While the baby is in the womb, its intestinal tract is sterile.
But as soon as the baby is born, various microorganisms enter the body.
Bifidobacteria and lactobacilli, as well as individual representatives of colibacteria, which can be classified as opportunistic, are considered beneficial.
With rapid reproduction, E. coli in an infant can cause a coli infection.
Reasons for the growth of E. coli in infants
Several types of pathogenic bacillus may be present in a child’s body – hemolysing and lactose-negative.
The latter belongs to the group of opportunistic pathogens, and in certain quantities it can be present in the body of an infant.
As for the hemolyzing bacillus, it can lead to serious disturbances in the functioning of the digestive tract.
The infection can enter the baby's body through the fecal-oral route. Hemolyzing bacillus can be passed through mother's milk during breastfeeding. Sometimes a child picks up an infection while in the maternity ward.
The main reason contributing to the development of E. coli in young children is reduced immunity. But even completely healthy babies can get an infection if they put dirty things in their mouths.
Therefore, parents should carefully monitor their children. Bottles should always be disinfected. If the pacifier falls on the floor, you must first wash it well and only then give it to the child. E. coli can also be transmitted through unwashed hands.
What causes E. coli in urine?
Escherichia appears in sterile urine for various reasons: pathological (indicate inflammation) and non-pathological (they are temporary and benign).
Non-pathological causes
Non-pathological factors (in a healthy person) include improper urine collection: an unsterile container, poor toileting of the genitals. In this case, it is necessary to conduct a repeat study.
Common reasons
Among the main reasons for the appearance of E. coli in the urine are infectious diseases of the kidneys and genitourinary organs:
- Cystitis.
- Urethritis.
- Vaginitis, prostatitis.
- Pyelonephritis.
Detection of Escherichia in the urine is usually accompanied by clinical symptoms: increased body temperature, painful and frequent urination, aching pain in the lower abdomen, discharge and discomfort from the genitals. In addition to these complaints, the patient notes changes in urine: unpleasant odor, impurities, mucus and clots. In some cases, bacteriuria is asymptomatic (during pregnancy, in children).
In infants
For children under 3 years of age, genitourinary infections are common. This is due to insufficiently developed immunity, anatomical features (short urethra), and non-compliance by parents with hygiene rules.
Symptoms

Most often, a child becomes infected with E. coli due to carelessness of parents.
If such a problem occurs, then you will need to be able to recognize the symptoms characteristic of the infection.
It will not be difficult to understand whether a baby has E. coli, since he will react acutely to the infection.
The main signs of the presence of E. coli:
- Hyperthermia. Infection is accompanied by an inflammatory process, and the body always fights it in the same way. Therefore, if parents notice a high temperature in their baby, then they should start to worry. As a rule, fever is accompanied by hyperemia of the extremities and general weakness.
- Loose stools are a symptom that accurately indicates the presence of an infection of intestinal etiology.
- Vomiting or excessive regurgitation.
- Restless behavior. The child becomes whiny, sleeps poorly, and refuses to eat.
Treatment methods
If you suspect infection in children under one year old, you should immediately call an ambulance, since it is possible to help a newborn if his body has been colonized by hemolytic E. coli only in a hospital setting. Pediatricians will definitely take tests - blood, urine, feces and vomit samples.
Children over one year old can be successfully treated at home according to the following scheme:
- Carry out antibacterial therapy. The best remedy is Nifuroxazide syrup, intended for the treatment of acute intestinal infections. You need to take it for 5-7 days in a dosage according to the instructions for the child’s age.
- Give the child a large amount of liquid (1-1.5 liters per day), prepared from special preparations for oral rehydration - “Regidron”, “Hydrovit”, “Humana Electrolyte”, “Maratonic”, “Gastrolit”, “Orsol”. WHO gives recommendations for preparing a similar solution at home: 1 teaspoon of table salt and soda, 1 tablespoon of sugar per 1 liter of water.
- Cleanse the body of toxins, since E. coli in infants can cause severe intoxication. The most effective sorbents are Enterosgel, Polysorb, Bactistatin, Smecta, Sorbex, Sorbolong. The method of administration and dosage are described in detail in the instructions for the drug.
- Help digest and absorb food. When infected with E. coli, enzyme deficiency often develops, so it is recommended to give the baby enzymes with food to improve digestion - “Mezim”, “Pancreatin”, “Creon”. Many pediatricians consider the latter drug to be the best.
- Restore normal intestinal microflora. Probiotics and prebiotics will help cope with this task. Probiotics are ready-made live microorganisms that normally inhabit the human intestines, and prebiotics are chemical compounds that create favorable microflora for the growth and reproduction of beneficial bacteria. During the first week, it is recommended to give the child probiotics - “Linex”, “Lactobacterin”, “Lactimak”, “Enterol”, “Bifiform”. During the second week, it is advisable to switch to prebiotics - Laktofiltrum, Goodluck, Duphalac, Lizalak, Fervital. By the way, breast milk itself is a unique natural prebiotic that helps restore the intestinal microflora in just 1-2 days, so this point can be skipped when treating breastfed children.
Follow a diet for two weeks so as not to put unnecessary strain on the liver and pancreas: cook porridge and soups in water, avoid fatty foods, limit meat, milk and eggs, exclude raw vegetables, fruits and juices.
With such therapy, even without antibiotics, the child should feel significantly better already on the 3rd day of treatment, and on the 5th day, recovery occurs in 90% of cases. For the next 2 weeks, it is recommended to take care of the body and do everything possible to help restore the immune system.
Diagnostics
If a baby develops the symptoms described above, parents should urgently show the baby to a doctor. To identify E. coli, it will be necessary to conduct a number of studies.

There are several methods to identify pathology:
- Bacterioscopy . The patient needs to donate blood, urine and feces. All analyzes obtained will be examined in laboratories using a microscope.
- Bacteriological research. Biological material taken from the patient is placed in a nutrient medium. If it contains pathogenic microorganisms, their number will rapidly increase.
Treatment of E. coli in children must be supervised by specialists. The duration of antibiotic therapy should not exceed 5 days. In addition to taking medications, it is very important to maintain a proper diet.
General recommendations for the treatment of E. coli in children:
- If an infection is detected, you should call a doctor as soon as possible.
- Most often, treatment can be carried out at home, but only with the consent of a specialist.
- In severe cases of the disease, hospitalization in a hospital is necessary.
Only after the type of E. coli has been identified and a diagnosis made, should the doctor prescribe appropriate treatment.
Variants of symptoms
There are no clinical symptoms characteristic only of hemolytic Escherichia coli. The priority role of this particular microbial agent as the main cause of the disease can only be confirmed as a result of laboratory examination.
All variants of clinical symptoms can be somewhat roughly divided into local and general.
General manifestations
They are noted only with a pronounced decrease in immunological resistance. Noted:
- increase in body temperature to low values (usually no higher than 38 ° C);
- weakness, increased fatigue;
- decreased performance, excessive unmotivated drowsiness.
Based on these signs, one can only suspect a systemic disease, but not establish its cause.
Local manifestations
Just like systemic changes, they are characterized by nonspecificity and polymorphism. It is convenient to consider possible clinical signs in accordance with the predominant localization of the bacterium.
| Localization of the bacterium | Local symptoms |
| Gastrointestinal tract |
|
| urinary system |
|
| Reproductive sphere |
|
Only a doctor can assess the severity of all signs, confirm the etiology of the pathological process and assess the need to eliminate hemolyzing E. coli.
Features of the course of the disease caused by this microorganism are usually not observed in children. It should be noted that in children under 3 years of age, complications develop in a shorter period of time: hypovolemic or infectious-toxic shock.
Therapy for lactose-negative Escherichia coli

Lactose-negative Escherichia coli belongs to the group of opportunistic bacteria. If the percentage of its content in the intestines does not exceed 5% of the total microflora, then it does not pose a danger, but, on the contrary, affects various processes:
- stimulates the production of vitamins belonging to group K and B;
- actively participates in metabolic processes;
- Helps the body absorb calcium and iron.
If the percentage of lactose-negative bacillus in the intestines exceeds the permissible norm, the following symptoms will be observed:
- the appearance of frequent regurgitation;
- increased gas formation;
- if the child is already receiving complementary foods, then particles of undigested food may be noticeable in the stool;
- abdominal pain;
- alternating constipation and diarrhea.
Experts believe that an increase in the percentage of lactose-negative bacillus in an infant is not a serious violation. To correct this, children are prescribed special medications that contain probiotics (for example, Bifidumbacterin) as well as prebiotics (for example, Hilak Forte).
How dangerous is the pathogen?
For a person with a normally functioning immune system, hemolyzing E. coli does not pose any danger. This is one of the permanent inhabitants of the mucous membranes of the body, which prevents the entry and proliferation of pathogenic microbial flora.
An important point is not only the amount of hemolytic E. coli, but also its ratio (percentage) relative to other representatives of the normal microflora of the human body. One should think about a serious danger for a person of any age only if dysbiosis develops - the number of cells of opportunistic microflora prevails over normal (non-pathogenic).
Among the complications that can be caused by hemolyzing E. coli are:
- various forms of intestinal infection (gastritis, gastroenteritis, gastroenterocolitis);
- inflammation of the genitourinary tract (cystitis, pyelitis);
- damage to the reproductive system (prostatitis in men, salpingoophoritis in women).
In addition, a severe course of intestinal infection is possible, which is complicated by hypovolemic or infectious-toxic shock.
Therapy for hemolytic Escherichia coli
Normally, a healthy child should not have a hemolytic bacillus in the intestines, and its detection in culture is considered by doctors as a pathological condition.
To cope with this problem, treatment is prescribed using sorbents and rehydration solutions.
The action of the drugs included in these groups is aimed at restoring the water-salt balance, because the appearance of hemolytic bacillus leads to serious disruption of the intestines.
In addition, the use of bifidobacteria, bacteriophages and probiotics is indicated.
Antibiotics are prescribed to children who have hemolytic E. coli very rarely, only in extreme cases. The doctor must take into account not only the general well-being of the baby, but also the results of the studies.
Antibacterial drugs not only fight the problem, but also destroy the bacteria necessary for normal intestinal function.
Determination of E. coli using a urine test
Escherichia from the intestine can migrate to other organs, primarily to the genitourinary organs (vagina, kidneys, urethra, prostate, bladder). Determination of Escherichia in urine is carried out by bacteriological inoculation of biomaterial. For this purpose, a small amount of liquid is placed on a nutrient medium (Petri dishes with agar-agar), on which microorganisms will multiply. The material is placed in a thermostat for a couple of days and after that the number of microorganisms is counted. The measuring units are considered to be CFU per 1 ml - colony-forming units that have germinated from 1 ml of urine. After inoculating the urine on Petri dishes, the sensitivity of the microbe to bacteriophages and antibacterial drugs is determined for further treatment.
The result of a urine microflora test will be ready in 5-7 days. Identifying e. Coli in urine analysis is a direct indicator of an infectious disease of the urinary organs.
General rules for preparing children for urine analysis

In order for the definition of bacteriuria to be reliable and informative, it is necessary to adhere to certain rules:
- The day before a urine test, you must not take medications, alcoholic beverages, coffee, or foods that color your urine.
- Purchase a disposable sterile container for collecting urine. Or use any dry and clean container, which has been previously scalded with boiling water.
- Collect urine in the morning on an empty stomach, and only morning urine should get into the container in the middle of urination (at the beginning and end of urination, urinate into the toilet).
- It is advisable not to go to the toilet the night before the test.
- Before collection, be sure to wash your genitals without using detergents. Do not collect urine during menstruation.
- It is advisable to fill 2/3 of the container volume (about 150 ml).
- The collected urine should be delivered to the laboratory as soon as possible (up to 2 hours); the temperature during transportation must be within 5-18°C.
Recommendations for preparing for the analysis of infants

For one-year-old children, there are certain recommendations when collecting urine:
- Since infants have a small amount of urine and uncontrolled urination, it is allowed to collect the entire portion of morning urine.
- 30-50 ml of urine will be sufficient for analysis.
- It is forbidden to pour urine from a potty or squeeze urine from a diaper or diaper.
- Before manipulation, thoroughly rinse and blot the external genital area. Girls need to be washed from front to back so that bacteria from the anus do not reach the genitals.
- If there is no urination, it can be stimulated by feeding the baby with a bottle, lightly stroking the suprapubic area, or using the sound of running water.
- You can collect urine from a baby by placing him over a container in the bathroom or using a special bag (urinal bag), which is attached with adhesive tape to the penis in boys and to the labia in girls. You can buy a urinal bag at a pharmacy.
Normal levels of bacteria in urine in children of different ages
Normally, urine is a sterile liquid, but in almost every analysis microorganisms are detected, and every second one will show e. Coli. The norm for Escherichia coli in urine is no more than 105 CFU (colony-forming units) per 1 ml. If, when taking the test, the patient has complaints characteristic of an infectious process, then up to 104 CFU/ml is considered normal.
Main symptoms: how to determine that a child has E. coli?
In a situation where E. coli, regardless of its type, begins to actively multiply, an imbalance of the microflora of the infant’s gastrointestinal tract occurs at the same time.
This is why the child’s behavior changes - he is capricious, is in a restless state, and has problems sleeping. In most cases, if pathogenic microflora multiplies in the gastrointestinal tract, this leads to the appearance of colic - paroxysmal severe abdominal pain, the appearance of which is usually noted after feeding.
When pathogenic microflora multiply, we can talk about a disease such as coli infection. This disease produces the following symptoms (all or some of them):
- The baby's abdomen becomes bloated and gas formation increases.
- Rumbling is constantly heard in the intestines.
- Food with certain disturbances passes through the gastrointestinal tract, so the baby spits up. He may also vomit more than once.
- Malabsorption syndrome may occur, in which the absorption of beneficial microelements by the small intestine is impaired.
- Diarrhea, foamy stools, and a characteristic putrid or sour odor from stool are often observed.
- The child either stops gaining weight or loses it altogether.
If a baby has fairly severe diarrhea, then dehydration is quite possible. This should not be allowed, so you should carefully check for the following symptoms: dry skin and mucous membranes, lack of urge to urinate, unusual calmness of the baby, drowsiness, lack of sweat and tears.
Bacteria in breast milk
Scientists from Spain are puzzled by the question of identifying all the bacteria that are found in breast milk. A study published in The American Journal of Clinical Nutrition found that the diversity of microorganisms in breast milk was much greater than expected, with more than 700 species of bacteria found. [1]
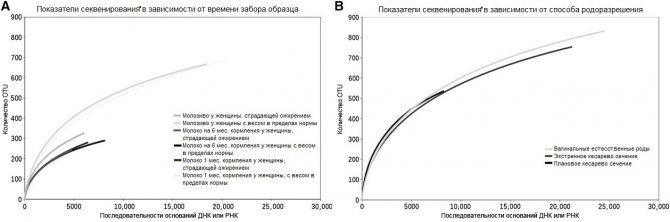
* Explanations for the graphs:
Sequencing is the general name for methods that allow one to determine the sequence of nucleotides in a DNA molecule. Read more here
DNA or RNA base sequence - the nucleotide sequence of a gene or genome
OTU - operational taxonomic unit (analogues of intestinal flora species)
The breast milk that newborns receive regulates the development of their own bacterial flora. The biological role of bacteria found in breast milk is still not fully understood, but it is already clear that it is extremely important for the successful development of the child. Breast milk contains a large number of beneficial bacteria that help babies absorb nutrients and develop their immune system.
In the course of their study, Spanish scientists identified bacteria in milk that belong to the healthy intestinal microflora (microbiome). They believe that microbial diversity in milk is due to several pre- and postnatal factors.
The researchers first turned their attention to colostrum, a newborn's first food, and found more than 700 different types of bacteria in it. Analyzes of colostrum samples showed that the most common types of bacteria in it were streptococci, lactic acid bacteria (Lactococcus), bacteria of the genus Leuconostoc, Weissella bacteria and staphylococci. [1]
Gram-negative bacteria Prevotella, Veillonella, and Leptotrichia were most often found in the breast milk of women who fed children aged 1 to 6 months. [1] At the same time, scientists noted that they are not yet able to determine how these bacteria get into milk. They can enter it from the baby's mouth after breastfeeding begins.
When first put to the breast, each newborn already receives its share of bacteria from breast milk, which ultimately colonize its digestive system. Now scientists are trying to find out how significant a role these bacteria play in the development of the child’s immune system and metabolism.
The conclusion reached by Spanish scientists is that many bacteria are present in milk by themselves and are not contaminants, and the microbiome of milk (the mass, or more precisely, the community of microorganisms inhabiting milk) depends on various factors and can be very different. Since bacteria from breast milk are one of the very first bacteria that enter the human body, the microbiome of milk is significant for the formation of human health, and its role in this process remains to be studied. [1]
Other Danish researchers, studying stool samples from more than 300 children collected at 9, 18 and 36 months, concluded that breastfeeding protects against obesity, diabetes, inflammatory bowel disease and allergies later in life, perhaps because that breast milk promotes the development of beneficial bacteria in the baby's intestines. And stopping breastfeeding, that is, stopping the child from receiving breast milk, leads to significant changes in the intestinal microflora and, at the same time, an increase in body mass index. [2]
Still others, in Canada, went even further and fed premature babies raw breast milk. The study examined the effect of milk containing bacteria on children, and how different the bacterial composition of the mother's and donor's milk is. Scientists at the hospital monitored the well-being of 98 premature babies who were fed their mothers' expressed milk and donor milk during the first 2 weeks of feeding. [3]
During the observations, it was noted that all 100% of children were exposed at least once to coagulase-negative staphylococcus, 41% to Staphylococcus aureus, and 64% were exposed to gram-negative bacilli. In donor milk, coagulase-negative staphylococci were found much less frequently than in mother's milk, and in lower concentrations, but Staphylococcus aureus and gram-negative bacilli were found in both donor and mother's milk with the same frequency.
The specific donor mother in this study was known for 75% of infant feedings. Most of the milk samples (77%) contained coagulase-negative staphylococci. The total number of samples in which coagulase-negative staphylococci were found was 5841 out of 7610 (each sample is one feeding of one child), 28% of them contained coagulase-negative staphylococci in quantities exceeding the norms of the milk bank. The prevalence of other staphylococcus species ranged from 0.01 to 5.6% of the milk samples participating in the study.
Gram-negative bacilli were found in 53% of milk samples, while 31% of women had only 1 type of these bacilli, 29% had 2 types, 14% had 3 types of gram-negative bacilli, 12% had 4 types, 8% had 5 types, 4% - 6 species, and 2% (1 woman) had 9 species of their own unique bacteria in their milk.
The results are presented in detail in the table below:
| Bacterium | Number of samples in which it occurred | % of the total number of samples studied | % of samples in which the number of bacteria exceeded the milk bank limit |
| Coagulase-negative staphylococci | 5841 | 77% | 28% |
| Viridans streptococcus (Streptococcus viridians) | 423 | 6% | 3% |
| Staphylococcus aureus (Staphylococcus aureus) | 307 | 4% | 94% |
| Nonhemolytic streptococci | 117 | 2% | 25% |
| Group B beta-hemolytic streptococci | 85 | 1% | 100% |
| Gram-negative bacteria Acinetobacter sp. | 232 | 3% | 89% |
| Pseudomonas fiuorescens group | 116 | 2% | 83% |
| Friedlander's wand (Klebsiella pneumonia) | 27 | 0% | 89% |
| Klebsiella oxxtoca (K. oxxtoca) | 54 | 1% | 91% |
| Ozaena stick (K. ozaenae) | 13 | 0% | 100% |
| Escherichia coli | 14 | 0% | 72% |
| E. hermannii rods | 31 | 0% | 100% |
| Enterobacter cloacae rods | 74 | 1% | 76% |
| E. agglomerans rods | 11 | 0% | 45% |
And then the researchers were surprised to discover that despite the fact that in some of the samples the number of bacteria exceeded the norms established by milk bank programs, this did not lead to any negative consequences for the children.
“There were surprisingly few, if any, adverse effects from ingestion of bacteria in raw breast milk.” [3] During the study, 10 newborns fell ill with bacterial infections, but in all cases it turned out that the infection occurred through a different route and with other strains of bacteria.
Finally, an excerpt from a WHO article on mastitis that addresses the issue of bacteria in breast milk: “Bacteria are often found asymptomatically in breast milk in both industrialized and developing countries. The spectrum of bacteria is often very similar in composition to skin bacteria. Marshall, for example, discovered Staph. epidermidis, diphtheroids, alpha-hemolytic and non-hemolytic streptococci. Thus, conducting bacteriological studies is complicated by the difficulty of avoiding the penetration of bacteria from the skin. Despite the use of special milk collection techniques for research, only 50% of milk cultures can be considered sterile, other samples contain “normal” bacterial colony counts ranging from 0 to 2,500 colonies per ml.” [4]
In summary, bacteria in milk is normal and they should be there, of course, if we are talking about milk that is safely expressed and carefully stored.
Author of the illustration: Tanya Russita
Sources
1. Raul Cabrera-Rubio, M Carmen Collado, Kirsi Laitinen, Seppo Salminen, Erika Isolauri, and Alex Mira “The human milk microbiome changes over lactation and is shaped by maternal weight and mode of delivery” https://ajcn.nutrition. org/content/96/3/544.full
2. Catharine Paddock PhD “Breastfeeding helps children grow friendly gut bacteria” https://www.medicalnewstoday.com/articles/276539.php
3. Barbara J. Law, Barbara A. Urias, Joy Lertzman, Diane Robson, And Lisa Romance “Is Ingestion of Milk-Associated Bacteria by Premature Infants Fed Raw Human Milk Controlled by Routine Bacteriologic Screening?” https://www.ncbi .nlm.nih.gov/pmc/articles/PMC267615/
4. https://www.who.int/maternal_child_adolescent/documents/fch_cah_00_13/ru/
Types of pathogenic bacteria
Scientists have found that even such necessary and healthy breast milk in some cases can contain microflora that is dangerous for children. The greatest danger is:
- Staphylococcus aureus;
- Staphylococcus epidermidis;
- Klebsiella;
- enterococcus;
- coli;
- shigella
Among the pathogenic bacteria often found in breast milk are Escherichia coli microorganisms and enterococci. They constitute putrefactive microflora and easily reach the baby when feeding through cracks in the nipples. The cracks are so small and invisible that they do not cause pain when breastfeeding the baby.











