Epidemiology
The source of infection can only be an already sick person or a virus carrier. Humans are the only host of this virus in nature. The main route of transmission is airborne droplets. That is, during communication or if the virus carrier sneezes or coughs. Infection through the fecal-oral mechanism through the food, water, contact and household routes is also possible (for example, when using the same hygiene items with an infected child).
The peak incidence occurs in the summer-autumn period. Contagiousness (infectiousness) sharply declines, starting from 7–8 days from the moment of “meeting” with the pathogen. Herpangina is widespread everywhere. Children's groups are characterized by so-called outbreaks, but most often there are isolated cases of infection. Mostly children of primary school and preschool age are affected. Herpangina may occur both in isolated form and in combination with enteroviral serous meningitis, myelitis, epidemic myalgia, and encephalitis. Having recovered from the disease, the child acquires stable, long-term immunity.
Pathogenesis
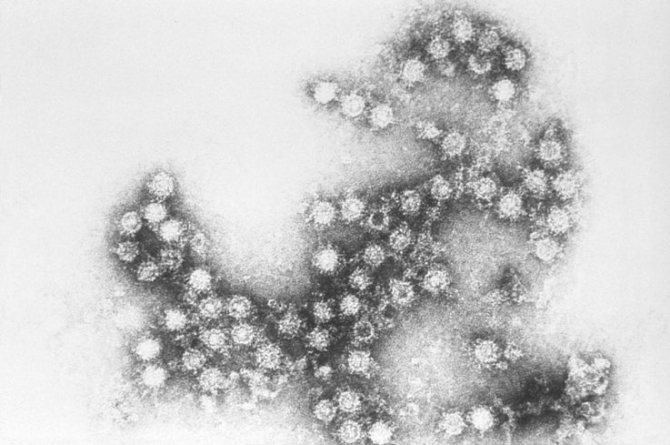
The causative agent is an RNA virus called Coxsackie. It belongs to the picornavirus family.
The virus was first isolated in 1948. It received its name in honor of the city of Coxsackie in the USA, where the children under examination were lying.
This virus has two groups: A and B. The group includes 19 serotypes (within the group there may be certain differences in immunological structure, such viruses are called serotypes). Tonsillopharyngitis can be caused by serotypes 2, 4, 5, 6, 10.
ECHO viruses were isolated in 1951 from the feces of healthy people.
The name is an abbreviation of the following words in English: Enteris Cytopathogenic Human Orphans (literal translation is: human intestinal cytopathogenic orphan viruses).
The virus enters the child’s body through the mucous membrane of the nasopharynx , replication (multiplication) of the virus occurs in epithelial cells and lymphatic structures, then, entering the blood, it “spreads” to different organs and systems. The most “preferred” for the virus is the mucous membrane of the oropharynx, the lesion of which is essentially herpangina. Unfortunately, damage to other organs is also possible - this is how a combined form of the disease occurs. There is evidence that the virus has tropism, that is, a direction of action in relation to muscle tissue and structures of the central nervous system.
Quite often, herpangina can occur against the background of an adenovirus infection or influenza.
Picture of the disease
The disease almost always begins acutely. The temperature suddenly rises to 38 or even 39 degrees (in rare cases, up to 40). But the general condition continues to be satisfactory. For older children, a rise in temperature to 39 degrees is unpleasant, but does not pose any particular danger, which cannot be said about children under one year old. In them, such a condition can cause seizures and other dangerous phenomena.
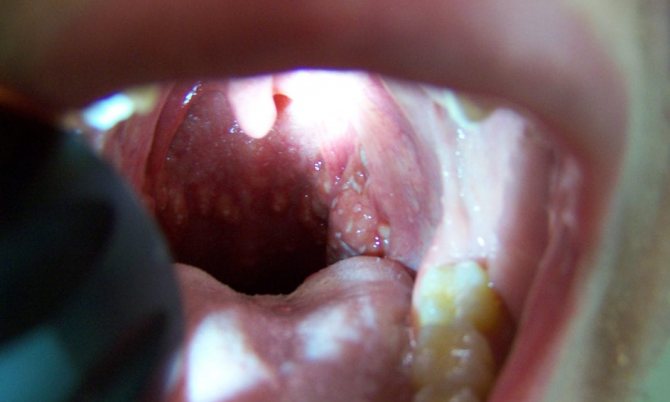
The temperature lasts from 2 to 5 days. In this case, a sore throat can be either mild or very strong. Single bubbles 1–2 millimeters in diameter appear on the mucous membrane of the tongue, palate, tonsils, and uvula. They grow quite quickly and reach 5 millimeters, then burst, and a painful ulcer forms in their place. If there are a lot of bubbles, they can merge, and then the ulcer can reach almost one centimeter in diameter.
If the disease is not accompanied by another infection, then after a week the ulcers heal on their own, and no trace remains of them, and a stable immunity to this type of enterovirus is formed in the body.
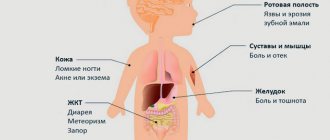
The main symptoms may be accompanied by additional ones:
- muscle pain, as if after intense physical exertion;
- lower back pain;
- heartache;
- abdominal pain, diarrhea;
- conjunctivitis;
- convulsions;
- rash on the torso.
The younger the patient, the more pronounced additional symptoms he has. In the most severe cases, sore throat in children can develop into meningitis.
Clinical picture

The incubation period ranges from 7 to 14 days. The first manifestations of the disease are the so-called flu-like syndrome : it manifests itself in the fact that the child feels general weakness, malaise, and decreased appetite. Herpangina is characterized by a very strong fever with a rise in temperature to 39 - 40 degrees. It is accompanied by pain in the back, abdomen, and muscles of the limbs; Vomiting, headache, and diarrhea are also possible. Then more specific symptoms appear, namely severe sore throat, pain during swallowing, coughing, nasal discharge, and drooling.
Vesicular pharyngitis develops in the throat of a child with herpangina; the following pathological changes are detected: severe hyperemia (redness) of the palatine arches, tonsils, tongue and palate, which is accompanied by the appearance of small papules (small nodules), then turning into vesicles (bubbles) with a diameter of up to 5 millimeters . No later than two days later, the vesicles open, and in their place whitish-gray ulcers measuring 1–6 millimeters in size with an area of redness around are formed. As a rule, the number of pathological elements is about 12 - 15. Sometimes these ulcers can merge with one another. Unfortunately, the resulting erosions are extremely painful, and children often refuse to eat food and water because of this.
Also, with herpangina, enlargement of the lymph nodes is possible: cervical, submandibular, parotid. They are painless upon palpation.
The fever “goes away,” as a rule, after 3–5 days, and defects on the mucous membrane heal within 6–7 days from the moment of appearance. If a child has a severe state of immunodeficiency or a large amount of virus in the blood, such dangerous manifestations of infection as meningitis, encephalitis, pyelonephritis, hemorrhagic conjunctivitis, and myocarditis may develop.
An atypical course of herpangina is also possible: in this case, there may be an unexpressed clinical picture similar to catarrhal changes in the oropharynx without the above-described blisters and ulcers. Sometimes a vesicular and papular rash appears on the distal parts of the upper and lower extremities and on the torso. In children with weak immunity, there may be a wave-like course, when fever, rashes and general signs of intoxication recur every 2 to 3 days.
Treatment of herpes sore throat in children
Treatment of the disease in children should be strictly under the supervision of a pediatrician. When confirming the diagnosis of herpes sore throat, parents should:
- give medications prescribed by a doctor;
- provide the child with plenty of fluids and bed rest (during the acute period of the disease);
- exclude from the diet sour, spicy, salty foods that irritate the mucous membrane of the oropharynx;
- increase the child’s immunity with the help of vitamin complexes and immunostimulating agents.
When treating herpes sore throat, the following is contraindicated:
- carry out warming procedures (apply compresses, rub the neck);
- perform inhalations;
- apply electrical procedures.
These treatments cause a local increase in temperature and improve blood supply to the throat. This process creates favorable conditions for the reproduction of the virus and contributes to its spread.

When treating herpes sore throat, inhalation is contraindicated.
Diagnostics
When diagnosing herpetic sore throat, the doctor looks at what the child’s oropharynx looks like, asks the parents about the symptoms, and prescribes a general blood test. If, upon examination of the pharynx, the presence of bubbles with serous contents is observed on the mucous membranes of the palate, tonsils, tongue and throat, and moderate leukocytosis is detected in the blood, then a positive diagnosis is made without additional laboratory tests.
If the clinical picture is atypical for herpes sore throat or blurred, then the doctor gives a referral for virological and serological tests.
To do this take:
- washings from the nasopharynx;
- throat swabs.
What else to read: Causes and treatment of herpes in the throat of a child
The most informative diagnosis is carried out using the immunofluorescence method. The development of the disease is confirmed if the test results show an increase in antibodies to enteroviruses. When collecting an anamnesis, the doctor differentiates herpes sore throat from serous meningitis, chickenpox, thrush, herpetic stomatitis, irritations of the oral mucosa caused by exposure to chemicals.

The most informative diagnosis is carried out using the immunofluorescence method. The development of the disease is confirmed if the test results show an increase in antibodies to enteroviruses.
Drug treatment
When treating a sore throat caused by the herpes virus, the pediatrician prescribes the antiviral drug Acyclovir. Its active substance penetrates the structure of the pathogenic microorganism and destroys it.
The dosage of the drug and the course of its administration depend on the age of the child, the characteristics of his development, and the severity of the disease.
If the cause of the development of the pathology is another pathogen (for example, the Coxsackie virus), Acyclovir is not used.
For herpes sore throat, symptomatic treatment is also carried out. To alleviate the baby's condition, oral administration is prescribed:
- drugs that have a hyposensitizing effect (Suprastin, Diazolin);
- antipyretic drugs (Efferalgan, Tylenol).

To alleviate the baby's condition, oral administration of Suprastin is prescribed, which has a hyposensitizing effect.
When carrying out local therapy, the oral cavity is treated with a solution of enzymes (Chymopsin, Trypsin), and then with an aerosol (Ingalipt, Hexoral).
If a bacterial infection is associated with herpes sore throat, then broad-spectrum antibiotics are used.
Folk remedies
Non-traditional methods of treating the disease are used in combination with drug therapy and only after agreement with the doctor. To combat herpes sore throat use:
- decoctions of medicinal herbs for gargling. They are made from sage, eucalyptus, calendula and chamomile;
- propolis, which is chewed every day for an unlimited amount of time (2 g);
- freshly squeezed beet juice diluted with 1 tsp. apple cider vinegar. Used to rinse the oropharynx. The procedure is repeated every 3 hours.
For children who are unable to gargle on their own, their parents wash their throats. For this, a syringe without a needle is used.

To combat herpes sore throat, use propolis, which is chewed every day for an unlimited amount of time (2 g).
Prevention
If a child is often sick, then the risk of developing herpes sore throat after exposure to the virus is high. Parents are recommended:
- exclude the possibility of the child coming into contact with an infected person;
- increase immunity by hardening and providing a balanced diet.
What else to read: Causes and treatment of herpes in the throat of a child
For infants, breast milk is used to prevent the disease. It contains antibodies that can resist the development of the disease.
Diagnostics

The diagnosis is usually made clinically. If a child has a picture of the typical course of herpetic sore throat, then it will not be difficult for a pediatrician or pediatric otolaryngologist to assume this pathology.
At the time of examination, the doctor notes the presence of characteristic rashes with typical localization on the surface of the tonsils, soft palate, posterior wall of the pharynx and the appearance described above (papules - “elevations” and vesicles - “bubbles”, which are then transformed into ulcers).
To identify the pathogen, it is possible to use a method such as PCR (nasopharyngeal mucus is taken as the test material), ELISA and RGPA are also used. With these methods, an increase in the titer of special antibodies is determined. The analysis is performed twice: on the 4th - 5th day from the onset of the disease and after the 14th. If an increase in antibody titer by more than 4 times is detected, then we can talk about the enteroviral etiology of the symptoms that have arisen in the child.

In a general blood test, the level of leukocytes may decrease, or less often, on the contrary, their level may increase. An increase in the level of lymphocytes is more specific for a viral infection, and a slight acceleration of ESR is possible. However, there are no highly specific changes in blood tests specifically for herpangina.
Changes in urine tests in the form of the appearance of protein (proteinuria), casts, and red blood cells are also unusual for herpangina. In this case we are talking about kidney damage.
To exclude the presence of serous meningitis in a child, consultation with a neurologist is recommended.
Symptoms
The incubation period (the time from the virus entering the body to the appearance of the first signs of the disease) of herpes sore throat averages from seven to fourteen days.
The first symptoms of herpetic sore throat are similar to those of the flu: weakness, poor health, loss of appetite. Body temperature can rise to thirty-nine to forty degrees. The child complains of pain in the head, muscles, back and abdomen. Nausea, vomiting, and stool disturbances occur. These unpleasant symptoms include a sore throat, cough, runny nose, and production of large amounts of saliva.
In childhood, the disease is characterized by a rapid increase in local symptoms.
On the first day, redness of the mucous membrane of the palate, tonsils, and uvula is observed. Small bubbles (papules) form on their surface. After some time, they transform into vesicles (vesicles approximately five millimeters in size filled with serous fluid).
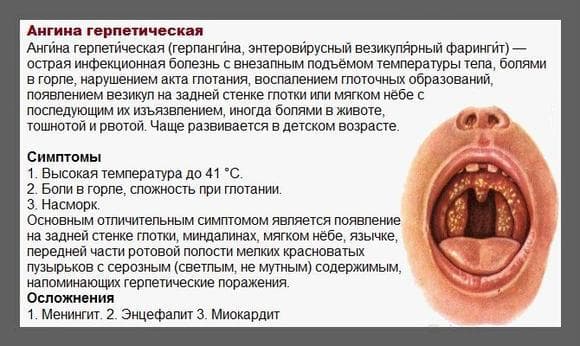
After about two days, the blisters burst, and in their place remain white-gray ulcers with redness around them. If the ulcers are connected to each other, then the formation of erosions occurs. Erosion causes pain to the child, so he refuses to eat and drink.
With herpetic sore throat, there is an increase in lymph nodes in the ears, neck and lower jaw.
At the same time, along with typical symptoms, erased signs of herpetic sore throat also appear. They manifest themselves only in catarrhal changes in the oropharynx. If a child has a weakened immune system, herpes rashes may occur every two to three days. At the same time, they will be accompanied by a feverish state and intoxication of the body. Less commonly, with herpes sore throat, a papular rash appears on the hands and feet, and on the body.
Typically, the symptoms of the disease begin to subside on the third to fifth day. And on the sixth or seventh day the mucous membrane begins to heal.
Differential diagnosis
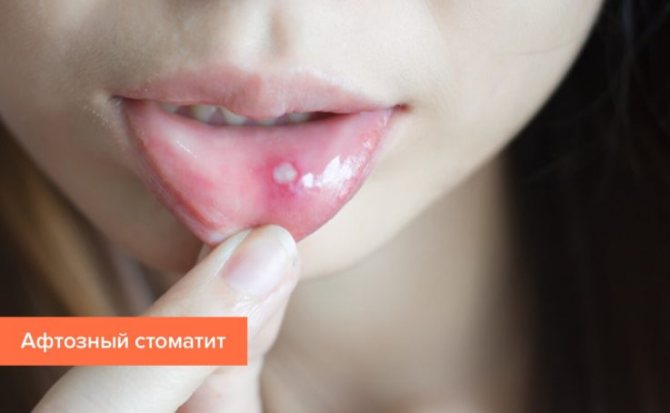
Due to the similarity of the clinical picture, the doctor will likely make a differential diagnosis with acute herpetic stomatitis. With this disease, the localization of the rash is different: the mucous membrane of the mouth, lips, skin. It is also characteristic that the rashes are repeatedly “repeated”, and with each appearance the temperature drops to low-grade levels (no more than 37.5 degrees).
With chickenpox, rashes can be seen on almost any part of the body; rashes and the so-called false polymorphism of the rash are characteristic, when, due to constant rashes, different morphological elements are visualized on the skin. It is also necessary to distinguish herpangina from chemical damage to the mucous membrane, from thrush, and aphthous stomatitis.
Herpes sore throat in children - symptoms
When herpes appears in a child’s throat, the symptoms of the disease resemble a sore throat. This greatly complicates the diagnosis of pathology. The disease begins with a sharp rise in temperature to 38–39 degrees. Almost simultaneously, the child complains of sore throat and sore throat. Young children become restless: they act up, cry, and hold their fingers in their mouths.
A characteristic symptom of the disease is rashes on the tonsils - vesicles. These are small bubbles with liquid inside - pus, sometimes blood. The rashes are located in groups. When spontaneously opening, the child feels severe pain. As the outbreak spreads and the number of rashes increases, it becomes painful for children to swallow, so they completely refuse to eat. Other symptoms of herpes in the throat include:
- swelling and hyperemia of the throat mucosa;
- headache;
- increased salivation;
- burning and itching in the throat;
- enlargement of the submandibular lymph nodes.
The difference between herpes sore throat and purulent
In order to correctly identify the disease and consult a doctor in time, every mother should clearly understand what herpes looks like in a child’s throat and how it differs from a purulent sore throat. The rashes in these diseases are similar, but with herpes the localization of the rash differs from sore throat. Herpes rash elements are always concentrated at the entrance to the throat and completely cover the tonsils. What does herpes look like in a child’s throat – a photo of the rash is located below.

With purulent sore throat, the rash spreads not only to the tonsils, but also affects the larynx. These changes lead to voice impairment and provoke coughing due to severe swelling, which practically does not occur with herpes. In practice, to make a final diagnosis, laboratory research methods are prescribed:
- general blood analysis;
- laboratory saliva analysis;
- scrapings from the oral mucosa;
- PCR;
- ELISA.
Temperature in children with herpes in the throat
Herpes sore throat without fever is practically never found in a child. The body always reacts violently to the introduction of a pathogen. When waste products of the virus enter the blood, intoxication occurs, which causes a rise in temperature - a natural reaction of the body. However, with other localization of herpes (in the groin, in the lip area), an increase in temperature may not occur. This is rare in children. A characteristic feature is that the temperature rises only during a rash. After their appearance, normalization of the indicator is observed.
What medications are used?

- with severe hyperthermia over 38.5 degrees, non-steroidal anti-inflammatory drugs (NSAIDs) are needed. For children, medications containing paracetamol (paracetamol in suspension, Efferalgan, Cefekon suppositories) and ibuprofen (Nurofen, ibuprofen in suspension and other drugs) are used. Paracetamol is used in a dose of 10 - 15 mg/kg/dose, not more than 60 kg/day. Ibuprofen, usually 10 mg/kg;
- for muscle pain, analgesics can be used, but the above NSAIDs have analgesic properties.
Metamizole sodium (aka Analgin) and all medications containing it are prohibited for use in children;
- antihistamines. In order to reduce the manifestation of inflammatory changes, it is possible to use these drugs. They also potentiate, that is, enhance the effect of antipyretics and analgesics. Of the first-generation drugs, chloropyramine (Suprastin, Supramin, Subrestin) is often used (allowed in children over 1 month), clemastine (Tavegil) in children over 6 years old and, of course, Fenistil drops, allowed from 1 month (Fenistil in capsules is allowed only from 12 years of age). Among the second generation drugs, the most familiar to all fathers and mothers are Zyrtec and Zodak (cetirizine; used from 6 months), loratadine - from 2 years (Claritin, Clarisan, Claridol, Lovanik and others), of the third generation antihistamines - desloratadine - from 1 years (Erius, Dezal, Telfast), levocytorizine - from 2 years (Xyzal, Suprastinex, Zodak-Express). When using these medications, the most pronounced side effect is sedation, that is, drowsiness. However, with modern drugs this manifestation is minimally expressed.
It is necessary to strictly and correctly observe the dosage and frequency of administration. Each drug has its own.
Local therapy for herpangina
Irrigation of the oral cavity with antiseptic solutions, which include Furacilin, Miramistin, and chlorhexidine solution, is of utmost importance for alleviating the child’s condition and preventing the development of secondary infectious complications.

You should not torture your child with Lugol's solution. The pain from its use far outweighs the beneficial effect.
What drugs and treatment methods should not be used to treat herpangina?
- Antibiotics are absolutely not needed, since herpangina is a disease of viral etiology. Antibiotics are added only when a secondary infection occurs, which, fortunately, happens quite rarely;
- Treatment with herpes medications (vanciclovir, acyclovir) is also unjustified. Despite the “herp” in the name, herpangina is not related to the herpes virus; the cause of the disease is the Coxsackie and ESNO enteroviruses.
Antiherpetic drugs are completely useless;
- various antiviral agents and immunomodulators (Imudon, Immunal, Anaferon, Arbidol, Tsitovir-3 and others), which our pharmacies are currently overflowing with, are drugs without an appropriate evidence base. Their use is inappropriate, and long-term consequences have not been studied;
- inhalations and warming the throat are also completely pointless. An increase in local temperature does not contribute to the elimination of the virus, while steam from inhalation, on the contrary, contributes to the spread of the infectious process in the body.
Diet and regimen during treatment
The child should be dressed comfortably; the baby should not be overly warmed. Normal room temperature (19 - 21 degrees) and normal air humidity are required.

As for diet, at the first stages of illness, dishes should be of a soft consistency so as not to further injure the damaged oral mucosa. A good diet would be Pevzner, which includes porridge (oatmeal, rice, semolina), soups, broths, soft bread, boiled or baked vegetables, dietary meat, and low-fat dairy products. More details about the diet can be found on the relevant resources.
Treatment of herpetic sore throat in children does not differ from that in adults.
Treatment of herpetic sore throat in children
The treatment process for herpetic sore throat in children is symptomatic. You can only help your baby by reducing pain or body temperature. Otherwise, you need to strengthen the state of his immune system. In severe form, with a weakened immune system, even hospitalization of the child is possible. Therefore, you need to be careful and monitor the health status and development of symptoms in your baby.
Tablets, medications for the treatment of herpes sore throat:
- Antihistamines, which will reduce swelling in the tissue of the larynx;
- Antiseptic solutions to prevent secondary microflora from joining the inflamed tissue;
- The same drugs have anti-inflammatory and antipyretic properties: Nimesulide, Ibuprofen. You can reduce the temperature with Paracetamol, but this should only be done if it rises to a level above 38 degrees. Before this, the body must fight the infection itself, in addition, there is a risk of reducing it to a critical level, which will lead to complications;
- Gargles can be given to a child using folk remedies: a decoction of medicinal herbs (chamomile, calendula, oak bark, sage), low-concentrated solutions of kitchen salt, Furacilin, Fukortsin or potassium permanganate;
- There is no need to use Acyclovir. This simply does not make sense, because the disease, despite the name, is not caused by the herpes virus. This drug does not work against the virus during the incubation period of Coxsackie;
A very important part of treatment is to drink plenty of fluids. You need to give your child as much water, tea, compote, juices as possible.
- To increase the resistance of the immune system, interferon preparations, vitamin complexes, balanced nutrition and a healthy daily routine are used.

In order to prescribe appropriate treatment, specific tests must be performed. The immunofluorescence method will help determine the presence of antibodies to a specific pathogen. This will ensure that your child is not harmed by being prescribed unnecessary medications, such as antibiotics, that can be harmful to their health. You need to know how the disease progresses in order to be prepared for possible complications and know what to do.
In newborns and infants, the disease develops extremely rarely, since their body protects the immunity inherited from the mother.
In addition, there is an opinion that breast milk also contains antibodies, which help fight pathogens. In children under 3 years of age, herpangina is often complicated and can cause serious consequences. This is the most vulnerable group of patients.