The stomach hurts at the 19th week of pregnancy due to changes in the mother’s body, obstetric and non-obstetric pathologies. During the period of bearing a child, inflammatory processes and chronic diseases diagnosed before conception may worsen.
How long have you had this pain syndrome?
- Several days (26%, 782)
- First day (21%, 634 Votes)
- Several months (13%, 382)
- Week (10%, 309)
- Several weeks (10%, 301)
- About a month (8%, 250)
- Chronic form (7%, 205)
- About a year (6%, 181)
Total voters: 3 045
Loading …
Use search Are you having a problem? Enter “Symptom” or “Name of the disease” into the form, press Enter and you will find out all the treatment for this problem or disease.
Why does my stomach hurt at 19 weeks of pregnancy?
Week 19 is the fifth obstetric month.
Changes in the mother's body continue. The uterus continues to grow. The skin stretches. The muscles of the abdominal wall are in constant tension. There is a heavy load on the ligaments. Increased weight has a bad effect on the functioning of the musculoskeletal system. These changes cause pain. It is considered a non-dangerous obstetric pain, that is, it is associated with the characteristics of bearing a child.
You can relieve suffering by resting and taking a comfortable position. Such sensations differ from pathological and dangerous obstetric sensations in the absence of additional characteristic symptoms.
There are a number of dangerous conditions that are accompanied by unpleasant sensations. The woman feels the lower abdomen begin to tighten, discharge mixed with blood appears, the temperature rises, and severe vomiting begins.
Causes of these symptoms:
- Premature birth.
- Placental abruption.
- Increased uterine tone.
For these pathologies, an ambulance is called and hospitalization is performed.
Painful sensations are typical for non-obstetric pathologies that occur in any person and are not associated with pregnancy:
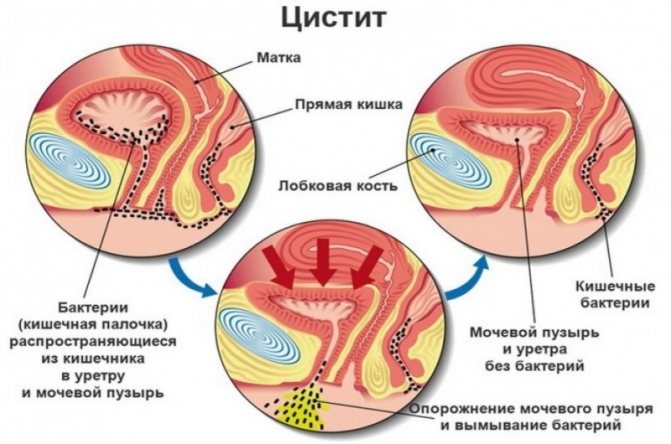
- cystitis is a dangerous inflammation of the bladder;
- pancreatitis is an inflammatory process affecting the tissue of the pancreas;
- cholecystitis - inflammation of the gallbladder;
- acute appendicitis;
- increased gas formation in the intestines;
- oncological diseases.
Treatment is carried out under medical supervision. Non-steroidal anti-inflammatory drugs are prescribed for inflammation. In some cases, surgery is performed to save the life of the mother and child. Pharmaceutical therapy is used for recovery and prevention.
For diagnosis the following is prescribed:
- Blood test (biochemical, erythrocyte sedimentation rate - shows inflammation).
- Ultrasound examination of the pelvic organs.
- Examination at an appointment with an obstetrician-gynecologist.
Lack of attention to existing health problems will lead to disastrous consequences. You need to monitor your own activity. Avoid high loads and overvoltage. Maintain a sleep and rest schedule. Consume permitted foods. Avoid bad habits.
Problems
The risks of the first trimester are far behind us, but some complications can still arise. Painful sensations in the pelvic area are common companions for women. If the pain intensifies or is accompanied by heavy discharge, it is better to play it safe and consult a doctor.
Stomach ache
They can occur for various reasons. Moderate spasms accompany the enlargement and stretching of the uterus. This is a normal option if bloody discharge does not appear against the background of pain.
Abdominal pain may accompany constipation and bloating. If it subsides after the gas passes, there is no reason to worry. Although it’s still worth reconsidering your diet.
If the pain is severe, spastic, it intensifies, is accompanied by bloody discharge and nausea and vomiting, you need to consult a doctor. If there is discharge, there is a risk of miscarriage. Nausea and vomiting may indicate appendicitis.
Lower back pain
She quite often accompanies pregnant women. The main reason is a shift in the center of gravity and an increase in the load on the lower parts of the spine.
There are several ways to prevent their occurrence:
- Do not stay in one position for more than 30-40 minutes.
- Walk or do gymnastics more often.
- If you spend the evening listening to TV or a book, it is better to lie on your side than to sit for more than 20-30 minutes.
- If there are no contraindications, you can go to the pool - this will help relieve the stress on the spine and improve overall well-being.
Bleeding
They occur quite rarely. The main causes are abdominal injuries and falls. Also, if sex is too aggressive, a small vessel may rupture, which leads to bleeding. If they are not accompanied by pain, it is enough to simply avoid unnecessary stress for a day or two and rest more.
If the bleeding is heavy (even if it is not accompanied by pain), it is better to consult a doctor to find out its exact cause.
Temperature
An increase in temperature usually indicates an infectious or inflammatory process.
Among the most common reasons:
- ARVI and other respiratory diseases;
- intestinal infections and food poisoning;
- diseases of the urinary and reproductive system.
If the temperature is below 38, the general condition is satisfactory - no need to worry. If the temperature is high, the woman is bothered by pain, nausea and other unpleasant symptoms - contacting a doctor should not be put on hold.
Toxicosis
In a normal pregnancy, by the 19th week a woman forgets about toxicosis. If it persists or returns after a short break, this indicates some complications. In this case, additional diagnostics are required.
Prolonged toxicosis may indicate a Rh conflict between mother and child, as well as non-preeclampsia.
Among other reasons:
- Poor nutrition, an abundance of fatty and spicy foods, food allergies.
- Arterial hypertension.
- Intestinal infection.
Nausea
Usually indicates a disease of the digestive system (acute inflammation or exacerbation of a chronic process) or intoxication. Mild nausea can occur when overeating or eating fatty foods.
If nausea is accompanied by pain, fever, vomiting and other symptoms, additional examination is necessary.
Cold
ARVI is less dangerous than in the first trimester. But this does not mean that a woman should let everything take its course. You shouldn’t buy up all the medications for colds: if there are no complications, the body will recover on its own if you follow a rest regime and drink enough fluids.
If complications do appear, you need to consult a doctor. He will prescribe medications that are safe during this period. For a severe cough, you can use drugs based on bromhexine and guaifenesin, you can use some vasoconstrictor nasal drops - but subject to strict adherence to the dosage.
The expectant mother's immunity becomes more durable during this period. But you should still take care of your health and, if possible, avoid going to crowded places during epidemics.
Antibiotics
If the infection is more dangerous than treatment, the pregnant woman can use some antibiotics to treat cystitis, sexually transmitted infections, bronchitis and pneumonia. Antibiotics of the penicillin group, cephalosporins, as well as some antifungal drugs (Clotrimazole, Natamycin, Nystatin - but only for local treatment) are allowed. All treatment is mandatory only after prescription by a doctor.
Alcohol
Throughout pregnancy, doctors do not recommend drinking alcohol. Some studies show that a small amount of weak alcohol (quality beer or wine) will not cause much harm. But it’s not worth the risk, because alcohol, even in small quantities, can provoke vasospasm.
Many people feel an increased craving for alcohol, even if they practically did not drink alcohol before pregnancy. This does not mean alcohol addiction at all. Most often, this condition occurs due to a lack of protein in the body.
You need to reconsider your diet, include more lean meat, fish, and eggs. If you really want to, you can take 1-2 sips of alcohol - but only at your own risk and if there is no threat of miscarriage.
Miscarriage
Spontaneous interruption in the current period is quite rare. Often the cause is a genetic abnormality. A miscarriage due to a genetic failure occurs before the 12th week, but if not all measures were taken to maintain the pregnancy in the first trimester, the consequences may appear at 19-22 weeks.
The risk of miscarriage at this stage increases:
- Bad habits (alcohol, smoking, taking drugs).
- Hormonal disorders (high levels of male sex hormones).
- Infections, especially sexually transmitted ones.
- Constant stress.
- Excessive exercise, heavy lifting, running and jumping.
- The use of certain medications and traditional medicines that are prohibited during pregnancy.
Possible dangers and complications
Complications at this stage are associated with minor risks. For example, if there is a lack of vitamin D, the fetus may develop rickets. Calcium deficiency is the cause of tooth decay in pregnant women, hemorrhoids and varicose veins. Being overweight in a woman can lead to preeclampsia and diabetes.
Under the influence of hormones, a woman can become distracted and inattentive. From the digestive system, heartburn, belching and increased gas formation often occur.
What causes nagging, aching pain during pregnancy?
Pain syndrome is provoked by obstetric factors:
- volume of the uterus;
- woman's body weight;
- condition of the musculoskeletal system;
- ligament extensibility;
- tone and elasticity of the abdominal muscles.
Discomfort due to illness:
- Inflammatory processes.
- Seasonal colds.
- Oncology of benign and malignant properties.
Self-medication is a rash decision.
To create a treatment plan you need:
- consult a doctor;
- undergo diagnostics.
Zootherapy for pain management
The practice of interacting with animals has been used in psychotherapy for quite a long time. As a result of exercise within 15 minutes, stress disappears, the rhythm of the heartbeat normalizes, and blood pressure normalizes. The effect is achieved due to the patient receiving positive emotions.
During pregnancy, it is allowed to use zootherapy in the absence of allergic reactions to animal fur. Communication practices that can be used:
- Dogs.
- Cats.
- Horses.
- Dolphins.
- Aquarium fish.
Zootherapy can reduce discomfort from non-dangerous obstetric pain.
What does dull, pulling, point or cutting pain in the abdomen indicate?
Stomach pain during pregnancy is due to changes in the body, in organs associated with hormonal changes, changes in the position of internal organs, and obstetric pathologies.
Many types of these sensations do not pose a threat to the health of the mother or the condition of the fetus. Others cause significant harm and even death to the woman and the unborn child.
Pain is a reaction of the nervous system to stimuli. A symptom of many diseases, including obstetric pathologies during pregnancy. A pregnant woman experiences hormonal changes and a restructuring of many systems. They are also accompanied by this feeling.
If discomfort and pain occur, it is better to consult with your doctor about the nature of these sensations and appropriate treatment. During pregnancy, a woman is responsible not only for her own health, but also for the health of the baby.
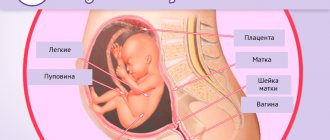
Nature has determined that the mother’s body tries to protect the fetus from all negative influences. A plug formed from mucus in the cervix prevents pathogenic microorganisms from entering.
Umbilical cord nutrition is formed in such a way that harmful chemical compounds do not enter the fetus. The uterus itself protects the child from external mechanical influence.
At the same time, during the period of bearing a baby, the woman herself may regularly experience pain of varying intensity and nature. Each type of discomfort indicates the presence of different pathological conditions, with the exception of harmless obstetric ones associated with changes in the maternal body and preparation for childbirth.
Based on the nature, intensity of pain, and gestational age, we can talk about how dangerous the condition is.
For example, pulling, extending to the lower back and groin, may indicate a risk of miscarriage. An additional sign of the condition will be the presence of bloody discharge.
In this case, you should immediately seek medical help and undergo an examination. If you delay visiting a doctor, the frequency of contractions will become more frequent and spontaneous miscarriage will occur.
Uterine tone is dangerous regardless of how early it was diagnosed. The fetus may experience a lack of oxygen and incoming nutrients. The woman feels a sharp pain like contractions. The solid state of the uterus and lower abdomen is recorded.
In case of injury, late toxicosis, or stress, placental abruption may occur. The condition is accompanied by acute pain in the lower abdomen. Often there is internal bleeding without external manifestations in the form of discharge. Urgent hospitalization and surgical intervention are required. Without help, death will occur.
Cramps accompanied by dizziness at five to twelve weeks can be a symptom of an ectopic pregnancy. For a number of reasons, the egg was unable to enter the uterus and became embedded in the fallopian tube.
As a result of the rapid growth rate of the fertilized egg, severe pain occurs. The woman is sent for an ultrasound examination. An operation to terminate the pregnancy is prescribed. Lack of medical care will result in death for the pregnant woman.
A number of non-gynecological problems also contribute to the occurrence of unpleasant sensations in the lower abdomen:
- Disruption of the gastrointestinal tract. Additional symptoms: bitterness in the mouth, tingling in the lower abdomen, heartburn.
- Inflammation of the bladder and urinary tract. Symptoms: discomfort and burning when urinating, increased frequency of the urge to urinate, increased body temperature.
- Seasonal colds. They are accompanied by headaches, nasopharyngeal congestion, aching bones, and fever.
- Inflammation of the appendix (appendicitis). An acute condition in which severe vomiting occurs, weakness, and a strong increase in temperature are detected. Surgery is used to remove the inflamed area. This procedure is safe for a pregnant woman. Abdominal laparotomy appendectomy is used if peritonitis is suspected and less invasive laparoscopy is used if there are no signs of peritonitis. A course of rehabilitation therapy is prescribed.
It is possible to diagnose the pathology based on additional symptoms. Treatment should be supervised by medical professionals. It is prohibited to take pharmaceutical drugs on your own. If you aggravate your own condition through inept actions, this will inevitably affect the child’s development.
Changes in the mother's body
The woman becomes calmer. She notices and feels changes in her body, and begins to take a more responsible attitude towards her health.
Some mothers become overly focused on themselves and their feelings and stop paying attention to the needs of their spouse.
Appetite stabilizes. If it remains elevated, the body may be experiencing a lack of vitamins.
The weight of a pregnant woman increases by 4.5-6 kg by this time. The maximum threshold is 6300. If a woman has gained 7 kilograms or more, this is a reason for additional examination.
Attitude to sex
If there are no contraindications or risk of interruption, sex is allowed at this time. It is necessary to avoid poses on the stomach, as well as those that put pressure on the stomach. Ideal options are on the side and the woman on top (in the latter case, the pregnant woman will be able to control the depth of penetration).
A woman may lose interest in sex due to hormonal changes and if she is very afraid of harming the baby. If the desire persists, the sensations during intimacy become more vivid.
hCG
The level of choriogonic gonadotropin gradually decreases. Its amount ranges from 10 thousand to 35 thousand honey/ml.
Progesterone
Progesterone levels rise to 72-75 nmol/l. This hormone ensures increased elasticity of muscles and ligaments. Causes a gradual divergence of the pelvic bones. This happens so that during childbirth the baby passes through the birth canal.
For many women, pelvic expansion causes discomfort: from mild aching pain in the pelvic joints to quite noticeable joint pain. Progesterone helps reduce pain.
Endometrium
The thickness of the endometrium at this stage reaches several tens of millimeters. Under the influence of hormones, small nodes may resolve if they were there before.
When do you need to see a doctor urgently, and which doctor will help?
Cases of pain where medical intervention cannot be avoided:
- Cramping attacks of a pulling nature (especially in the first trimester of pregnancy) - you need to immediately seek help. There is a high risk of miscarriage or placental abruption. The presence of mucous discharge mixed with blood is a reason to call an ambulance for immediate hospitalization of the patient.
- Shingles with a return to the lower back in the presence of a burning sensation at the time of urination - signs of the development of pyelonephritis. Long-term treatment may be required. Signs of illness should be reported immediately.
- In the later stages, accompanied by contractions and increased uterine tone - a sign of premature birth.
Regardless of the stage of pregnancy, the appearance of bleeding from the vagina with or without pain - you should definitely call an ambulance.

Consulting a pregnant woman and caring for the patient during pregnancy is the responsibility of the local obstetrician-gynecologist. They work in district antenatal clinics.
You can get an appointment with them in the following ways:
- through an electronic appointment system;
- by calling the registration number of the medical institution;
- Some consultations retained the journal recording system.
If the pain is not associated with the course of pregnancy and does not affect the development of the fetus, then you need to contact your local physician. It is important that treatment is selected taking into account saving the life and health of the mother and child.
Medical and lifestyle advice
It is important to adhere to proper nutrition and avoid prolonged bowel retention. You need to control your drinking regime and not reduce the volume of fluid consumed - on the contrary, you can increase it slightly. Reducing the amount of water you drink can lead to increased blood viscosity, the risk of blood clots, and a decrease in the volume of amniotic fluid.
You need to move moderately. If you have problems sleeping, take a walk in the evening. If there was a risk of miscarriage, which has already gone away, you can resume gymnastics and yoga classes for pregnant women.
It's time to learn to breathe correctly. Breathing techniques will help put your nerves in order and not stress your baby. There will also be time to fully master breathing exercises. You can learn proper breathing on your own, but it is better to do it at a school for expectant mothers.
Scheduled doctor visits
To make sure that a woman is tolerated well by pregnancy, there is no threat to her health, you need to do an electrocardiogram. It will show how well the heart can cope with the load (increased weight, increased blood volume).
A preventative visit to the dentist wouldn't hurt. If a woman has pockets of caries that do not require painful treatment and tooth extraction, it is better to clean and fill them to neutralize the infection in the oral cavity. If your gums are bleeding excessively, your doctor will recommend additional measures.
A visit to the ophthalmologist will allow you to assess the condition of your vision (especially the retina), and identify possible contraindications to natural childbirth (if there is a high risk of detachment).
A visit to an otolaryngologist is also scheduled. It will help identify existing chronic diseases and neutralize their possible impact on the fetus.
Necessary studies and analyzes
It's time to get tested for hemoglobin levels, since many pregnant women experience anemia.
You also need:
- Test urine for protein.
- Get a blood sugar test to rule out gestational diabetes. If the results are disputable, a glucose tolerance test is required.
It is necessary to undergo examination for TORCH infections, if it has not been carried out previously. If there are complaints and unpleasant symptoms, a vaginal smear and a general blood and urine test are taken.
Diet
Since fetal growth accelerates at this time, the mother needs to carefully monitor her diet. During this period, it is necessary to reduce the consumption of fats (but not remove them completely), and consume sweets to a minimum.
The diet should be varied and balanced. Products with fiber, as well as vegetable oils (they can be added to salads and cereals) will help cope with constipation.
Cabbage, legumes, and sweet juices should be limited, or better yet, eliminated altogether: they cause increased gas formation.
Lean meat, especially beef, as well as nuts (a source of omega-3 fatty acids) are a must in the diet: this will help prevent anemia and have a positive effect on the development of the child’s brain and nervous system.
To prevent anemia, meat should be supplemented with buckwheat, pomegranates and liver. It is important not to overeat: let there be more meals, but they will be fractional.
Lifestyle
As long as the stomach does not restrict movement, the expectant mother can walk - and it is advisable to do this more often. You should not go on a 6-7-hour continuous marathon: two hour walks in the morning and evening will be enough.
If you work, you need to take regular breaks. Going on vacation will also be beneficial. Moreover, long journeys are not yet prohibited.
If there is no threat to the health of mother and child, you should not give up physical activity: you can go to the pool and do special gymnastics for pregnant women.
Since the child begins to feel the difference between lighting modes, it is worth paying special attention to the daily routine: do not stay up late and do not sleep until noon. You should also avoid attending noisy concerts, parties, and cinemas with special effects.
What's prohibited?
To avoid circulatory problems, the expectant mother should not stay in one position for a long time. If your job is sedentary, you need to get up and stretch a little every 40 minutes. Staying in an upright position for a long time is also undesirable: a rush of blood to the uterus can provoke its hypertonicity.
You cannot run or walk quickly, even if you are 30 meters from the bus stop. It is better to wait for the next one than to chase after the one leaving, risking falling. You should avoid traveling in crowded transport.
In slippery weather you need to be extremely careful; if possible, do not leave the house at all.
If the house is undergoing renovations (many parents start renovations in the nursery just at this time, when most of the threats have passed), it is better to entrust all the work to builders or household members: breathing paint, varnish and even wallpaper glue is harmful for a pregnant woman.
You should also avoid smoked foods, especially store-bought ones, soda, and undercooked fish and meat, so as not to provoke allergies or food poisoning. It is also undesirable to try exotic products.
Taking vitamins
If a woman is healthy and tolerates pregnancy well, eats well, she does not need multivitamin complexes - vitamin D and calcium are enough, which are necessary for the development of the fetal skeletal system. If there are disturbances in health, appetite, or anemia is diagnosed, vitamin supplements are necessary. But their composition and dosage should be prescribed by a doctor after several tests.
Should I wear a bandage?
Most pregnant women start wearing a brace between 20 and 24 weeks. But for some, already at 19, it’s hard to cope with their stomach. If your lower back hurts often, it is better to start wearing a bandage at 19 weeks of pregnancy. This will help maintain the mother’s emotional state and relieve her of negative emotions and pain.
You need to choose the most comfortable one, which supports, but does not press on the stomach and does not irritate the skin.
What do doctors prescribe?
By this time, the placenta begins to work as a full-fledged filter. If just a few weeks ago most medications for mothers were prohibited, then by week 19 some of the medications can be used. The main thing is to follow the doctor’s recommendations and read the instructions carefully.
In the absence of indications, the doctor simply monitors the condition of the pregnant woman. If you are not prescribed even simple multivitamins, then there is no need for it. If there are infections, including genital infections, the doctor can prescribe the most gentle antibiotics if the harm from them is several times less than intrauterine infection of the fetus.
If you suspect diabetes mellitus, preeclampsia, or a tendency to form blood clots, the doctor may prescribe an additional examination, and only then treatment.
Top medications to reduce abdominal pain during pregnancy and breastfeeding, painkillers
Painkillers are not advisable during pregnancy. Especially in the first months, when the main formation of organs and tissues of the future person occurs. However, the process of experiencing discomfort caused by constant negative factors also does not bode well.
Before purchasing analgesics, consultation with a specialist is required. It is advisable to try non-pharmaceutical ways to cope with discomfort.
The least dangerous drug is Paracetamol. Suitable for use throughout the entire gestation period. Toxic components are in minimal concentration and are quickly excreted in the urine.
Ibuprofen is a non-steroidal anti-inflammatory drug. Prescribed with caution during the second trimester. Contraindicated for the first and third trimester. Use may cause a number of dangerous side effects. If your condition changes slightly for the worse while taking an analgesic, you should inform your doctor.
Indomethacin also belongs to the group of non-steroidal anti-inflammatory drugs. It is subject to the same restrictions as Ibuprofen. If taken continuously, there is a risk of damage to the child's kidney function.
For the first two trimesters, it is permissible to use creams and ointments based on:
- Diclofenac.
- Ketoprofen.
- Ketorolac.
In the third trimester, you can only use local products based on herbal ingredients. It is forbidden to apply them if they contain bee or snake venom.
Ointments with an irritating effect that stimulate increased blood circulation can also have a negative effect. There is a risk of developing uterine tone and high blood pressure.
The most powerful painkillers are classified as narcotic substances and are prohibited for free sale. Their use occurs only in a hospital with extremely severe pain. These are drugs based on morphine and codeine.
The list of chemical compounds for pharmaceutical use during pregnancy is extremely limited. Before you start taking it, you should read the instructions for use in detail and strictly follow the manufacturer’s recommendations on dosage and method of use.
It is important to familiarize yourself with the provisions on common side effects and contraindications.
It is possible to use folk and non-traditional methods of getting rid of suffering. For example, yoga for pregnant women, acupuncture, light massage, aromatherapy. Traditional methods are also used. But their use also needs to be discussed with a specialist.
Preventive measures to avoid abdominal pain
The basis of prevention is the correct lifestyle of a pregnant woman:
- No stress factors. The mental state of the mother is the key to the health of the child. The fetus inside a woman reacts sensitively to changes in the mother’s emotional background. He is not able to recognize the causes of depression or fears, but he is aware that adverse events are occurring. If the mother is very worried, there is a risk of pathological changes during the formation of the future person. Neurological and psychological problems are possible.
- Elimination of physical fatigue. Pregnant women are not recommended to attend training regularly. During active sports, blood pressure levels increase noticeably. This will provoke the development of uterine tone, which will inevitably lead to adverse consequences. You can go for walks in the fresh air.
- Properly designed diet and nutrition schedule. It must be balanced. You should not consume fast food products or preservatives; it is recommended to reduce the amount of tea and coffee. It should consist of vegetables, fruits, animal and plant protein. It is worth taking vitamins prescribed by a doctor for those who are pregnant. Weight control is required, since the percentage of subcutaneous fat outside the normal range negatively affects the functioning of the cardiovascular system and gastrointestinal tract. The feeding processes of the fetus are disrupted. With rapid weight gain, nutritional correction and a special diet may be prescribed. Excess weight contributes to decreased activity, bad mood, and additional pain in the back and joints. Make sure there is no overeating.
- Maintaining a sleep and rest schedule ensures that a woman is highly active. She does not feel tired and overwhelmed, which means she has a positive morale.
- Regular observation by an obstetrician-gynecologist according to the established schedule, passing mandatory tests, compliance with received medical recommendations. Undergoing developmental ultrasound examinations and other diagnostic measures.
- Tracking the development of chronic pathologies that were diagnosed before pregnancy.
- Prompt treatment of colds, bacterial and viral diseases acquired during pregnancy.
- Eliminate all bad habits, such as alcohol, smoking, and drug use. Failure to comply with this rule results in a developmental delay in the baby.
- Monitoring blood pressure for hypertension (high blood pressure) or hypotension (low blood pressure). Monitor your sugar levels if you are diagnosed with diabetes.
- Do not take a hot bath or shower, or a contrast shower. A sharp change in ambient temperature threatens a rise in pressure and disruption of the cardiovascular system.
Compliance with these rules will ensure comfortable and proper pregnancy. The pain will be considered obstetrically safe. But even if you follow all the recommendations, you need to carefully monitor your own condition and, if there are reasons, seek medical help.
What does sudden abdominal pain mean?
The suddenness of the development of pain is a sign of an acute form of pathology. If the sensation is localized on the right side, accompanied by nausea, vomiting, dizziness, there is a risk of developing inflammation of the appendix.
Immediate hospitalization and surgical intervention are required before perforation begins. Removing appendicitis is a common procedure for surgeons. It passes without complications.
During pregnancy, the operation is performed in compliance with all required patient safety criteria.
Non-obstetric types of pathological pain of a sudden acute nature include:
- intestinal obstruction;
- peritonitis.
As with appendicitis, acute pain accompanied by vomiting and general weakness. The syndrome extends to the lower abdomen, lower back, sacrum, and groin.
Unilateral, accompanied by bleeding from the vagina - a sign of ectopic pregnancy.
Additional signs of a dangerous condition:
- cramping character;
- increased symptoms in a horizontal position of the body;
- severe vomiting;
- shortness of breath at rest;
- frequent heartbeat, which in frequency goes above 100 beats per minute.
In the absence of medical attention, the fallopian tube ruptures. Internal bleeding begins.
What about the fruit?
It is actively growing and developing. At this point, the rudiments of all teeth (deciduous and permanent) are formed. The child becomes more active. The baby is actively gaining weight, growing faster than in previous weeks.
Important! If at this time a breech presentation is noticeable on an ultrasound, there is no cause for concern: during the remaining half of the term, the baby will have time to change position several more times.
How is it developing?
The week is marked by important events:
- The child’s brain is almost completely formed, and the areas responsible for the senses are already beginning to function.
- Movements become conscious, the baby learns to move his arms and legs.
- A swallowing reflex appears.
- Bones begin to form.
- The baby hears, feels the mother’s mood, and can distinguish between light and darkness.
- The digestive system is formed, the original feces are deposited - meconium, which consists of excess cells and thickened bile.
- The kidneys and urinary system begin to work. Small portions of urine are excreted into the amniotic fluid.
The baby's heart beats at a speed of 160 beats per minute. The skin and blood vessels are fully formed. The main organs are formed, but for now - in a smaller version. They will actively develop in the coming weeks.
What does it look like?
Almost like a fully formed baby: head, body, limbs, fingers. With a detailed ultrasound, you can see the baby's facial expression. If the child is in a comfortable position, you can determine who the expectant mother is expecting: a boy or a girl.
The body becomes proportional. Thin hair appears on the head. Small fat reserves begin to be deposited on the cheeks, chest and kidney area. They will enlarge so that immediately after birth the baby can use them as a source of energy.
Weight and height
The height of the fetus is about 15 centimeters. Its size is comparable to a grapefruit, medium potato or large tomato. The weight of the fruit is from 200 to 300 grams.
Movements
Most expectant mothers feel the first tremors of the baby during this period. This is due to the fact that the baby’s movements become controlled and manageable. For some, already at this stage, activity reaches 7-8 times per hour.
Very vigilant mothers may mistake intestinal colic or gas movement for movement. If the baby has not yet begun to move, do not worry: the norm is the absence of movements until 22 weeks.