MULTIPLE PREGNANCY
- pregnancy that occurs with the simultaneous development of two or more fetuses.
M. b. observed in 0.4-1.6% of all pregnancies; In this case, twins occur most often.
Causes of M. b. insufficiently studied. Heredity has a certain significance; Families are known in which twins and even triplets will be born from generation to generation (more often with repeated pregnancies). M. b. can occur either as a result of fertilization of two or more eggs (fraternal twins develop), or when embryos develop from one fertilized egg (identical twins develop).
Features of the structure of the fertilized egg
Rice.
1. Schematic representation of biamniotic fetuses: each fetus has separate amnion and chorionic membranes; on the left - each fetus has its own decidua (indicated by arrows); on the right - the decidua is common to both fetuses (indicated by an arrow). Rice. 2. Schematic representation of the placenta with fraternal twins: the septum between the two amniotic cavities consists of four membranes - two amnions (1) and two chorions (2). With M. b. each fertilized egg, after penetration into the decidua (see), forms its own amnion and chorionic membranes (see. Membrane), from which each fetus develops its own placenta (see) with an independent network of vessels; the capsular decidua can be common to all fetuses or separate to each (Fig. 1). Identical twins can be biamniotic - the embryos form separate amnions and they remain separate, or monoamniotic, i.e. a common amniotic cavity is formed for both embryos; Identical twins share a common chorionic plate (monochorionic twins). Whether the twins were fraternal or identical is judged by the results of examination of the placenta: fraternal twins are characterized by the presence of separate or touching placentas, the septum between the fetal sacs consists of 4 leaves; Identical twins are characterized by a common placenta, the septum consists of 2 leaves (Fig. 2).
Problems with the development of the fertilized egg
During the period of nidation (introduction of the fertilized egg with the help of chorionic villi into the uterine mucosa), a number of problems may arise. Due to the fact that successful implantation of the fertilized egg depends on the speed of its movement along the fallopian tube, if the membrane of the fertilized egg moves too quickly, it may not have time to fully form, which prevents the egg from attaching to the uterine wall and leads to termination of pregnancy (miscarriage of the fertilized egg ).
Cases of low attachment of the fertilized egg, which may indicate a cervical (ectopic) pregnancy, also require constant monitoring. In this situation, surgical intervention is performed, since the development of this type of pregnancy poses a threat to the woman’s health, including removal of the uterus.
If pregnancy is terminated, you need to carefully ensure that the egg comes out completely. The remains of the fertilized egg are removed by scraping the walls of the uterine cavity. In cases where the cause of the miscarriage remains unknown, a histological analysis of the fetal egg is performed.
Remnants of the fertilized egg remaining in the uterine cavity after a miscarriage can lead to the development of an infectious process, the treatment of which will require antibacterial therapy.
Another complication that can result from the remaining fertilized egg is bleeding.
A “false egg” that appears during an ectopic pregnancy and differs on ultrasound in the shape and width of the walls is an accumulation of blood or glandular secretion of the fallopian tube.
One of the serious developmental pathologies is an empty ovum, which appears due to a number of reasons: the age of the mother, the presence of genetic disorders, taking medications that are contraindicated during pregnancy. It must be taken into account that at 1-2 weeks of pregnancy, an empty ovum is the norm (the fetus at this stage is simply visually indistinguishable), while the presence of this pathology at a later stage leads to a medical termination of pregnancy.
The course of pregnancy and features of fetal development
M. b. may proceed normally, but is often complicated. Spontaneous abortions (see), premature birth (see), toxicoses (see Toxicoses of pregnant women) are often observed. With M. b. Even with an uncomplicated course, a woman may feel tired, shortness of breath, frequent urination, and constipation appear due to a significant increase in the size of the uterus. These phenomena intensify with polyhydramnios (see), tachycardia and other symptoms characteristic of it appear.
The development of fruits, as a rule, is more or less uniform, the difference in weight is small. Sometimes there is a pronounced unevenness of their development, associated with the presence of anastomoses between the vessels of the fetal placentas; with different intensity of cardiac activity of the fetuses, the blood supply of one of them is much better, as a result of which the second fetus lags behind in development and may even die (see Antenatal pathology). This, in all likelihood, is the mechanism of a rare form of underdevelopment of one fetus from twins - the so-called. paper fetus (a shapeless formation found in the membranes of the born placenta). With identical, monoamniotic twins, incomplete splitting of the embryonic rudiment is possible, resulting in developmental defects (see) in the form of conjoined twins. Fusion of fruits occurs in the head region (craniopagus), pelvic region (pygopagus, ischiopagus), and trunk region (thoracopagus, stereopagus, etc.).
Rice. 3. Schematic representation of the most common location of fetuses in the uterus during multiple pregnancies: longitudinal position and cephalic presentation of twins.
The location of the fetuses in the uterus with M. b. may be different: most often both fetuses are in a longitudinal position and cephalic presentation (Fig. 3). Other options are possible: one fetus is in a cephalic presentation, the other in a pelvic presentation: both fetuses are in a breech presentation; one fetus is in a cephalic presentation, the second is in a transverse position; breech presentation of one fetus and transverse position of the other; both in a transverse position.
Diagnosis in early pregnancy is difficult. It is based on dynamic observation; with an increase in the size of the uterus that does not correspond to the gestational age, it is necessary to carry out a differential diagnosis with polyhydramnios (see), hydatidiform mole (see), uterine fibroids (see). In such a situation, the diagnosis is established using ultrasound (see Ultrasound diagnostics), which makes it possible to determine M. b. at the earliest possible date (from 2.5 weeks). After 10 weeks pregnancy, fetal cardiac complexes can be recorded using electrocardiography (see Fetus). At the end of pregnancy, an increase in abdominal circumference that does not correspond to the gestational age with one fetus, a feeling of fetal movements and palpation of its small parts in different parts of the abdomen, identification of a saddle-shaped uterus, grooves between fetuses, identification of three or more large parts of the fetus, the presence of different places of the uterus at two points of distinct heart tones with a difference in frequency of 10 heart beats per minute or more, and the so-called. zones of silence between them. X-ray to identify M. b. used extremely rarely and only when indicated at the end of pregnancy.
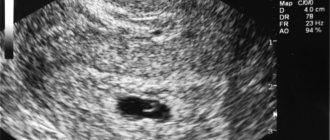
Twin pregnancy: early ultrasound
At the first examination at 4-6 weeks, the gynecologist will not be able to determine the number of fetuses. This is visible on ultrasound only from the 8th obstetric week of pregnancy (provided the doctor has a good device). Until this date, it is impossible to say for sure whether you have a multiple pregnancy or not.
Ultrasound of twins 8 weeks
Photo of ultrasound of twins in early pregnancy, 8 weeks
At 8 obstetric weeks (or 6 weeks from the moment of conception), transvaginal ultrasound is usually used. The device is inserted inside to better see the embryos. Two or three dark spots are visible on the monitor. The doctor measures the length of the embryos and records several heartbeats.
Ultrasound of twins 12 weeks
Early pregnancy photo of twins, 12 weeks
Ultrasound multiple pregnancy, quadruplets, 12-13 weeks
At 12 - 14 weeks, all pregnant women undergo the first screening. Women expecting twins or triplets are sent for research as early as possible. At 10-11 obstetric weeks.
Ultrasound is performed as a screening method. That is, the device is moved over the abdomen so as not to damage the embryos. At this stage, the number of placentas and fetal bladders is already visible.
At 10-12 weeks, the doctor can determine the type of pregnancy:
Dichorionic - diamniotic (di-di) - each fetus is in its own sac (amnion), each has its own separate placenta.
Monochorionic - diamniotic (mono-di) - children have one placenta for all. But they are separated from each other, since each embryo has its own amniotic sac.
Monochorionic - monoamniotic (mono-mono) - one placenta and one amniotic sac for all. Children are not separated from each other.
Childbirth
Childbirth with M. b. usually occur through the natural birth canal and more often proceed normally: after dilatation of the cervix, first one fetus is born, then the next one is expelled. However, complications are not uncommon: untimely rupture of amniotic fluid and loss of small parts of the first fetus, weakness of labor forces due to overdistension of the uterus, fetal hypoxia (see Asphyxia of the fetus and newborn), premature placental abruption of the second fetus after the birth of the first (see Premature placental abruption), delayed rupture of the membranes of the second fetus, hypotonic bleeding in the placenta and early postpartum periods (see Hypotonic bleeding).
To regulate the contractile activity of the uterus and relieve pain during labor during M. b. use electroanalgesia (see Electroanesthesia), antispasmodics (see), and prevent fetal hypoxia. The amniotic sac of the first fetus is opened carefully and amniotic fluid is slowly released; The period of exile is expectant. If complications occur on the part of the mother or fetus, the period of expulsion of the first fetus is accelerated by surgical methods - the application of a vacuum extractor (see Vacuum extraction), obstetric forceps (see), extraction of the fetus by the pelvic end (see Breech presentation of the fetus). After the birth of the first fetus, the fetal and maternal ends of the umbilical cord are carefully tied, since in case of identical twins, the second fetus may die from blood loss through the vessels of the umbilical cord of the first fetus if its umbilical cord is not tied.
After the birth of the first fetus, the position, presenting part and condition of the second fetus are determined. If the mother and fetus are in good condition and its longitudinal position, the birth is expectant. After 10-20 minutes. after the birth of the first fetus, when uterine tone appears and contractions resume, the amniotic sac of the second fetus is opened (amniotic fluid is released slowly) and labor is allowed to proceed naturally. When the second fetus is in a transverse position, a pedunculated rotation is performed (see Obstetric rotation). Turning the fetus onto its leg and immediately removing it is also carried out if fetal hypoxia occurs or bleeding from the birth canal occurs when the fetal head is located above the entrance to the pelvis; if the fetal head is in the pelvic cavity, the birth is completed by applying obstetric forceps. When the fetus is breech, it is removed by the leg or inguinal fold. With conjoined twins, sometimes childbirth occurs spontaneously (fusion of the heads and buttocks with a small size of the fetus), sometimes childbirth is impossible and it is necessary to resort to fetal-destroying surgery. If the heads of two fetuses enter the pelvis at the same time, or if the first fetus is breech and the second is cephalic, delivery is possible only by decapitation of the first fetus (see Decapitation).
The afterbirth period requires special attention. Immediately after cutting into the presenting part of the second fetus, in order to prevent hypotonic bleeding, the woman in labor is given an intravenous drip of 1 ml of methylergometrine or oxytocin with 500 ml of isotonic sodium chloride solution. If bleeding occurs, measures are immediately taken to remove the placenta from the uterus (see Sediment period). The placenta that is born is carefully examined to ensure its integrity and to establish the identical or dizygotic origin of the twins. Fraternal twins can be same-sex or opposite-sex, have the same or different blood type; Outwardly, as a rule, they are not similar to each other. Identical twins are always the same sex and look very similar to each other; They have the same blood type.
In the first hours after birth, the condition of the postpartum woman, the tone of her uterus and the amount of blood discharge from the genital tract are carefully monitored.
Forecast
With M. b. the prognosis for the mother and especially for the fetus may be unfavorable. For the mother, the prognosis is determined by the severity of toxicosis, the prolonged course of labor, the possibility of developing hypotonic bleeding, and postpartum diseases of a septic nature (see Postpartum diseases).
Fruits with M. b. often die due to premature birth; Surgical intervention during childbirth in women with multiple births sometimes adversely affects the health of the newborn.
Prevention of complications.
Pregnant women with multiple births require careful monitoring in an antenatal clinic. In case of complicated pregnancy (toxicosis, threat of miscarriage, etc.), urgent hospitalization is necessary in the department of pathology of pregnant women for appropriate treatment.
See also Pregnancy, Childbirth.
Bibliography:
Breunung M. Analysis of the causes of premature birth, multiple births and stillbirths, Vopr. ocher mat. and children, vol. 15, no. 12, p. 40, 1970, bibliogr.; Genetic and statistical analysis of multiple births in humans, Genetics, v. 12, no. 9, p. 118, 1976, bibliogr.; Demidov V.N. and F e d e r 3. M. Features of hemodynamics during multiple pregnancy, Issues, protection. mat. and children, vol. 21, no. 11, p. 67, 1976; Kapralova R. S. Diagnosis of multiple pregnancy, Obstetrics and Gynecology, No. 8, p. 62, 1977; S y r o v a t k o F. A. et al. Auxiliary methods for diagnosing multiple pregnancy, ibid., No. 4, p. 66, 1969.
I. V. Ilyin.