21 weeks pregnant how many months is it? - You are almost a week into the second trimester of pregnancy. Hopefully you've had your mid-pregnancy screening done and you're all set. All you need to do is take better care of yourself so that the next few months pass without complications.
Why does my stomach hurt at 21 weeks of pregnancy?
Pain at 21 weeks does not always indicate pathology.
This symptom is associated with the following natural processes:
- The uterus expands, pressure begins on the abdominal cavity.
- The pelvic bones move apart to allow the baby to pass through the birth.
- A large fruit helps to shift the center of gravity of the body.
- New hormones appear in the body.
But there are pathological ailments that can be dangerous. Therefore, if you have any unpleasant feelings, you should consult your doctor.
Pathologies that cause the disorder:
- The tone of the uterus is a girdle pain, radiating to the lower back, mild, the stomach turns to stone.
- Risk of miscarriage - strong, cutting sensations, accompanied by bleeding, spotting brown discharge.
- Premature birth – is present for a long time, has a cramping character, pulls the bottom as during menstruation.
- Placental abruption is characterized by intense bleeding, as a hematoma occurs between the placenta and the uterus.
There are a number of chronic diseases, the exacerbation of which occurs due to an enlarged uterus, putting pressure on some internal organs. The woman feels discomfort.
Such diseases include:
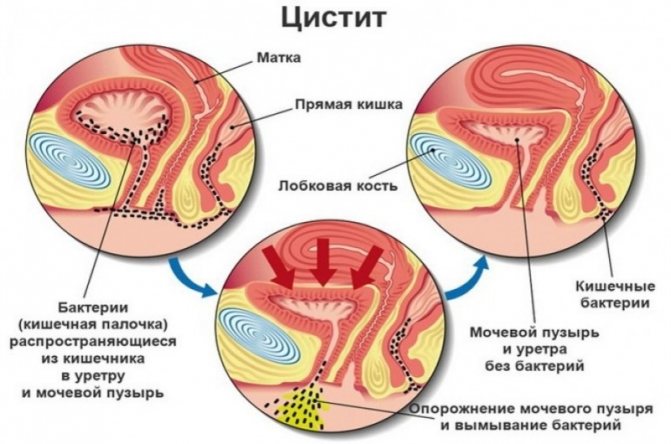
- infection, inflammation of the bladder;
- thrush;
- diseases of the ovaries, fallopian tubes;
- STI;
- ovarian cysts (usually their rupture);
- acute appendicitis;
- inguinal hernia;
- radiculitis;
- disbacteriosis in a neglected state;
- symphysitis of the symphysis pubis;
- pathologies of the gallbladder and pancreas.
If everything is within normal limits, pain can be eliminated by changing body position, for example, lying on the other side.
If the disorder persists, it is recommended to call an ambulance to avoid worsening the condition. At an early stage, all consequences can be circumvented and the pregnancy can be maintained.
Pain
The 21st week of pregnancy can be distinguished by the appearance of a wide variety of pains that arise due to the body being thoroughly “adapted” for bearing and further birth of a child.
It is likely that now you will experience pain in your navel and a feeling of pressure on your stomach in this area from the inside. The fact is that the uterus has now reached just such a standing height at which it begins to put pressure on the navel. As pregnancy progresses, when the uterus passes this section of the path, the pain in the navel and the feeling of pressure on it will go away on its own.
The weight that has increased over the previous time also causes significant stress on the legs and, in particular, the knee joints. It is not surprising that at the end of the day a woman may experience pain in her legs, and at night wake up from cramps in her legs. By the way, cramps during this period are also a consequence of the increased need and, probably, lack of calcium in the pregnant woman’s body, which is now consumed to the maximum by the growing fetus. To reduce problems associated with pain and fatigue in the legs, and to avoid cramps, it is advisable to increase your dietary intake of calcium-containing foods, and also give your legs a rest regularly throughout the day. Stay in a standing position less, when sitting down, do not cross your legs, taking a horizontal position - raise your legs to a height, for example, on the cushion of a sofa. It is good to massage your legs and feet in the evenings, and take warm foot baths with the addition of a decoction of soothing herbs.
As your weight increases, the stress on your spine and lower back will increase. To avoid back pain, avoid prolonged walking and sitting, do not sit on chairs without a backrest, learn to get out of bed correctly (first lower your legs to the floor, and only then get up yourself), lift and carry heavy objects: it is better to distribute the load equally in two hands, and bending down, slightly spread your legs to the sides and sit down, bending them at the knees; If you lift something heavy, distribute the load across your buttocks, hips and shoulders.
What causes nagging, aching pain during pregnancy?
A woman’s body undergoes a major restructuring, accompanied by inconvenience and malfunction of the body system. The disturbances cause a nagging, aching pain in the abdomen.
This is usually a symptom:
- Intestinal obstruction, stagnation of feces.
- Constipation, diarrhea.
- Accumulations of intestinal gases.
- Tension of ligaments.
- Lack of vitamins.
A woman must be observed in a antenatal clinic and tell the gynecologist about the discomfort that is bothering her. The doctor determines the type of sensations, selects drugs that are safe for the fetus, a method of therapy, and prescribes additional tests.
Fetus
The average weight of the fetus is 350-400 grams, and its height is 27 cm.

This week the fetus:
- The skin is coated with a protective lubricant that protects it from external influences. The subcutaneous fat layer begins to form.
- The endocrine system and glands that produce hormones are activated.
- The digestive system is actively developing: the fetus swallows a large amount of amniotic fluid, training the digestive tract.
- The processes of hematopoiesis are improved, and from the 21st week the spleen begins to work actively.
- The fetal bones and muscles continue to strengthen. The child is actively moving.
- The vestibular apparatus is formed, which is responsible for orientation in space.
- Sense organs develop: the fetus discerns taste and begins to hear.

Fetus at 21 weeks of gestation
SPA therapy for the expectant mother
Spa treatments for pregnant women are useful.
They relieve psychological stress and help eliminate the effects of hormonal changes:
- stretch marks;
- cellulite;
- swelling;
- pigmentation;
- dilatation of veins
The following physiotherapy programs are allowed for expectant mothers:
- Peeling.
- Algae, oil wraps without a warming effect.
- Lymphatic drainage massage.
- Massage of the collar area.
There are always restrictions when pregnant, and in the spa you need to adhere to some rules:
- The preparations used must be made from natural ingredients.
- Use essential oils carefully.
- The duration of the procedure is no more than two hours.
What does dull, pulling, point or cutting pain in the abdomen indicate?
Stomach pain during pregnancy is due to changes in the body, in organs associated with hormonal changes, changes in the position of internal organs, and obstetric pathologies.
Many types of these sensations do not pose a threat to the health of the mother or the condition of the fetus. Others cause significant harm and even death to the woman and the unborn child.
Pain is a reaction of the nervous system to stimuli. A symptom of many diseases, including obstetric pathologies during pregnancy. A pregnant woman experiences hormonal changes and a restructuring of many systems. They are also accompanied by this feeling.
If discomfort and pain occur, it is better to consult with your doctor about the nature of these sensations and appropriate treatment. During pregnancy, a woman is responsible not only for her own health, but also for the health of the baby.

Nature has determined that the mother’s body tries to protect the fetus from all negative influences. A plug formed from mucus in the cervix prevents pathogenic microorganisms from entering.
Umbilical cord nutrition is formed in such a way that harmful chemical compounds do not enter the fetus. The uterus itself protects the child from external mechanical influence.
At the same time, during the period of bearing a baby, the woman herself may regularly experience pain of varying intensity and nature. Each type of discomfort indicates the presence of different pathological conditions, with the exception of harmless obstetric ones associated with changes in the maternal body and preparation for childbirth.
Based on the nature, intensity of pain, and gestational age, we can talk about how dangerous the condition is.
For example, pulling, extending to the lower back and groin, may indicate a risk of miscarriage. An additional sign of the condition will be the presence of bloody discharge.
In this case, you should immediately seek medical help and undergo an examination. If you delay visiting a doctor, the frequency of contractions will become more frequent and spontaneous miscarriage will occur.
Uterine tone is dangerous regardless of how early it was diagnosed. The fetus may experience a lack of oxygen and incoming nutrients. The woman feels a sharp pain like contractions. The solid state of the uterus and lower abdomen is recorded.
In case of injury, late toxicosis, or stress, placental abruption may occur. The condition is accompanied by acute pain in the lower abdomen. Often there is internal bleeding without external manifestations in the form of discharge. Urgent hospitalization and surgical intervention are required. Without help, death will occur.
Cramps accompanied by dizziness at five to twelve weeks can be a symptom of an ectopic pregnancy. For a number of reasons, the egg was unable to enter the uterus and became embedded in the fallopian tube.
As a result of the rapid growth rate of the fertilized egg, severe pain occurs. The woman is sent for an ultrasound examination. An operation to terminate the pregnancy is prescribed. Lack of medical care will result in death for the pregnant woman.
A number of non-gynecological problems also contribute to the occurrence of unpleasant sensations in the lower abdomen:
- Disruption of the gastrointestinal tract. Additional symptoms: bitterness in the mouth, tingling in the lower abdomen, heartburn.
- Inflammation of the bladder and urinary tract. Symptoms: discomfort and burning when urinating, increased frequency of the urge to urinate, increased body temperature.
- Seasonal colds. They are accompanied by headaches, nasopharyngeal congestion, aching bones, and fever.
- Inflammation of the appendix (appendicitis). An acute condition in which severe vomiting occurs, weakness, and a strong increase in temperature are detected. Surgery is used to remove the inflamed area. This procedure is safe for a pregnant woman. Abdominal laparotomy appendectomy is used if peritonitis is suspected and less invasive laparoscopy is used if there are no signs of peritonitis. A course of rehabilitation therapy is prescribed.
It is possible to diagnose the pathology based on additional symptoms. Treatment should be supervised by medical professionals. It is prohibited to take pharmaceutical drugs on your own. If you aggravate your own condition through inept actions, this will inevitably affect the child’s development.
Baby's movements
It would seem that just recently the expectant mother was impatiently waiting for the first movements of the fetus to appear, and after a few weeks it became so active that one can distinguish between periods of its sleep and wakefulness. This is due to the active development of the child’s musculoskeletal system. Some women claim that they can distinguish which part of the body the baby has turned towards the front wall of the uterus.
What can be said for sure is that it is already possible to understand in which half of the abdomen the child is located, moving inside the uterus. At such moments, it is visually noticeable how the stomach slightly increases on one side and decreases on the other.
The movements can become too intense when a woman is in an unventilated and stuffy room for a long time. The baby senses a lack of oxygen and, by moving, stimulates the work of his heart for the active exchange of blood and the supply of oxygen to it.
Sometimes the baby’s activity increases noticeably when the expectant mother needs rest and a night’s sleep. In such cases, perinatal psychologists recommend calming the baby down by gently stroking his belly, singing him a song, and playing soft, calm music.
When do you need to see a doctor urgently, and which doctor will help?
Cases of pain where medical intervention cannot be avoided:
- Cramping attacks of a pulling nature (especially in the first trimester of pregnancy) - you need to immediately seek help. There is a high risk of miscarriage or placental abruption. The presence of mucous discharge mixed with blood is a reason to call an ambulance for immediate hospitalization of the patient.
- Shingles with a return to the lower back in the presence of a burning sensation at the time of urination - signs of the development of pyelonephritis. Long-term treatment may be required. Signs of illness should be reported immediately.
- In the later stages, accompanied by contractions and increased uterine tone - a sign of premature birth.
Regardless of the stage of pregnancy, the appearance of bleeding from the vagina with or without pain - you should definitely call an ambulance.

Consulting a pregnant woman and caring for the patient during pregnancy is the responsibility of the local obstetrician-gynecologist. They work in district antenatal clinics.
You can get an appointment with them in the following ways:
- through an electronic appointment system;
- by calling the registration number of the medical institution;
- Some consultations retained the journal recording system.
If the pain is not associated with the course of pregnancy and does not affect the development of the fetus, then you need to contact your local physician. It is important that treatment is selected taking into account saving the life and health of the mother and child.
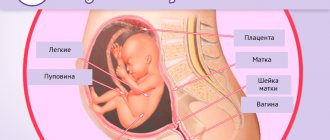
Special problems – low placentation
During a routine ultrasound, the doctor may discover that a woman has low placentation, or placenta previa. In this case, the placenta is not located at the bottom of the uterus or at the side wall, but opposite the pharynx of the cervical canal. This condition is considered a pathology that threatens pregnancy. In some cases, placental abruption occurs, which leads to the death of the fetus. At this stage of termination of pregnancy, the child is not yet able to survive. When diagnosing placenta previa, a woman is advised to abstain from sex and any physical activity; constant medical supervision is required.
Top medications to reduce abdominal pain during pregnancy and breastfeeding, painkillers
Painkillers are not advisable during pregnancy. Especially in the first months, when the main formation of organs and tissues of the future person occurs. However, the process of experiencing discomfort caused by constant negative factors also does not bode well.
Before purchasing analgesics, consultation with a specialist is required. It is advisable to try non-pharmaceutical ways to cope with discomfort.
The least dangerous drug is Paracetamol. Suitable for use throughout the entire gestation period. Toxic components are in minimal concentration and are quickly excreted in the urine.
Ibuprofen is a non-steroidal anti-inflammatory drug. Prescribed with caution during the second trimester. Contraindicated for the first and third trimester. Use may cause a number of dangerous side effects. If your condition changes slightly for the worse while taking an analgesic, you should inform your doctor.
Indomethacin also belongs to the group of non-steroidal anti-inflammatory drugs. It is subject to the same restrictions as Ibuprofen. If taken continuously, there is a risk of damage to the child's kidney function.
For the first two trimesters, it is permissible to use creams and ointments based on:
- Diclofenac.
- Ketoprofen.
- Ketorolac.
In the third trimester, you can only use local products based on herbal ingredients. It is forbidden to apply them if they contain bee or snake venom.
Ointments with an irritating effect that stimulate increased blood circulation can also have a negative effect. There is a risk of developing uterine tone and high blood pressure.
The most powerful painkillers are classified as narcotic substances and are prohibited for free sale. Their use occurs only in a hospital with extremely severe pain. These are drugs based on morphine and codeine.
The list of chemical compounds for pharmaceutical use during pregnancy is extremely limited. Before you start taking it, you should read the instructions for use in detail and strictly follow the manufacturer’s recommendations on dosage and method of use.
It is important to familiarize yourself with the provisions on common side effects and contraindications.
It is possible to use folk and non-traditional methods of getting rid of suffering. For example, yoga for pregnant women, acupuncture, light massage, aromatherapy. Traditional methods are also used. But their use also needs to be discussed with a specialist.
Medical examination
Screening
By week 21, as a rule, the second scheduled screening has already been carried out and its results are known. In the 2nd trimester, screening consists of a triple test for genetic abnormalities and ultrasound. If, based on the screening results, doctors suspect that the fetus has a pathology, additional studies may be required.
The goals of ultrasound examination at this stage are:
- Identification of various pathologies of fetal development.
- Assess the condition of the placenta, umbilical cord, cervix and amniotic fluid.
- Assess the state of blood flow using Doppler sonography.
- Determine the sex of the child.

Visit to the gynecologist
During the scheduled visit at week 21, the doctor makes the following entries in the exchange card:
- weight gain,
- height of the uterus,
- abdominal circumference,
- arterial pressure,
- Fetal heart rate,
- results of a general blood and urine test taken before visiting the doctor.
Based on the results of the examination of the pregnant woman, the doctor gives recommendations and, if a pathology of fetal development is suspected, prescribes additional tests for diagnosis.
Preventive measures to avoid abdominal pain
The basis of prevention is the correct lifestyle of a pregnant woman:
- No stress factors. The mental state of the mother is the key to the health of the child. The fetus inside a woman reacts sensitively to changes in the mother’s emotional background. He is not able to recognize the causes of depression or fears, but he is aware that adverse events are occurring. If the mother is very worried, there is a risk of pathological changes during the formation of the future person. Neurological and psychological problems are possible.
- Elimination of physical fatigue. Pregnant women are not recommended to attend training regularly. During active sports, blood pressure levels increase noticeably. This will provoke the development of uterine tone, which will inevitably lead to adverse consequences. You can go for walks in the fresh air.
- Properly designed diet and nutrition schedule. It must be balanced. You should not consume fast food products or preservatives; it is recommended to reduce the amount of tea and coffee. It should consist of vegetables, fruits, animal and plant protein. It is worth taking vitamins prescribed by a doctor for those who are pregnant. Weight control is required, since the percentage of subcutaneous fat outside the normal range negatively affects the functioning of the cardiovascular system and gastrointestinal tract. The feeding processes of the fetus are disrupted. With rapid weight gain, nutritional correction and a special diet may be prescribed. Excess weight contributes to decreased activity, bad mood, and additional pain in the back and joints. Make sure there is no overeating.
- Maintaining a sleep and rest schedule ensures that a woman is highly active. She does not feel tired and overwhelmed, which means she has a positive morale.
- Regular observation by an obstetrician-gynecologist according to the established schedule, passing mandatory tests, compliance with received medical recommendations. Undergoing developmental ultrasound examinations and other diagnostic measures.
- Tracking the development of chronic pathologies that were diagnosed before pregnancy.
- Prompt treatment of colds, bacterial and viral diseases acquired during pregnancy.
- Eliminate all bad habits, such as alcohol, smoking, and drug use. Failure to comply with this rule results in a developmental delay in the baby.
- Monitoring blood pressure for hypertension (high blood pressure) or hypotension (low blood pressure). Monitor your sugar levels if you are diagnosed with diabetes.
- Do not take a hot bath or shower, or a contrast shower. A sharp change in ambient temperature threatens a rise in pressure and disruption of the cardiovascular system.
Compliance with these rules will ensure comfortable and proper pregnancy. The pain will be considered obstetrically safe. But even if you follow all the recommendations, you need to carefully monitor your own condition and, if there are reasons, seek medical help.
Prevention
Prevention measures are known and available to all women; it is only necessary to apply this knowledge in practice:
- It is worth limiting your social circle, not communicating with strangers on the street, in a hospital, or on public transport, so as not to catch an infection.
- Protect yourself from hypothermia.
- Dress according to the season, do not wear too warm clothes in hot weather, dress warmer in cold weather.
- Eat healthy food, consume enough vitamins and microelements.
- Ventilate the living space where you spend the most time.

To avoid getting ARVI, it is important to dress according to the season.
These preventive measures will reduce the risk of illness, but even if you are already sick, there is no need to be too upset, because there are safe treatment methods, which will be presented below.
We also recommend: ARVI at 20 weeks of pregnancy
What does sudden abdominal pain mean?
The suddenness of the development of pain is a sign of an acute form of pathology. If the sensation is localized on the right side, accompanied by nausea, vomiting, dizziness, there is a risk of developing inflammation of the appendix.
Immediate hospitalization and surgical intervention are required before perforation begins. Removing appendicitis is a common procedure for surgeons. It passes without complications.
During pregnancy, the operation is performed in compliance with all required patient safety criteria.
Non-obstetric types of pathological pain of a sudden acute nature include:
- intestinal obstruction;
- peritonitis.
As with appendicitis, acute pain accompanied by vomiting and general weakness. The syndrome extends to the lower abdomen, lower back, sacrum, and groin.
Unilateral, accompanied by bleeding from the vagina - a sign of ectopic pregnancy.
Additional signs of a dangerous condition:
- cramping character;
- increased symptoms in a horizontal position of the body;
- severe vomiting;
- shortness of breath at rest;
- frequent heartbeat, which in frequency goes above 100 beats per minute.
In the absence of medical attention, the fallopian tube ruptures. Internal bleeding begins.
How to recognize ARVI?
Popularly, a respiratory infection is simply called a cold, and during pregnancy this disease has the same symptoms as in non-pregnant women, namely:
- Difficulty breathing due to nasal congestion.
- Severe runny nose.
- Watery eyes and redness of the eyelids.
- Dry or wet cough.
- Sneezing, sore throat.
- General weakness and drowsiness.
- Dizziness.
We also recommend: ARVI at 33 weeks of pregnancy
As a rule, in everyday life, people begin to be treated with aspirin, other medications, and reduce the temperature with antibiotics, but all this cannot be counted on during pregnancy, because many medications are contraindicated during this period.
Doctors recommend immediately contacting an experienced therapist who will conduct an examination, prescribe appropriate tests and prescribe the necessary treatment.

With ARVI, a pregnant woman experiences coughing, sneezing, runny nose and other symptoms