16826
4
In this article:
- Reasons for development
- Epidemiology
- Clinical picture
- Treatment
- Prevention
- Useful video about enterovirus infection
Enterovirus infection in children is a very pressing problem. This is one of the most common infectious diseases transmitted at this age. That is why every parent needs to know what it is, how to recognize it and what methods of control, and most importantly, prevention can be taken. This article will clearly describe the symptoms and treatment of enterovirus in children.
What it is?
- enteroviruses - 4 types;
- polio viruses - 3 types;
- echoviruses - 31 types;
- Coxsackie viruses (A and B) - about 30 types.
All these viruses are very resistant to an acidic environment, so they can easily survive the attack of gastric juice and enter the intestines, where they begin to exhibit their pathogenic activity. In addition, these viruses can exist at normal room temperature for several days.

Symptoms
Recognizing enterovirus infection is not as easy as it seems. About 90% of polio infections occur covertly; almost half of the remaining enteroviruses also do not give any specific symptoms. Only a few pathogens are capable of producing a specific clinical picture, which allows one to suspect an enterovirus infection in a child:
- fever, increased body temperature;
- respiratory manifestations – runny nose, cough, sore throat;
- abdominal pain, diarrhea. This symptom is rare.
Typically, enteroviruses cause diseases that doctors conditionally divide into potentially severe and less dangerous. The first include encephalitis and serous meningitis, myocarditis and hepatitis. Less dangerous include fever with or without a rash, herpetic sore throat, conjunctivitis, pharyngitis, gastroenteritis, three-day fever.
Diagnosis, due to the vagueness of symptoms, is difficult. The doctor whom the parents call to the house can only make a presumptive diagnosis, but only laboratory tests will help to accurately answer the question of whether the child has an enterovirus infection and what particular virus has affected him:
- serological blood test;
- virological examination of blood and stool;
- molecular biological method for isolating enteroviruses from a laboratory sample.
Therefore, if a child has nothing but a fever, a feeling of aching muscles and a slight runny nose, the pediatrician will be right in assuming that the baby has an enterovirus infection.

Symptoms of the disease in children
Let's look at how the disease manifests itself. The infection enters the child’s body and begins to actively develop over several days. The virus then multiplies in the digestive tract. If you have a good immune system, the infection process stops at an early stage. As a result, the disease occurs in a milder form and does not cause much discomfort. It is important to note that with a cold and problems associated with the respiratory tract, young children immediately become infected with this unpleasant disease. Sometimes the virus spreads throughout the body and enters the bloodstream, leading to:
- fever,
- headache,
- vomiting
- diarrhea
- abdominal pain
- high temperature
With such symptoms, doctors often call the infection “summer flu.” Although all these signs indicate the spread of enterovirus infection. It should be noted that some strains of enterovirus also cause a generalized, vague skin rash or mouth ulcer. This type of disease is the most common enterovirus infection. Rarely, the development of an unpleasant illness begins from this stage. The virus can harm various internal organs and lead to serious complications.
The infection is transmitted by sexual contact, airborne droplets, water, fecal-oral and vertical routes. The incubation period lasts from two to seven days. If a terrible disease occurs, there is a possibility of the temperature rising to 40 degrees. The treatment course lasts from two to three weeks, depending on the child’s body.
To diagnose enterovirus infection prematurely, doctors examine the person’s general condition and monitor the degree of development of the disease. If a rash or ulcer is observed on the body, then the patient is prescribed an individual course of treatment using certain medications. Doctors may require a blood test or send samples taken from the throat, stool, or spinal fluid to a laboratory for culture and testing.
Enterovirus infection is usually eliminated under the supervision of a qualified specialist. If you miss the disease and do not carry out appropriate treatment, then you can cause enormous damage to the cardiovascular or nervous system. Sometimes improper treatment can be fatal. However, in the case of children, such treatment for enterovirus infections is aimed at relieving symptoms.
Transmission routes
Enteroviruses enter the body most often through the mouth - with dirty hands, water, and food. A child can easily become infected from a sick person through airborne droplets. Most often, outbreaks of infection occur in summer and early autumn. In cities and countries with hot climates, outbreaks and even epidemics are observed more often than in northern latitudes.
This implies a fairly wide geographic distribution of enteroviruses in resort towns and on popular, crowded seashores. In 2020, the Coxsackie virus was rampant in Turkey, and in 2000, the ECHO virus affected hundreds of people in Singapore and Taiwan. From time to time, small outbreaks are also recorded on the Black Sea coast in Russia. However, this does not mean that there are no such viruses far from the sea and sun. They are widespread everywhere.

Treatment
Evgeniy Komarovsky argues that calling enterovirus infection intestinal is not entirely correct. That is, it is essentially intestinal, but is strictly viral in origin. Whereas an intestinal infection, in the broad sense of the word, can be caused by both toxins and bacteria.
It follows that enteroviral diseases should be treated according to all the rules for the treatment of viral infections. This means that antibiotics are contraindicated because they do not have the slightest effect on viral particles. At the same time, they increase the risks of secondary complications, including those affecting the central nervous system.
There are special drugs against enteroviruses; this virus cannot be defeated with universal antiviral tablets. Quite often, doctors recommend products that belong to the groups of interferons and immunoglobulins.
However, many doctors are disingenuous, saying that the pills will definitely help the child. Most doctors know that immunoglobulins show relative clinical effectiveness only when given intravenously and only in certain groups of patients - newborns and people with HIV infection.

- the microclimate in the room should be favorable - the air temperature is from 18 to 20 degrees, regardless of the time of year, and the relative humidity is 50-70%;
- drinking plenty of fluids at body temperature - under such conditions the liquid is absorbed faster;
- saline rinsing of the nose and nasopharynx in the presence of respiratory symptoms (runny nose, cough) - every half hour if the child is not sleeping;
- thorough ventilation of the room, frequent wet cleaning;
- in the absence of fever - walks in the fresh air.
Prevention
There is no specific prevention against enteroviruses. There is not a single medication that can be used to reduce the risk of infection, although some sources indicate antiviral drugs of the interferon group as a prophylactic agent. This statement, from the point of view of evidence-based medicine, has no real evidence, says Evgeny Komarovsky.
Vaccinations against enteroviruses as such have not been developed, with the exception of vaccines against polio and hepatitis. But there are more varieties of viruses, as well as the diseases they cause. After illness, immunity to most enteroviruses develops lasting and lasts for several years.

In the next video, Dr. Evgeniy Komarovsky talks about enterovirus infection in children.
medical reviewer, psychosomatics specialist, mother of 4 children
Enterovirus infection in children is a disease that affects internal organs. Various symptoms appear, there may be damage to the digestive tract or signs of respiratory diseases.

The causative agents of the infection are intestinal viruses, the incubation period is from three to ten days. The level and severity of the disease varies from country to country.
Diet for enterovirus
The functioning of the gastrointestinal tract during a viral illness is difficult, so it is very important to pay special attention to the selection of nutrition. Diet for enterovirus infection in children involves the following points regarding nutrition:
- drinking plenty of fluids will help remove toxins as quickly as possible and will also be an excellent prevention of dehydration;
- food for children can be in the following options: boiled, stewed, baked in the oven, low-fat, pureed, crushed;
- a categorical ban on everything spicy, smoked, salty, fried and sweet;
- Eggs, whole cow's milk, butter and vegetable oils are excluded from the menu;
- prohibition of any carbonated drinks;
- you can consume fresh fermented milk products (biokefir, low-fat cottage cheese);
- vegetables and fruits only in the form of dishes;
- Meat broths, nuts, legumes and fresh bread are prohibited;
- You should eat small meals and eat at least 6 times a day;
- The baby should be fed warm food;
- If there is no desire on the part of the child to eat, you should not insist, and you should also not overfeed.
If a child has no appetite, then there is no need to force him - in this case, the body itself knows its needs better.
The acute form of diarrhea requires more strict dietary restrictions and adherence to the following diet:
- Hungry pause. Taking a short break from eating will be very helpful. Spending the whole day hungry or skipping at least one or two meals would be quite appropriate. For infants, of course, such fasting breaks are contraindicated. Increase pauses between meals in proportion to the child's age.
- Strict diet. On the first day you can eat porridge cooked in water, baked apples and crackers. The next day, you can gradually begin introducing fermented milk products, pureed vegetable soups, and boiled potatoes. Lastly, you should leave low-fat meat and fish dishes in the form of meatballs, meatballs and steamed cutlets.
For acute diarrhea in children, the following drink options are possible:
- dried fruit compote (preferably pear);
- decoction of chamomile flowers;
- berry jelly from dried fruits (preferably blueberries);
- weak green tea;
- raisin broth;
- alkaline water without gas.
Let us remind you once again that drinks should be offered often, but in small portions. A variety of drinks will allow even the most demanding patient to drink liquid.
Warm dried fruit compote is perfect as a restorative drink.
Causes
The causes of infection are intestinal viruses, classified into the following categories:
- 23 types of Coxsackie A virus;
- 6 types of Coxsackie B virus;
- types 1, 2 and 3 of poliovirus;
- from 68 to 71 types of enteroviruses;
- 32 serovars of ECHO viruses.
Viruses can live in the external environment for two months, remaining quite viable. After heat treatment they die instantly. That’s why it’s so important to prepare foods correctly and thoroughly.
The source of infection is a healthy or sick virus carrier - a person. The virus is transmitted by airborne droplets or fecal-oral routes: being nearby a sneezing or coughing virus carrier, not following hygiene rules - dirty hands while eating and after walking. A vertical route from an infected mother to the fetus is very likely.
Enteroviral infections are seasonal. Most often, symptoms are observed in the autumn-summer period. The age category is also specific: children, young people and middle-aged people. After an illness, the body develops immunity. The gateway for the virus is damaged mucosa.
Classification and symptoms
Enteroviruses are one of the causative agents of acute respiratory infections. Symptoms are most severe in individuals with acquired immunodeficiency syndrome. The infection is fraught with serious complications in newborns, which is why timely diagnosis of the infection, which most often occurs asymptomatically, is so important.
When classifying an infection, several types of disease are distinguished, taking into account the location and symptoms that appear:
Main symptoms: disruption of the gastrointestinal tract. Frequent watery stools (diarrhea), abdominal pain, painful bloating. Possible signs: nausea, vomiting. General state of weakness, apathy and lethargy. Appetite decreases, temperature rises to 38⁰, and sometimes a rash appears.
In children under 2–3 years of age, the gastroenteric form of intestinal infection can be combined with the respiratory one. The painful condition lasts up to two weeks in newborns and infants. Children over three years old cope with the virus in three days, the rash disappears quickly.
There is a strange paradox: enteroviral fever most often manifests itself in the overall picture of signs of intestinal infection. But this form is rarely diagnosed due to the lack of local symptoms. Main symptoms: fever for a period of no more than four days, moderate symptoms of intoxication, health is often normal, a rash is possible, sometimes nausea and vomiting.
Another name is Boston fever. From the very first days, a reddish rash appears on the child’s body. After a couple of days, the rash completely disappears. Enteroviral exanthema is characterized by the possible manifestation of symptoms of herpetic sore throat, vesicular pharyngitis of the throat, conjunctivitis, and sometimes uveitis. In rare cases, central nervous system disorders are possible: infectious meningitis, encephalitis, polyradiculoneuritis, facial neuritis.
Rare forms in newborns and consequences: encephalomyocarditis, myocarditis, renal dysfunction and MPS. How long the illness will last and what the consequences are depends on each individual case.
Classification and forms of the disease
Detection of symptoms and treatment of enterovirus infection in children requires high professionalism from doctors and the mandatory use of laboratory diagnostic methods. The main problem is the variety of diseases that are caused by enteroviruses. Doctors divide them into typical and atypical.
Interesting! How to get rid of worries and stress?
So, the first category includes:
- epidemic myalgia;
- herpetic sore throat;
- enteroviral exanthema;
- serous meningitis.
As for atypical manifestations of the activity of intestinal viruses, such rare forms include:
- pancreatitis;
- polio;
- myocarditis;
- gastroenteritis;
- cystitis;
- nephritis;
- uveitis;
- orchitis
The virus, after entering the body and multiplying on the mucous membranes of the oral cavity or gastrointestinal tract, can be transferred through the bloodstream to any organ of the body, causing specific symptoms.
Enterovirus infection in children, the symptoms and treatment of which differ depending on the types of viruses that act as its causative agents, occurs in different forms, distinguished by different symptoms and consequences. Among all forms of enteroviral disease, common and rare forms are distinguished.
Frequent (typical) forms
- Catarrhal (respiratory) form - occurs mainly in children from 3 to 10 years old and the symptoms are almost no different from ordinary ARVI. These include a sharp increase in temperature, a sore throat when swallowing, and the appearance of painful blisters on the back of the palate and pharyngeal walls, which subsequently burst, forming open small and painful ulcers. This form lasts from 5 to 7 days.
- Flu-like form - has symptoms typical of ARVI: nasal congestion and swelling of the throat, runny nose, temperature rises to 38 degrees, pain in the head and muscles, weakness and lethargy. There are also symptoms typical for enterovirus that help distinguish this form from regular flu: nausea with vomiting, diarrhea and general stool upset. This form almost always occurs when infected with an intestinal infection and lasts from 3 to 7 days.
- Intestinal is one of the most common and dangerous varieties. It is characterized by a moderate rise in temperature to 38 degrees and is accompanied by extensive diarrhea, with a frequency of 5 times a day. Accompanied by pain and bloating, vomiting and flatulence. The main threat with these symptoms is dehydration, which complicates the general condition of the child. The form lasts from 3 to 7 days.

Enerovirus infection in children may be accompanied by a rash as a symptom, or may be an independent disease. Therefore, treatment depends on one form or another - Enteroviral rash (exanthema) - most often appears in children aged 1 to 6 years. It has 2 types - rubella-like and roseola. A rash appears on the child’s body and face already on the 1st or 2nd day of illness. It looks like red rashes that form uneven bright spots, sometimes with the appearance of vascular elements. This form mainly occurs in the summer.
Rare and severe forms:
- Enteroviral fever is characterized by headache and muscle pain, redness and inflammation of the throat (possibly ulcers), redness of the face and, in rare cases, enlargement of the liver and spleen. This form lasts no more than 3-4 days and passes without complications. An uneven course with subsidence and exacerbations is possible over 8-10 days.
- Epidemic myalgia - accompanied by severe muscle pain and a strong increase in temperature. Pain in the back, abdomen, chest or headache, pallor, increased sweating, and intermittent breathing may also occur.
- Hemorrhagic acute conjunctivitis - includes photophobia, increased tearing, eye pain and loss of clarity of vision.
- Meningitis is one of the most severe forms of enteroviruses. It is indicated by a sharp increase in temperature up to 40 degrees, acute headache, frequent and profuse vomiting, steely abdominal pain, cramps and the appearance of mesh rashes of spider veins.
Treatment
Epidemiology does not imply treatment of infection in each specific case with specific drugs. A sick child is contagious and is treated at home for the entire period, taking medicine and keeping bed rest until the temperature subsides in order to exclude complications after infection in newborns. How long the illness lasts depends on the child’s immunity.

How to treat the infection? Antiviral drugs and antibiotics are prescribed only in case of concomitant bacterial infection. In a hospital setting, treatment is carried out for children with complications in the central nervous system, heart, liver, MPS and kidneys. In such cases, the appropriate antibiotic must be selected.
Epidemiology involves not only treatment with medications, but also adherence to a special gentle diet. You need to drink plenty of fluids; prolonged diarrhea and vomiting can cause dehydration.
If the disease is mild, antibiotics are not prescribed, only antiviral drugs. Epidemiology practices treatment with drugs that relieve the symptoms of sore throat (sprays, rinses). Antipyretics are used to reduce the temperature. Diarrhea is treated with rehydration.
Epidemiology is aimed at the study of viruses, including intestinal ones. Treatment of all manifestations is carried out under the strict supervision of a doctor who prescribes medications and monitors the dynamics. Sick children are subject to complete isolation to avoid the spread of the virus.
Epidemiology involves treatment by following the strictest dietary rules. Nutrition is aimed at eliminating dehydration, which is possible with symptoms such as diarrhea and high fever. The diet includes several important points.
- It is necessary to drink liquid every hour in small doses.
- A strict ban on fried, fatty and spicy foods, including pickles.
- A gentle diet is recommended. You can only eat low-fat pureed foods: vegetable soups, purees.
- Fresh vegetables and fruits, milk and dairy products are strictly excluded. Vegetables can be boiled, stewed and baked, pureed into a soft puree.
- The diet of a sick child excludes foods that increase peristalsis - this can cause painful diarrhea.
- Plan your diet so that meals are as fractional as possible. It is best to feed a sick child 5-6 times a day and give more fluids.
- One of the negative aspects of infection is diarrhea and putrefactive processes. To remove toxic elements from a child’s body, you need to include baked apples in the menu.

Diet for enterovirus infection
In addition to all treatments, it is necessary to follow a proper and strict diet, and only with such complex treatment can quick results be achieved.
You should exclude juices, carbonated waters, dairy products, vegetables and fruits from your diet. You can eat:
Low-fat chicken broth;
Porridge, buckwheat or oatmeal and not with milk;
Steamed omelette;
A little chicken or turkey meat;
Crackers;
Decoctions or fruit drinks from blackcurrant or rosehip;
Carrots and zucchini only boiled.
Prevention
The best prevention of enterovirus infection is personal hygiene. It is necessary to teach a child from infancy to wash his hands after a walk, visiting the toilet and before eating. Children must have individual dishes and bath accessories: towels, soap.
There are no special methods of prevention. Cleanliness, daily wet cleaning of the premises, isolation of sick children and healthy ones until the incubation period expires are the most effective methods that will protect against infection.
Enterovirus infection is a group of anthroponotic acute infectious diseases caused by enteroviruses.
The pathology has different forms and a number of clinical manifestations, among which fever comes first. The disease can occur with damage to the central nervous, cardiovascular, digestive, respiratory or muscular systems. In many children, the skin and mucous membranes are involved in the pathological process.
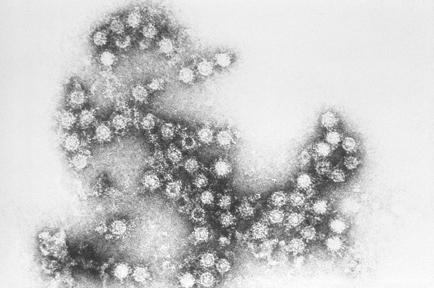
Enteroviruses belong to the picornavirus family. All representatives of this class have their own RNA chain. This means that all genetic information is contained in RNA, and not in the DNA of viruses, as is typical for other viral pathogens.
What it is?
Enterovirus infection is a whole group of diseases. In most cases, children suffer from it; adults get sick less often.
The specificity of the disease is such that after it is transferred, the body develops lifelong immunity. But it is worth considering that immunity is formed only to the type of virus that provoked the development of pathology. This is why children can get enterovirus infection several times, but in each case they will have a predominant symptomatology. For the same reason, there is no vaccine against EVI yet.
This pathology mainly affects children 3-10 years old. However, newborn babies who are breastfed are also susceptible to the disease, despite the immunity that they receive along with their mother's milk.
Transmission routes and pathogens of EVI
Enteroviruses are a large group of viruses that provoke polysymptomatic diseases in children. However, most often the causative agents of these pathologies are echoviruses and Coxsackie viruses. The group of EVs also includes polioviruses, the causative agents of poliomyelitis. But there are also those that do not belong to any of the above groups. In general, there are 70 main viruses that provoke the development of EVI, but in 75% of cases the disease develops under the influence of 10 viruses.
The causative agents of the disease are ubiquitous. They are very resistant to the external environment and low temperatures. The activity of viruses is not affected by ethyl alcohol, Lysol or ether. They die only when exposed to high temperatures (50 degrees and above), drying, exposure to formaldehyde or chlorine-containing disinfectants.
Most often, enteroviruses are detected in water, soil, some types of food and the human body. In feces, these organisms can remain viable for about six months.
Enteroviruses are transmitted in 5 ways:
- oral-fecal;
- vertical (from mother to child during childbirth or during pregnancy);
- contact and household;
- airborne;
- aquatic (when swimming in polluted waters where EVs live).
There have been recorded cases of infection with enteroviruses when drinking water from coolers.
EVI is characterized by seasonal outbreaks, which usually occur in the summer-autumn period. But children are often diagnosed with diseases of enteroviral etiology, regardless of the time of year.
How does infection occur?
Infection occurs in several ways: water, food, household contact, airborne droplets (from sneezing and coughing) and through the mother’s placenta. Transmission factors include water and vegetables infected with enteroviruses. The virus can also be transmitted through dirty hands, toys and other environmental objects. Most often, infection occurs through water, by drinking unboiled water or swallowing water from reservoirs.
The incidence of the disease in children is significantly higher than in adults.
The virus enters the environment from a sick person or from a virus carrier (a person who does not have clinical manifestations of the disease, but has the virus in the body). Virus carriage can last up to 5 months and sometimes forms after an illness or in people with stable immunity in whom the virus, having entered the body, could not cause the disease.
Breastfed children have immunity in their bodies, received from the mother through breast milk, however, this immunity quickly disappears after stopping breastfeeding.
Classification
Enterovirus infection has a fairly broad classification. Depending on the severity of the clinical picture, EVI can be:
- asymptomatic - no ailments are noted in children;
- manifest - in this case the clinical picture is quite pronounced, a whole range of symptoms is observed.
Depending on the severity of the disease, the disease is divided into 3 stages:
Criteria for the severity of EVI are based on the severity of the intoxication syndrome and local changes. In addition, enterovirus infection can occur in the following forms:
- sharp smooth;
- uncomplicated;
- complicated;
- recurrent.
EVI is a disease that occurs under the guise of other pathologies. Most often it manifests itself in the form of:
Enteroviral meningitis in children under 3 years of age is diagnosed extremely rarely. Most often, it affects young school-aged patients.
Enteroviral encephalitis is diagnosed only in 3-8% of cases, and can be combined with meningitis (meningoencephalitis). In children 1-3 years old, cases of paralytic forms of EVI are quite common. They develop less frequently in preschoolers aged 5 years and schoolchildren aged 6-7 years. However, this type of enterovirus infection has a benign and favorable course.

How dangerous is enterovirus infection?
What is enterovirus?
Enterovirus infection is a large group of pathogens. Different organs and systems are affected, depending on the type of enterovirus. The pathogens have minimal sizes and persist for a long time in food and in the environment. They easily reproduce in tissue cultures, but die at temperatures above +55 degrees or under the influence of substances containing chlorine.

Main routes of infection
Enterovirus infection penetrates through the mucous membrane of the digestive tract or through the respiratory tract. Here the virus begins to multiply and provokes an inflammatory process, which immediately paints a clinical picture of the disease. If treatment is insufficient or absent, enteroviruses continue to spread and multiply in other organs and tissues. When they get into areas of the central nervous system, damage is observed with a deterioration in the patient’s condition up to severe.
Main features
Enterovirus infection has an incubation period lasting from 2 to 7 days. The disease has an acute onset: the temperature rises sharply, chills and headache appear. Externally, there is pallor in the area of the nasolabial triangle and redness of the mucous membrane of the eyes, lips and cheeks acquire a bright shade. The gastrointestinal tract is characterized by such manifestations as nausea, vomiting, constipation or diarrhea, and almost always abdominal pain. Most often, the disease progresses quickly, within a few days. There is a tendency to relapse (up to several times).
Forms of the disease
Enterovirus infection can manifest itself in different ways, depending on the type of virus that provoked the disease. In childhood, herpetic agina, aphthous stomatitis, and serous meningitis are most often observed. During this period, collective outbreaks are characteristic, especially in the summer-autumn season. Often there is a complex of symptoms of the disease, i.e. it is possible, for example, that the intestinal form may occur simultaneously with herpetic sore throat. Similar phenomena can occur in adulthood.
Diagnostics

In the general blood test, a slight increase in lymphocytes is observed. In rare cases, leukocytosis is possible, which then gives way to eosinophilia and lymphocytosis. ESR remains within reasonable limits. A blood test using ELISA detects the virus in the first days of the disease. Virologists collect swabs from mucous membranes affected by the virus. Enterovirus infection, the symptoms of which are similar to many diseases, is still classified as a separate group of diagnoses. Its treatment must be carried out by a qualified specialist.
Enterovirus infection: treatment
There is no specific drug or treatment against enterovirus. The main goal is to relieve symptoms and prevent complications. Children with the most pronounced signs of the disease are subject to mandatory hospitalization. Persons who were in contact with the patient are observed and, if necessary, removed from collective communication.
Symptoms
Hyperthermia often has an intermittent character. This means that the next rise in body temperature may be followed by its independent decrease until complete normalization. But such changes are temporary and appear over different periods of time. General symptoms of intoxication of the body are not uncommon - weakness, body aches, lethargy, drowsiness, sweating, etc.
Other common symptoms of enterovirus infection in children include:
- arrhythmia, which may be accompanied by tachycardia (increased heart rate) or bradycardia (decreased heart rate);
- slight weight loss;
- numbness of the limbs;
- pain in the bones, pelvis, genitals and/or chest;
- myalgia;
- arthralgia;
- visual disturbances;
- enlarged lymph nodes.
Symptoms of enterovirus infection can be divided into safe and potentially dangerous. The list of the most dangerous manifestations of EVI in a child includes:
- myocarditis;
- pericarditis;
- anicteric form of hepatitis;
- serous form of meningitis;
- acute paralysis;
- kidney damage;
- sepsis (most often develops with EVI in newborn infants).
The list of less dangerous manifestations of enterovirus infection can include:
- a three-day fever, which may be accompanied by skin rashes;
- development of gastroenteritis (inflammation of the gastrointestinal tract with all accompanying symptoms);
- herpetic sore throat;
- lymphadenopathy – enlargement of lymph nodes and their soreness;
- polyradiculoneuropathy;
- enteroviral conjunctivitis;
- damage to the optic nerve;
- inflammation of the ocular choroid;
- vesicular pharyngitis (its symptoms are very similar to herpetic sore throat, but in this case the inflammatory process affects the back wall of the pharynx).
Important! When enterovirus type D68 enters the body of a young child, the sick child may develop bronchopulmonary obstruction. Its main symptom is a severe cough and difficult, wheezing breathing.
In children, EVI in the vast majority of cases occurs in the form of a common acute respiratory infection, and is accompanied by:
- runny nose;
- difficulty in nasal breathing;
- pain in the throat, ears, nose;
- cough;
- shortness of breath;
- whistling sounds during inhalation/exhalation.
With herpetic sore throat, concomitant with enterovirus infection, babies may suffer from:
- febrility;
- severe sore throat;
- headache;
- sleep and appetite disorders;
- pain while swallowing.
A characteristic symptom of herpetic sore throat is the formation of papules on the mucous membranes of the soft and hard palate. After some time, they turn into vesicles filled with pathological contents. They may have a white or yellowish tint.
Important! Under no circumstances should you try to puncture or squeeze out the vesicles! This approach to the treatment of herpetic sore throat accompanying EVI is fundamentally incorrect and extremely dangerous. It can lead to the spread of infection and aggravation of the pathology in the child.
Often, herpetic sore throat is complicated by the addition of a secondary (bacterial) infection. It is possible that other symptoms of enteroviral disease may occur in children.
Enteroviral disease in children often occurs in the form of an acute intestinal infection. In this case, patients experience symptoms such as:
- bloating;
- backflow of stomach contents into the esophagus (reflux);
- nausea;
- pain in the epigastric zone;
- pain in the lower abdominal segment;
- diarrhea;
- nausea (with or without vomiting);
- constipation
Appetite disturbances, flatulence, change in stool color - these symptoms can also accompany the intestinal form of enterovirus infection in children of all ages.

Neurological and psychological disorders due to enterovirus infection are observed in children less frequently than intestinal or flu-like symptoms. But, nevertheless, they are possible, and parents should be able to recognize them. They appear:
- anxiety and worry;
- depression;
- impaired memory, attention;
- sleep disorders.
With a significantly elevated body temperature, confusion may occur. In this case, you must immediately call a doctor.
The most dangerous form of enterovirus infection in young children is serous meningitis. It is accompanied by:
- photophobia (fear of bright light);
- an increase in body temperature to febrile and pyretic levels (38 - 40 degrees);
- vomiting;
- anxiety, anxiety, nervousness of a sick child;
- stiff neck;
- decreased abdominal reflexes;
- severe pain in the abdominal area;
- hypersensitivity to loud and sharp sounds;
- severe headache when tilting the chin to the chest;
- lethargy, loss of strength;
- apathy;
- muscle cramps.
Some children experience psycho-emotional agitation. But it is not a specific symptom of serous meningitis that accompanies enterovirus infection. Along with this, oculomotor disorders, confusion, myalgia (muscle pain), and increased tendon reflexes may be observed.
Symptoms of enteroviral serous meningitis can last from several days to 2 weeks. However, signs of infection may be present in the cerebrospinal fluid for another 14-21 days from the moment the clinical manifestations of the disease disappear.
Damage to the ocular conjunctiva during enterovirus infection is usually combined with other forms of the disease, and manifests itself:
- pain or pain in the eyes;
- photo sensitivity;
- intense lacrimation;
- redness of the conjunctiva and eyeball;
- swelling of the eyelids – lower and/or upper;
- the appearance of serous or purulent discharge, which accumulates in the corners of the eyes (after waking up, you may notice that the child’s eyelids are stuck together and he cannot open his eyes).
It is worth noting that with enteroviral conjunctivitis, only one visual organ is primarily affected. But with improper treatment or complete absence of it, the infection spreads to the second eye.
Enteroviral fever is characterized by the development of a febrile state. It usually occurs 3 days after the onset of the pathological process. During this period, the sick child exhibits general signs of intoxication of the body, but they are not as pronounced as in the flu-like form of EVI.
Some babies with enterovirus fever experience skin rashes. Deterioration in general health manifests itself in a mild or moderate form.
When the first symptoms of an enterovirus infection appear, the child should be immediately taken to the pediatrician. If the body temperature or general condition of the patient does not allow this, you should call a doctor at home.
Clinical picture
The virus penetrates through mucous membranes. The specific location depends on how the pathogen enters the child’s body. That is, when airborne droplets are carried out, the first sign will be manifestations from the respiratory tract. Accordingly, if there is a fecal-oral mechanism, then the symptoms of enterovirus in children will appear from the intestines.
After active reproduction on the mucous membrane of the corresponding area, the virus enters the lymph nodes of this region, where it continues its vital activity. This stage is especially important, because if the child’s immune system fails to destroy the pathogen here, it will begin to spread throughout the body. The further cycle depends on the specific pathogen. The fact is that everyone has certain general symptoms, but a specific type is characterized by effects on certain organs and tissues.
When an infectious agent enters the body, it does not immediately provide external signs of the disease. The period before the first symptoms is called incubation. For enteroviruses, its value ranges from two to ten days, with an average of five.

The onset of infection is always characterized by fever, reaching 39 degrees. Such numbers can last up to five days, and then they normalize. It happens that the temperature curve has a wave-like character: periods of normal values are replaced by elevated ones. This entire period is accompanied by lethargy, drowsiness, patients complain of headache, nausea and vomiting. At this stage, parents may already suspect the need for treatment of enterovirus in children. In addition, when the pathogen enters through the respiratory system, enlarged lymph nodes in the neck can be detected.
With widespread damage to the body, the following organs and tissues may be involved in the process:
- nervous system (both central and peripheral);
- upper respiratory tract (nasopharynx and oropharynx);
- eyeballs;
- muscle;
- heart;
- intestines;
- liver;
- testicles.
If the virus infects the oropharynx, the disease develops as a sore throat. Body temperature rises, signs of intoxication such as headache, lethargy, pain in muscles and joints are noted. In this case, the rash due to enterovirus infection in children covers the arches, the tonsils themselves, and adjacent areas of the mucosa. It consists of blisters that subsequently burst open, and in their place small ulcers with a whitish coating appear, after healing of which no scars remain.
A characteristic manifestation is conjunctivitis with all its characteristic symptoms such as lacrimation, redness of the eyes, and photophobia. In addition, there is some swelling of the eyelids and vascular injection.
Myositis also occurs when muscles are involved in the process. Their pain is related to the intensity of intoxication: the greater it is, the more the muscle tissue hurts. Especially often the primary affect is intestinal damage. A characteristic symptom is enteroviral diarrhea in children with unchanged stool color and without impurities, as well as abdominal pain.
In relation to the heart, we can talk about the development of myocarditis, and inflammation spreads to the valves with the inner membrane when endocarditis develops. If the entire organ is affected, then we are talking about pancarditis. All this entails serious consequences of enterovirus infection in children with arrhythmias and even valve defects in the future with poor quality treatment.
Dangerous situations occur when the virus reaches nerve tissue. In this case, encephalitis, meningitis and other neurological diseases develop. In addition, convulsive syndrome, paresis of the limbs, and loss of consciousness may occur. On the part of the liver, hepatitis may develop. The testicles are also affected in the form of their inflammation, when they are painful and enlarged. And don’t forget about the rash that often appears on the body with this disease. All this determines the importance of treatment of enterovirus infection in children.
Diagnostics
To begin with, a child with symptoms of an enterovirus infection must be taken to see a pediatrician. If the symptoms of the disease are varied, then parents and their sick child may be referred to specialists in other fields:
- ophthalmologist;
- neurologist;
- pulmonologist;
- dermatologist;
- cardiologist;
- surgeon;
- nephrologist;
- gastroenterologist.
To identify and determine the type of EVI pathogen, a blood test is performed using one of 4 methods:
- Immunochemical. This procedure allows you to identify specific antigens in the child’s blood.
- Serological. Infection is determined by the presence of specific substances - immunoglobulin markers.
- Molecular biological. They are aimed at identifying viral RNA in the patient’s blood.
- Virological. Using this technique, enteroviruses are determined by urine, blood, feces or scrapings taken from the mucous membranes of the child’s mouth or throat.
Along with this, a general clinical blood test is also performed. If the diagnosis of enterovirus infection occurs, then the following deviations will be noted in the test results:
- slight leukocytosis;
- neutrophilia (manifests at an early stage of the disease);
- eosinophilia combined with lymphocytosis (occurs as enterovirus infection further progresses);
- extremely rarely, signs of hyperleukocytosis can be seen in the CBC.
Important! The detection of a specific enterovirus in a child’s blood is not always proof that it triggered the development of the disease. Often there is asymptomatic carriage of one or another strain of the virus. Proof that the disease is provoked by the identified pathogen is an increase in the level of immunoglobulins A and M by more than 4 times.
If there are symptoms characteristic of cardiac, neurological or other forms of EVI, the doctor prescribes additional instrumental and laboratory tests:
- electrocardiogram;
- magnetic resonance imaging;
- coagulogram (blood test for clotting);
- lumbar puncture;
- biochemical blood test for bilirubin, urea, creatinine and liver enzymes - ALT and AST;
- Ultrasound of the abdominal organs;
- CT;
- EchoCG;
- encephalography, etc.
The diagnostic scheme is developed purely individually, and depends on the symptoms that appeared in the child at the time of seeking help from a doctor.

Treatment of enterovirus infection in children
Specific treatment methods for EVI have not yet been developed. However, there are general principles for treatment at home for enterovirus infection in children. Basically, it is based on:
- Detoxification activities. The prescription of certain drugs depends on the form in which EVI occurs. Thus, sorbents (White or activated carbon), diuretics, and antiemetics may be prescribed. A prerequisite is to drink plenty of fluids. This is one of the main components of detoxification therapy.
- Symptomatic treatment. Headaches, myalgia, arthralgia, hyperthermia are the most common symptoms accompanying EVI in children. To relieve them, as a rule, NSAIDs are used - Ibuprofen, Ibufen, Nurofen, etc. It is possible to use oral non-narcotic analgesics - Paracetamol, Panadol, etc. For psycho-emotional overexcitation, it is possible to use sedatives of herbal origin.
- Antiviral treatment. For influenza-like forms of EVI, as well as for herpetic sore throat, antiviral drugs are prescribed. These may be Groprinosin, Laferobion, interferon preparations for oral or intranasal use.
Until the child recovers completely, it is necessary to provide him with plenty of fluids and a continuous flow of fresh air at home. During treatment, he should be isolated from his peers and not allowed into kindergarten or school.
In case of serous meningitis, myo- or pericarditis, the sick child should be immediately hospitalized. Further therapy will directly depend on the severity of the disease and the general condition of the baby.
Methods and rules of treatment
The doctor determines how to treat enterovirus infection in a child. Simple cases can be treated at home. Damage to the nervous system, fever (it is not possible to bring down the fever for a long time), problems with the heart, kidneys - indications for hospitalization of a small patient. There are no specific drugs for enterovirus infection; treatment is aimed at eliminating nonspecific symptoms; compliance with special rules speeds up the recovery process.
Doctors recommend adhering to the following rules:
- keep bed rest. Rest and sleep are the best “medicines” in the fight against illness;
- in most cases, the disease is accompanied by elevated body temperature. Children are given antipyretic drugs, it is allowed to use rectal suppositories (if there is no severe diarrhea), drugs in the form of a suspension. For such purposes, Paracetamol, Ibufen and others are used;
- restoration of water-salt balance is necessary to normalize the condition of a small patient. Diarrhea and frequent vomiting can lead to dehydration. Treatment for this situation consists of drinking plenty of fluids, using Regidron, and it is allowed to give the baby compotes and fruit drinks;
- to increase the baby’s immunity, interferons are prescribed (non-specific medications, they prevent the proliferation of pathogens and strengthen the child’s body’s defenses);
- Antibiotics are prescribed in cases where a bacterial infection occurs in a chronic form. The doctor chooses the specific drug; it is strictly forbidden to give the baby strong medications on your own;
- special diet. Includes an abundance of protein foods (lean meat), dairy products are allowed in small quantities. It is forbidden to give fresh fruits and vegetables to the baby; boiled vegetables and baked apples are suitable. It is strictly forbidden to feed your baby fried, smoked foods, soda, and sweets. The diet must be followed until complete recovery, preferably for a few more days after its onset;
- It is important to isolate the child from all family members during treatment. Provide your baby with separate bedding and dishes. When in contact with the baby, wear a gauze bandage, then wash your hands thoroughly and change clothes.
READ ALSO: Inflammatory process of the external genitalia - vulvitis in girls: causes of development, methods of treatment and prevention of infection
Prevention
There are no specific measures to prevent EVI. However, you can reduce the risk of developing the disease if:
- carefully and strictly observe the rules of hygiene;
- handle food well;
- avoid swimming in polluted waters;
- treat hands with antiseptics after working with soil or contacting a sick person;
- regularly carry out wet cleaning in the living area.
With timely initiation of treatment for EVI, the prognosis is favorable. This applies to almost all forms of the disease. But if therapy was started untimely or prescribed incorrectly, this can cause the development of serious complications:
- pneumonia;
- acute respiratory distress syndrome;
- cerebral edema;
- convulsive syndrome;
- hypovolemic shock;
- acute renal impairment;
- and others.
The presence of at least one of the above complications significantly worsens the prognosis of the disease. Therefore, at the first symptoms of EVI, even if they appear in a mild form, it is necessary to show the child to a pediatrician or family doctor!
Enterovirus infection - complications
The disease in question sometimes leads to serious and life-threatening consequences. Enterovirus in an infant can lead to serious disturbances in cardiac and respiratory activity. In isolated cases, this can even lead to death. Enterovirus infection is rarely complicated in older children - symptoms and treatment that are not determined in a timely manner can lead to:
- diabetes mellitus;
- orchitis;
- heart, liver failure;
- chronic pathologies of the respiratory tract;
- cerebral edema;
- mental disorders;
- epilepsy;
- pneumonia.