy.
In especially severe cases, children are given IVs and even blood transfusions. An excellent prevention of jaundice is feeding with mother's milk. It is very important to get your baby to the breast as quickly as possible. Read how to do this in the article: Breastfeeding: WHO recommendations.
Feeding on demand also helps reduce the amount of harmful pigment. Colostrum provokes the excretion of meconium from the newborn’s body, along with which a large amount of bilirubin is released. Learn more about on-demand feeding>>>
One of the bad pieces of advice that a mother may hear is to give a baby with jaundice more to drink. Neither sweet water nor rosehip decoction will reduce bilirubin levels. It’s better to put your baby to your breast more often and follow your doctor’s recommendations.
Bilirubin content is an important indicator of the health of the newborn. In no case should you refuse to determine it and treat jaundice. The consequences of such a refusal can be much worse than some inconveniences during therapy.
One of the important indicators of a child’s health immediately after birth is the level of bilirubin in the blood, which is not stable in the first days of life and causes anxiety in young mothers, turning the baby’s body a jaundiced color. What should be the level of bilirubin in newborns, how to distinguish normal from pathology, and also choose the right treatment tactics? Only a pediatrician can answer these questions in detail after closely monitoring the baby’s condition, but in our article you will read basic information on this topic.

Phototherapy
Phototherapy for bilirubin in a newborn 300 gives good results. The method is based on the use of safe ultraviolet radiation with a wavelength of 400-550 nm. Under the influence of a lamp, indirect pigment can be eliminated from the body.
The child is placed under a lamp and the boy’s eyes and genitals are covered with special glasses. The child is only taken out to eat. With severe jaundice, the child is kept under a lamp around the clock; it is possible to place the lamp above the mother’s bed and carry out treatment even during feeding. Periodically, the child should be turned onto his back and stomach so that bilirubin breaks down on all sides.
Breastfeeding has a positive effect on the removal of toxic substances from the body. It should be noted that with phototherapy, the baby's need for fluid increases by 10-20% and the number of breastfeeding may increase. Treatment is completed when the total level of bilirubin in the blood decreases.
Is bilirubin 300 dangerous in a newborn? Reviews from mothers say that it is dangerous, but only in the absence of treatment. When phototherapy is started on time, the prognosis is favorable.
How to lower bilirubin in the blood with folk remedies: treatment at home
Approximately 60% of full-term newborns and 80% of infants develop jaundice. In this case, the skin, mucous membranes and sclera of the child’s eyes acquire a yellow tint. Parents have a question about how to quickly reduce bilirubin in the blood.
Bilirubin is a component of bile that arises as a result of the breakdown of hemoglobin, myoglobin, and cytochrome. This substance often increases in newborns.
There are physiological and pathological jaundice. A couple of days after birth, children's skin and eyeballs turn yellow. The state of health does not deteriorate. These are signs of physiological jaundice.
This condition does not require treatment. It occurs due to the breakdown of fetal hemoglobin. The body is gradually cleansed of toxic compounds. Excessive amounts of bilirubin are excreted in feces and urine. This process is quite long. As a rule, the skin and sclera of the eyes acquire a healthy color after 4-5 days.
But it happens that cleaning takes about 2-3 weeks. This means that the body cannot cope with the load. Pathological jaundice is caused by disturbances in the functioning of the liver and gallbladder. It is accompanied by poor health: nausea, lack of appetite, pain in the right hypochondrium, drowsiness. This kind of jaundice needs to be treated.
Pathological jaundice negatively affects the functioning of the brain, nervous system, and digestive tract.
Parents whose children have been diagnosed with pathological jaundice are faced with the question of how to quickly reduce bilirubin in the blood of a newborn.
In the warm season, it is recommended to provide the child with sunbathing daily; ultraviolet light promotes the effective breakdown of bilirubin.
To speed up the process of removing this substance from the body, various medications are used. They must be used as prescribed by a pediatrician.
If the child’s condition is not serious, then treatment can be carried out at home. Some parents resort to using folk remedies. Non-traditional methods of therapy have a lighter and gentler effect on the body and usually do not provoke the appearance of adverse reactions. There are also hardware methods for reducing high bilirubin levels.
Before prescribing treatment, the doctor conducts an examination. If the cause of high bilirubin is a decrease in liver function, then hepatoprotective, choleretic drugs, vitamins and sorbents are prescribed.
If jaundice is caused by an infectious-inflammatory process, then antiviral and antibacterial medications are used. Regardless of which remedy is chosen, it should be taken strictly according to the instructions and recommendations of the pediatrician.
Newborns are allowed to be given the following medications to support the liver, gallbladder and digestive function:
- Karsil. Contains milk thistle extract. Restores liver cells;
- Hofitol. The main active ingredient of the drug is artichoke extract. For young children, an oral solution is used;
- Ursofalk. Contains ursodeoxycholic acid. Activates the liver, reduces the load on the brain, and has an immunomodulatory effect. It is given to newborns in the form of a suspension;
- Ursosan. The main component is ursodeoxycholic acid. It has a beneficial effect on the liver, helps convert free bilirubin into direct bilirubin.
To cleanse the body of harmful substances, infants should be given the following sorbents:
- Enterosgel;
- Activated carbon.
For pathological jaundice, the doctor may recommend Hepel to the baby. This is a homeopathic remedy. It contains only natural ingredients that are safe for newborns. The drug absorbs toxins and improves liver function.
Drug Hepel
In severe cases, glucose solution is administered intravenously. It reacts with bilirubin and breaks it down, thereby reducing the concentration in the blood. The child may also be given other medications to cleanse the blood by infusion.
Folk remedies
The advantage of using folk remedies is their safety and accessibility. As a rule, decoctions of medicinal herbs are used to normalize bilirubin levels. These include corn silk, motherwort, St. John's wort, birch leaves, and chamomile.
Effective recipes for the treatment of jaundice in newborns and infants:
- Mix equal parts of corn silk, motherwort, birch leaves and chamomile. Brew two tablespoons with a glass of boiling water. Insist and give to the baby before meals twice a day;
- pour a couple of tablespoons of calendula into 400 ml of boiling water and simmer for half an hour. Add to baby's bath. Immerse the baby in the broth for 10-15 minutes. Then rinse his body with clean water.
Medicinal plants have a beneficial effect on the liver, bile ducts, and digestive function, thereby stimulating the cleansing of the body.
One of the effective methods for treating jaundice is phototherapy. Its essence is that the baby is placed under an ultraviolet lamp.
The radiation from this device penetrates the skin into the blood and destroys harmful bilirubin.
Remains of the substance are excreted along with feces and urine. Irradiation is carried out under the strict supervision of medical staff.
Ultraviolet lamps can cause dehydration and dry skin.
Therefore, when undergoing phototherapy, it is necessary to give the child more fluids. This can be plain water, rose hip decoction, or breast milk. A nursing mother is advised to avoid eating fatty, salty and fried foods.
Video on the topic

If the level of pigment in the blood is elevated (for a long time), parents need to immediately take the baby to a specialist who can make an appropriate diagnosis and, as a result, prescribe treatment.
Several methods are used to remove bilirubin from the baby’s body:
- Phototherapy. This method involves exposing the baby to ultraviolet rays. To do this, the child is placed in a crib over which the device is located. When ultraviolet light hits a child’s skin, it helps remove pigment from the body, but during this procedure, parents should be aware that such rays can harm the baby’s vision, so his eyes should be covered with a special bandage.
- Infusion therapy. As a result of exposure of the child’s skin to ultraviolet radiation, a large amount of fluid is removed from his body, as a result of which infusion therapy is prescribed, which helps restore the water balance in the baby’s body. To do this, glucose, soda, and drugs that improve microcirculation are introduced into the child’s body.
- Enterosorbents. In this case, Smecta or Entorosgel is prescribed. This is necessary to prevent the reverse absorption of bilirubin into the baby’s blood through the intestines.
- In especially severe cases, the baby is indicated for a blood transfusion.
The selection of methods for removing pigment from the body is carried out exclusively by a doctor.
When breastfeeding, it is recommended that mothers put the baby to the breast more often, as this also helps to quickly remove pigment from the body.
Drug treatment
Drug treatment is prescribed for prolonged jaundice and for identified pathologies in the gastrointestinal tract.
If the disease is caused by intestinal obstruction, then surgical intervention is required. When bile stagnates, choleretic drugs approved for newborns are used. They can use “Hofitol”, “Ursofalk”, “Ursodez” and others. These medications improve the baby's metabolism and improve appetite.
Additionally, sorbents are used to help bind and remove bilirubin from the intestines. You can use activated carbon, Enterosgel or Polysorb. Additionally, the doctor in the hospital prescribes an enema so that harmful substances do not remain in the body.

Folk remedies and medications that the pediatrician has not prescribed are contraindicated for infants. Choleretic herbal preparations, castor oil and laxatives should not be given.
Infusion therapy
With the infusion method of treatment, medications are administered intravenously into the child's body. Therapy is carried out only in a hospital under the supervision of doctors. It is prescribed if it is impossible to fully feed the child during phototherapy, with weight loss, with vomiting, constant regurgitation or other conditions in which the child loses fluid.
When women see IVs, the question arises: “Is bilirubin 300 dangerous in a newborn?” It is dangerous if the pathology is not treated in a timely manner. And if the doctor decides to prescribe intravenous infusions, then they must be completed.
To reduce intoxication and accelerate the elimination of indirect bilirubin, a solution of glucose and sodium chloride is added to the dropper. In some cases, the protein albumin can be administered.
How long does it take for bilirubin to decrease?
No one can say for sure how long it will take for bilirubin to drop to 300 in a newborn. Usually within a week the indicator becomes harmless and gradually decreases to normal levels. But the exact period will depend on the reason for the increase in pigment. If the bilirubin level reaches more than 400 µmol/l, then the therapy will be long-term. With obstructive jaundice, the level may not decrease until the cause is eliminated.

Prevention of jaundice
Prevention should begin in preparation for pregnancy. But even while carrying a child, it is not always possible to stay safe and prevent an increase in bilirubin. If you follow these rules, your chance of reducing the manifestations of jaundice increases:
- identification of Rh factor conflict in mother and child;
- donate blood in a timely manner to determine genetic enzyme deficiency;
- avoid alcohol, tobacco, drugs and chemicals;
- escape from stressful situations;
- reduce the use of medications during pregnancy and childbirth;
- start breastfeeding in the delivery room;
- feed the baby on demand, establish lactation;
- If possible, take the child out into the sun, taking precautions against heat and sunstroke.
Prevention of jaundice is not always able to reduce the manifestations of the disease. In case of yellowing of the child’s skin, it is necessary to show it to the pediatrician.

Many mothers in the maternity hospital hear the phrase “your baby has increased bilirubin.”
In order not to be afraid of these words, it is necessary to understand what role bilirubin plays in newborns and what amount of this substance is safe for the baby.
What can a mother do to reduce the amount of bilirubin in the baby’s blood?
If the baby is breastfed, then the mother should relieve the liver as much as possible by following certain nutritional rules:
- exclude everything fried, salty, smoked, sweet;
- give up carbonated drinks, alcohol, strong tea and coffee;
- steam, boil or bake in the oven;
- give preference to fresh vegetables and fruits;
- Any diets are prohibited;
- you need to eat fractionally, in small portions;
- drink at least two liters of pure still water per day.
What is bilirubin?
Bilirubin is a pigment, a high concentration of which in the body can become poisonous to the nervous system. This substance is the result of the breakdown of red blood cells.
Hemoglobin is released from obsolete red blood cells, which immediately becomes toxic. The immune system begins to “attack the enemy” and destroys hemoglobin, releasing hemes - compounds containing iron. Under the influence of enzymes, hemes are transformed into bilirubin.
It is necessary to distinguish between direct and indirect bilirubin. Direct bilirubin is excreted in feces and urine, while indirect bilirubin first forms a compound with albumin and is transported to the liver, where it ferments and becomes direct bilirubin, which easily leaves the body.
Bilirubin in the blood of a newborn is always elevated. The fact is that oxygen in the body of an unborn child is carried by red blood cells saturated with fetal hemoglobin. After childbirth, it loses its functions and is destroyed, leaving behind a breakdown product - bilirubin.
In the maternity hospital, the child's blood is taken several times to determine the level of this pigment. Increased bilirubin in newborns indicates the occurrence of jaundice, and thus doctors monitor its progress.
Jaundice with high bilirubin is dangerous both in itself and may indicate the development of some pathological condition in the baby.
What is bilirubin, classification
Bilirubin is a pigment, the high content of which can have a toxic effect on the baby’s nervous system.
This pigment is formed during the breakdown of red blood cells in the blood. In the process of their vital activity, red blood cells die, as a result of this, hemoglobin is released, as a result of which it becomes toxic to the child’s body. The immune system, in turn, begins to attack it, releasing hemes that contain iron. Subsequently, hemes are transformed into bilirubin.
Classification
Direct bilirubin is excreted from the baby's body through feces and urine.
Indirect bilirubin first combines with albumin and is transported to the liver, where it is then transformed into direct bilirubin.
An increase in bilirubin in the baby’s body in the first few days of life is a completely natural reaction. Therefore, in the maternity hospital, doctors often take a blood test to determine its level. If the pigment is significantly exceeded, then the baby has jaundice.
In the first days of life, the level of bilirubin in the blood should be 60 µmol/l, after a few days the pigment level rises to 205 µmol/l. and these are completely normal indicators and they shouldn’t scare mom at all.
If a child is born prematurely, the level of bilirubin in the blood is 170 µmol/l, but no more. When the baby turns 1 month old, the pigment level drops to 8.5-20.5 µmol/l.
If, after 1 month of life, the level does not drop and remains persistently at high levels, then this may indicate the presence of various types of pathological changes in the baby’s body, and in this case, the child should be hospitalized and undergo additional laboratory tests that help identify and diagnose the disease.
What tests need to be taken?
- Immediately after the baby's first cry, doctors measure the level of pigment in the umbilical cord blood. Two days later, the full-term baby is tested again.
- For premature babies, the amount of pigment in the blood is checked a day after birth, and it is monitored every 24 hours.
- For children at risk (difficult pregnancy, difficult childbirth, severe yellowness of the sclera and skin), blood is taken from the vein on the head.
This procedure is painless and safe for the child, although it is very scary for mothers. The sampling is carried out with a special thin needle by the hands of an experienced nurse; this analysis helps to diagnose the development of dangerous complications in time, so you should not refuse it in the maternity hospital.
- Children who do not have clear signs of jaundice are given a bloodless test - bilitest.

The analysis device is a photocell that records the skin color on the child’s forehead and thus determines the amount of yellow pigment. The result can be seen instantly. The disadvantage of this test is that it does not show direct and indirect bilirubin, and these numbers are very important for diagnosis.
With jaundice, babies undergo control tests throughout the entire treatment period until the pigment level decreases to normal.
Once again, a test for bilirubin in newborns is done in the clinic, during medical examination at one month of age. In this case, blood is taken from a vein on the head or on the arm, in different ways in different medical institutions.
Norm of bilirubin in the blood of newborns
An analysis for the amount of bilirubin is taken from a newborn in the first minutes of life from the cut umbilical cord, and then on the third day.
There are three types of enzyme: general, direct and indirect. At the beginning, indirect bilirubin is formed, which the body finds difficult to remove, so it transforms it into direct bilirubin.
| Age | Total (μmol/liter) | Indirect | Straight |
| At birth | 51 – 60 | 90 % | 10% |
| 2 – 7 days | Can go up to 256 | ||
| 21 day | 8,5 – 20,5 | ||
| Over 1 month | 8,5 – 20,5 | up to 15.4 µmol/l (75%) | up to 5.1 µmol/l (25%) |
| Age of the newborn | Amount of bilirubin (µmol/liter) |
| First day | Under 34 |
| Second day | 24 – 149 |
| Third – fifth days | 26 – 205 |
Such numerical variations are due to the fact that the baby is actively producing pigment, but is excreted much more slowly.
There are a lot of numbers, you can even get confused in them. But remember one thing: three hundred units of bilirubin is a critical level. It is at this moment that the child needs urgent medical assistance! Visually, any parent will determine the need for hospitalization - the child’s skin will be colored intense yellow.
- stimulation of labor;
- pathological course of childbirth;
- premature birth;
- infections and diseases of the mother during pregnancy;
- oxygen starvation of the child during childbirth;
- pregnancy diabetes;
- increased levels of female hormones in breast milk;
- Rh conflict between mother and child;
- stopping breastfeeding after childbirth;
- liver disease and disruption of its function in a newborn;
- intrauterine pathologies and developmental anomalies;
- genetically determined destruction of red blood cells;
- hormonal disbalance;
- intestinal obstruction in a child;
- significant weight loss in the neonatal period.

Bilirubin norms in children
Since the process of blood renewal occurs constantly, a safe amount of pigment is always present in the body. The norm of bilirubin in a one-month-old baby falls in the range from 8.5 to 20.5 µmol/liter. But for a newly born baby and in the next few weeks, these numbers are much higher. This situation occurs due to the breakdown of a large amount of fetal hemoglobin.
- The pigment content in the blood from the umbilical cord is considered normal:
- 51–60 µmol/liter in children born at term;
- 71.8–106 µmol/liter in premature babies.
Normal bilirubin level from birth to two months
Every body contains a component called bilirubin. The normal level of bilirubin depends on the age of the person. Everyone knows its activation - when a bruise goes away, a yellow spot forms in its place.
At birth, bilirubin is always higher than in an adult. This happens because in the mother’s womb the fetus does not yet breathe on its own; tissues are saturated with oxygen due to the woman’s cells. After birth, all received hemoglobin begins to be actively excreted, resulting in an increase in bilirubin.
A bilirubin test is taken from each newborn. Next in two days.
Normal bilirubin is divided into 3 types:
- Straight.
- Indirect
- General.
Initially, an indirect enzyme is present in the body, but it cannot be eliminated on its own, so over time, direct bilirubin is formed.
If at birth total bilirubin can reach up to 256, then by 2 months the norm is considered to be an indicator that ranges from 8.5 to 20.5 units.
The numbers vary greatly, and only a doctor can determine whether they are dangerous for the child. The main thing is that you should not ignore any changes occurring in the baby’s body. The most important symptom of increased bilirubin is unnaturally yellow skin. Its intensity can tell a lot even before donating blood for analysis.
Why does a child have high bilirubin and what is the danger of this condition?
When bilirubin is higher than the normal level (256 µmol/l in children born at term and 172 µmol/l in “hurried” babies), doctors talk about the development of jaundice. It comes in two types. Physiological jaundice most often ends on its own by the 4th week of a child’s life and does not have any consequences for his body.
However, children with this diagnosis need constant monitoring, as the disease can develop into a more severe form. Pathological jaundice requires treatment, and if it is not treated, it causes significant harm to the child’s health.
If bilirubin is increased in the blood of a newborn, the reasons may be the following:
- difficult pregnancy;
- maternal diabetes;
- complicated childbirth;
- premature pregnancy;
- lack of oxygen in the child during pregnancy or childbirth - for example, when the umbilical cord is entangled.
With pathological jaundice, bilirubin in the blood of children goes through the roof. The reasons for this increase may be the same problems that lead to physiological jaundice. Also, an extremely high level of pigment may indicate:
- liver problems in the baby;
- hormonal disorders;
- Rh conflict between mother and child;
- intestinal obstruction;
- a genetic disease leading to the destruction of red blood cell membranes;
- obstruction of the bile ducts.
Also, pathological jaundice can be caused by drugs that the mother received during pregnancy and childbirth.
When this condition is detected in a child, doctors treat not only the symptoms themselves, but also eliminate the cause of the disease.
Conditions that can cause pathological jaundice are themselves very dangerous and sometimes fatal. But high bilirubin in newborns cannot be ignored. This pigment is poison for the baby’s nervous system. When its level in the blood is high, bilirubin encephalopathy develops. Signs of this condition are:
- enlarged liver and spleen;
- decreased blood pressure;
- convulsive syndrome;
- the baby sleeps a lot or, on the contrary, is constantly on the move;
- The child practically does not take the bottle and breast.
Delayed treatment (or complete lack of help) for bilirubin encephalopathy can have the following consequences:
- hearing loss;
- developmental delay;
- motor paralysis
Sometimes bilirubin in a baby increases due to mother’s milk: the so-called “breastfeeding jaundice” develops. Milk contains fatty acids that prevent the liver from converting indirect bilirubin into direct bilirubin, and the toxin accumulates in the body. In this case, the children are transferred to formula feeding for two days.
If bilirubin decreases, then the child is left on artificial feeding. Or it is possible to feed the baby with mother's milk. To do this, you need to express it into a bottle and warm it up to a temperature of 70°, then cool it and give it to the baby. Learn more about how to properly express breast milk>>>
When heated, fatty acids are destroyed, and the milk will not harm the baby.
The danger of jaundice in infants
Physiological jaundice at birth is common. Usually everything goes away within 1-2 weeks. Sometimes bilirubin can make itself known only after seven days. This mainly happens because a nursing mother's breast milk has high levels of estrogen. Therefore, it is worth examining the baby for bilirubin. The normal bilirubin level for a two-month-old baby is from 8.5 to 20.5 units.
To recognize increased bilirubin, or physiological jaundice, you need to know the symptoms:
- when the body functions correctly, this condition appears 2-4 days after the birth of the baby;
- the duration of this period is no more than 10 days;
- yellow or orange skin color;
- the state is characterized within positive limits;
- the child’s activity and behavior are normal;
- urine and feces of unchanged color.
Depending on the reason for the jaundice, the treatment method is determined. Not only children, but also mothers are sent for examination. Jaundice, which is dangerous to the life and health of a child, is called pathological.
Its occurrence is influenced by several factors:
- lack of compatibility of the blood groups of the baby and mother.
- Childbirth that began ahead of schedule.
- Diseases of a genetic nature.
- Infections suffered by women during pregnancy.
The whole danger is that bilirubin can penetrate into the baby’s central nervous system. If this happens, doctors can diagnose bilirubin encephalopathy from the first day of life.
The symptoms are as follows:
- very low pressure;
- periodic cramps of the arms and legs;
- aversion to food;
- constant desire to sleep;
- yellowness of the skin may disappear after a while, but then return.
If such symptoms are left unattended, then by six months the child will become disabled. Increased bilirubin at 2 months is a serious pathology that requires urgent medical attention.











