Hello, dear readers! In the article we explain why a child sweats a lot after an illness and determine the severity of the condition. Here we introduce the reader to special cases that require attention from parents and specialists. Don’t forget to also give valuable advice on how to get rid of the unpleasant symptom and restore the baby’s condition.
Sweating in children: is it normal?
The process of sweating is completely normal. It is carried out due to the work of the sweat glands and is responsible for many processes in the body. There are two types of glands: apocrine and eccrine. The former are present only in some parts of the body and are responsible for the release of pheromones, which determine the natural smell of a person. The latter have greater functionality. They participate in acid-base metabolism, protect the skin from bacteria, carry out thermoregulation of the body and participate in the elimination of toxins.
In children before puberty, only the eccrine glands work. They cover the entire body, but in some areas their concentration is especially high. Under normal conditions, the body produces a small amount of sweat, which quickly evaporates from the surface of the skin. When enhanced thermoregulation is necessary, for example, during physical activity, this secretion is released in large quantities.
Sweating is considered pathological if the secretion is released in large quantities at a moment of complete physical and emotional rest. If the child’s nervous system is excited or he is actively doing something, then increased sweating is quite natural.
Why does a person sweat when he has a cold?
As you probably remember from the basic physics course, liquid evaporating from a surface cools this surface. The sweating system works on the same principle, cooling our body.
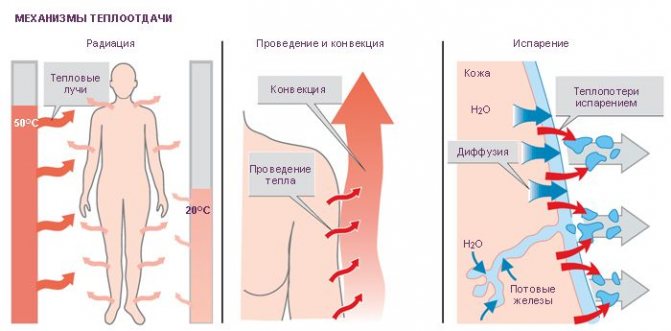
The principle of cooling the body through sweating.
But in addition to the main function, sweat is also necessary for a person to remove waste and toxins harmful to the body, as well as regulate water and salt balance. Therefore, doctors have long concluded that there are only two reasons for sweating during a cold:
1. Increased body temperature. Infection of the upper respiratory tract with pathogenic microorganisms provokes the body to produce antibodies necessary to destroy the infection. This is why the body temperature rises, as a result of which the sweating system is activated, which tries to normalize it.
This manifestation is completely natural, and attempts to reduce or completely eliminate sweating are not only not rational, but can also significantly harm the body. After all, attempts to prevent sweating, which is normal for this condition, will only cause even greater overheating of the body, which can reach temperatures critical for life.
In addition, an independent reduction in sweating at elevated temperatures indirectly affects the effectiveness of fighting infection. The higher the temperature, the more antibodies needed to destroy the infection are produced by the immune system. That is why doctors do not recommend taking antipyretic drugs until the body temperature exceeds 38 degrees.
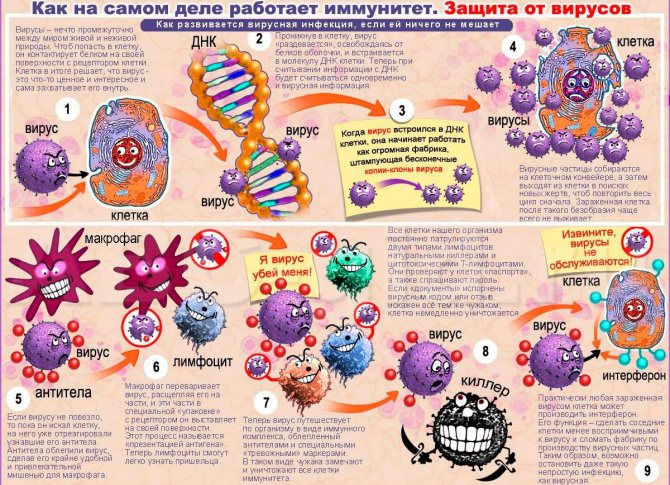
The principle of the immune system fighting infection, which also provokes sweating.
2. Removal of toxins and waste. The second reason for stronger sweating compared to the normal state of the body is the increased concentration of toxic substances. But where do they come from? As a rule, these are ordinary waste products of bacteria, which, when bacteria actively multiply, accumulate in quantities that are enormous for the body and cause severe intoxication. Its symptoms are headaches, nausea, weakness and profuse sweating.
The role of the latter is precisely to remove these toxins from the body. Attempts to stop sweat during a cold only aggravate the patient’s general condition and intensify the symptoms of intoxication.
However, there are cases, or rather conditions of the patient, accompanied by sweating during a cold, in which you should really be wary:
- Hypertension. In a person suffering from hypertension, sudden bursts of sweating can cause an increase in blood pressure. In this case, you need to consult a doctor, and then strictly follow his recommendations, observing only bed rest.
- Carrying a cold on your feet. Heavy sweating in the absence of bed rest leads to extremely negative consequences. The fact is that the patient’s clothes constantly become wet and cold, which leads to severe hypothermia and a decrease in the already weakened immune system.
- Presence of skin diseases and injuries. Large volumes of sweat released irritate the skin, provoke the development of various allergic reactions and diseases, and also aggravate existing defects. In addition, under the influence of the bacterial flora in the body, it is possible that an inflammatory process may develop directly in the areas of irritation or damage. Therefore, it is necessary to pay special attention to regular hygiene procedures.
Causes of increased sweating
Increased sweating occurs quite often in children. And this condition is not always a sign of any pathological process occurring in the body. However, if a child sweats after an illness in a state of complete rest, then this fact should not be ignored. After all, excessive sweating is a sign of a number of diseases. Many of them are quite serious and require timely treatment.
Also, sweating after illness can be caused by the body's attempts to restore its original balance by getting rid of harmful substances. In this case, this condition is absolutely harmless. Sweating is often caused by external factors. Without knowing about them, parents may not pay attention to them at first. However, after eliminating this cause, it will be possible to cope with the increased work of the sweat glands.
It is important to understand that until the age of five, the sweat glands are not fully formed, while the child’s thermoregulation does not fully function until the child is a month old.
In addition, such elements are present in a much larger volume on a child’s body than on an adult’s. Therefore, increased sweating in children is not always a consequence of some negative impact. But this does not mean that such a sign should be ignored. In any case, if such a problem occurs, you need to show the child to a doctor to make sure there are no pathological processes.
Why is there increased sweating after a drop in temperature?
An increase in temperature during illness is due to the effect on the hypothalamus of immune cells, as well as various pathogenic substances. Fever has a protective function and helps the body fight the disease. When the temperature rises, several important functions begin to take place. It is thanks to them that the body begins to fight the disease.
What happens when the temperature rises:
- In conditions of elevated body temperature, pathogenic microorganisms multiply worse;
- Due to the increase in temperature, phagocytosis and other immune processes are activated;
- Antibodies and other elements important in the fight against diseases begin to be intensively produced by the body.
Thus, it is the increase in temperature that activates all processes in the fight against the disease. Therefore, fever with a cold is quite natural. When pathogenic life forms are “defeated” by the body, the temperature begins to decrease. However, stabilization of the set point cannot occur immediately. This is carried out due to the thermoregulation system, which is represented by the sweat glands. That is, when the temperature drops, the child will produce cold sweat.
Such processes occur not only with a natural decrease in temperature. Increased sweat production will also be observed when taking antipyretic drugs.
Why can antibiotic treatment cause cystitis?
Recurrence of cystitis after treatment with antibiotics is usually familiar to women. In general, females are most often affected by this disease. This is explained by the characteristics of their microflora, as well as the structure of the genitourinary system and genital organs. Unlike men, whose urinary canal is longer, the structure of the female urethra is completely different. This is one of the reasons for infection and the development of inflammation.
The microflora inherent in women is the factor that largely determines the likelihood of various types of diseases. A woman’s health status directly depends on her immunity. If there are any problems or influences on him from the outside, he goes down. Consequently, the necessary protective functions of the body decrease and a favorable environment is created for the proliferation of bacteria and exacerbation of the disease.

Lung diseases and excessive sweating
Excessive sweating is a symptom of most lung diseases. It’s worth talking about them separately because colds often cause complications specifically in this organ. When a child develops signs of ARVI or ARI, it is very important to consult a doctor and not self-medicate. After all, the cause of unpleasant symptoms can be bronchitis, which, if not properly treated, can develop into more serious diseases.
Sweating after an illness can be caused by the fact that bronchitis was “not fully treated” and developed into pneumonia. Of course, in this case, other symptoms are often present in the form of fever, chest pain and a prolonged dry cough. However, in some cases these signs are not observed.
Pneumonia is a very dangerous disease. If left untreated, it can be fatal. Also, lungs affected by pneumonia are more easily infected by other, no less serious bacteria. Another lung disease, a symptom of which is increased sweating at night, is tuberculosis. This disease is caused by the pathogenic Koch bacillus.
Recently, cases of infection with tubercle bacilli in children have become more frequent. This is due to the fact that now the mantoux reaction test is optional and many parents have begun to refuse it.
Symptoms of tuberculosis in the early stages can easily be confused with pneumonia and even bronchitis. In the first stages of its development, only increased sweating, decreased appetite and a slight increase in temperature are observed. There may not be a cough.
Tuberculosis is now successfully treated. However, the sooner the patient addressed this problem to a phthisiatrician, the faster the recovery will occur. Due to the similarity of the symptoms of tuberculosis and pneumonia, children who have had pneumonia are registered at the tuberculosis dispensary. This allows you to completely eliminate the development of pathogenic processes.
In view of the danger of the described complications arising from an untreated cold, it is necessary to carefully monitor the child’s condition after he has recovered. If excessive sweating is observed for more than two weeks, then you need to consult a doctor to undergo the examinations prescribed by him.
Temperature after antibiotics in a child: causes, treatment methods, reviews
When a child becomes ill with a viral infection, he is prescribed a course of treatment with antibiotics. After a few days, the little patient’s condition improves, and the temperature returns to normal. But sometimes after therapy the thermometer creeps up again, and the child develops pain, lethargy and chills.
A low temperature, slightly higher than normal, and accompanying symptoms indicate a normal reaction of the body to the inflammatory process.
After treatment with antibiotics, such consequences are common in medical practice. However, this condition may also indicate a new disease that the prescribed drug cannot cope with.
A laboratory blood test will help resolve this situation.
Peculiarities
A child’s temperature after antibiotics is 37 degrees, indicating that the body is trying to fight the disease on its own. However, this process must be controlled.
For any ailment, especially if it concerns children, you should consult a doctor to determine the cause.
Sometimes parents themselves begin treatment. Such frivolity on their part can lead to undesirable consequences.
If, after taking antibiotics, a child’s temperature rises and does not decrease within several days, this is the result of improper treatment.
Drugs that are prescribed for colds cannot cope with other types of infection, but only worsen the patient’s condition.
Excessive concern
A common reason for a child to have a fever after antibiotics is excessive parental care. They do their best to protect the child from re-infection, mistakenly believing that wrapping him in several clothes will help avoid a new infection or possible complications. Against this background, the baby's temperature may rise.
To exclude pathology, you first need to change him into light clothes and measure his temperature again. Elevated thermometer readings do not always indicate illness.
It is necessary to pay attention to the child's condition. If he has no other painful signs, he is active, plays with toys, then normal overheating is possible and the temperature will return to normal within a short time. Otherwise, you need to see a doctor.
Drug components
Experts believe that some elements included in the drugs penetrate the blood and cause fever. It is characterized by an increase in temperature after antibiotics in a child and the appearance of a rash on the body. In some cases, the normal heart rate decreases. This type of disease can only be determined as a result of the necessary individual studies.
If a child’s temperature rises after antibiotics, but there are no other signs of illness, then you should pay attention to the state of the child’s nervous system.
This reaction of the body is caused by neuroses caused by fatigue and increased nervous excitability. According to doctors, in such situations, walks in the fresh air, vigorous exercise or other physical activity, healthy sleep, and proper rest are recommended.
Effect of antibiotics after therapy
Antibiotics continue to act for 14 days after you stop taking them. Moreover, compared to other drugs, they are slowly eliminated from the body.
Medicines kill a large number of painful microorganisms that enter the blood and infect it with toxic substances. The body reacts to such processes by increasing its temperature. Additional treatment in such cases is not prescribed. The thermometer reading will return to normal after the body is cleansed of toxins.
Allergy
In some cases, treatment with the drugs in question causes allergies. Such consequences do not occur in all patients and are associated with individual intolerance. As a result, the child has a fever again after taking antibiotics, and other symptoms appear in the form of redness of the skin and itching.
In case of such ailment, according to pediatricians, the prescribed drug should be discontinued completely and undergo an antiallergic course of treatment.
Wrong reception
Antibiotics are prescribed to kill infections that cause illness, but are not used to treat symptoms.
If the child has a fever, but the disease is not detected, then the drug has the opposite effect. It does not regulate the temperature, but, on the contrary, helps to raise the thermometer on the second or third day after its use.
Colitis
Antibacterial drugs cause an intestinal disease, which has the medical name “pseudomembranous colitis”.
Associated symptoms are fever, weakness, and vomiting. This disease requires medical treatment and the help of doctors. Otherwise, undesirable consequences in the form of complications are possible.
This disease takes time to develop, so the temperature does not rise immediately.
Kidney problems
Treatment with the drugs in question has a negative effect on the child’s kidneys, causing inflammation and damaging the tissues. In this case, the child’s temperature may persist for a long time after taking antibiotics.
In this case, the child experiences a sleepy state, weakness, nausea, rash, and painful sensations in the muscles. Only a specialist can make a correct diagnosis after conducting a series of studies.
The reasons for an increase in temperature after treatment are very different, therefore the therapy must correspond to the established diagnosis. And for this you need to do all the necessary studies prescribed by the doctor.
Features of therapy
Many practitioners believe that the cause of fever after a course of antibiotics in a child may be an incorrectly chosen treatment method.
An incorrect dosage of a prescribed antimicrobial drug can lead to complications and other diseases that will take a long time to treat.
Only a professional can understand all the intricacies of a viral or bacterial infection, so parents should not treat their child on their own.
Periodic increases and decreases in temperature are one of the most undesirable forecasts. This is how the body can react to complications after a course of therapy with antibacterial medications.
Pediatricians develop a special treatment regimen, which parents often violate as a result of good intentions aimed at a quick recovery of the child. In such cases, pathogenic microbes reduce their activity, but continue to carry out destructive work at a slow pace.
If special studies have not been carried out to determine the body's sensitivity to antibiotics, then its use does not make any sense, except for negative side effects.
Today, many varieties of microorganisms have appeared that are very resistant to the action of antibacterial drugs on them, so their use increasingly does not give the expected effect. In this regard, pediatricians are increasingly replacing previously widely used treatments with other medications that provide better results.
To establish a diagnosis when the temperature rises, the doctor prescribes a study of the composition of the blood, urine, and, if necessary, an x-ray examination. Using ultrasound, it checks the functioning of the heart, intestines, and blood vessels. Determines the body's sensitivity to antimicrobial drugs, takes samples for allergies.
Thus, this once again confirms that it is impossible to determine a child’s disease at home. It is unacceptable to use antibiotics as a prophylactic agent.
This, on the contrary, will lead to weakening of the body, and therefore to the development of the disease.
It is worth noting that antibiotics are prescribed to children only in cases where all other methods of treatment have been tried.
Doctors classify symptoms such as runny nose and cough as acute respiratory diseases, for which the drugs in question are not prescribed. There are other safer antiviral treatments. Antibiotics are used for bacterial infections or fungal diseases and only with a confirmed diagnosis.
Recommendations
Before consulting a doctor, parents are advised to give their children traditional medicine in the form of tea with honey, lemon, raspberries, as well as herbal infusions. Judging by the reviews, after taking antibiotics, parents should start strengthening the child’s body.
To do this, it is necessary to introduce into his diet a diet that helps eliminate toxins. It includes all foods containing fiber, as well as vitamin-rich vegetables and fruits.
In such cases, pediatricians advise giving the child nettle infusions and rosehip infusions.
Intestinal disorders can also be treated at home. They use medication prescribed by the doctor and combine it with home and folk remedies that are indicated for this type of disease. All these methods help restore intestinal microflora, absorb toxic substances, and prevent the removal of water.
To ease the work of the intestines, it is recommended to give children boiled carrots, as well as puree of this vegetable with the addition of potatoes, flour and butter. If the disease is acute, the patient is admitted to a hospital. During the treatment period, children should not be given fried, spicy, a lot of sweets and flour products. Healing mineral waters are recommended to restore the body.
Kidney disease is treated with medications that contain magnesium and calcium. For preventive purposes I use drugs that are made based on natural substances. According to most parents, it is better to exclude foods containing oxalic acid, as well as fats and carbohydrates from the diet. Pediatricians recommend giving the child more water during treatment.
It must be remembered that only a doctor can determine what processes are occurring in the baby’s body, whether they are normal or a disease. And he will also prescribe the correct therapy if a child develops a fever after antibiotics.
Source: https://FB.ru/article/462780/temperatura-posle-antibiotikov-u-rebenka-prichinyi-sposobyi-lecheniya-otzyivyi
Concomitant medical conditions that may cause sweating
Sometimes sweating after an illness is caused by some pathological process occurring in the body that is not related to the previous disease. Therefore, if a child sweats heavily after an illness for a long time, it is very important to consult a doctor in a timely manner.

Possible causes of increased sweating:
- One of the infrequent but probable causes may be a congenital disease such as hyperhidrosis. It usually makes itself felt in the first years of life. The causes of this pathology have not yet been studied.
- Sweating can also cause rickets. This condition occurs as a result of a lack of vitamin D3. At the moment, to prevent this condition, almost every baby is prescribed this vitamin.
- Various nervous disorders can also lead to increased sweating. If a child is constantly experiencing stress or there is a turbulent situation in the family, then this state will be quite natural.
- Another disease that can cause this condition is phenylketonuria. This pathology refers to genetic diseases.
- Cystic fibrosis is a genetic disease that is inherited. With it, the body does not produce protein that interacts with chlorine. And one of the symptoms of this disease is increased sweating.
- Excessive sweating is also characteristic of disruption of the endocrine system. Of course, such problems are not common in children. However, recently cases of diabetes mellitus in children have become more frequent.
- Various viral and bacterial diseases can lead to increased sweating. At the same time, this problem is caused by both re-infection with a cold and AIDS.
- A child may also sweat due to poisoning. In this case, this is a sign of intoxication of the body.
- Apnea is nocturnal cessation of breathing. It may be a sign of other diseases.
Thus, it turns out that the child’s sweating may not be related to the disease. This problem may be a consequence of other diseases that begin to manifest themselves in the body.
Consequences of antibiotic treatment
Many adverse reactions in children are associated with taking antibiotics. The risk of their occurrence is associated with the properties of the drugs and the response of the weakened child’s body to them. For example, penicillins are low-toxic antibiotics and cause less harm. However, in sensitive babies they can cause dysbiosis.
The risk of side effects depends on the duration of drug use, dosage and dosage form.
As a rule, they go away 1-2 weeks after stopping the drugs, but they weaken your health. What consequences should parents be prepared for when taking antibiotics?
Stomatitis
In 25% of cases, stomatitis develops after taking antibiotics. Its mild form is characterized by redness, burning, and swelling of the mucous membrane. As it progresses, red, painful ulcers appear in the mouth and take a long time to heal. Manifestations of stomatitis are possible 1-2 days after starting antibiotics. The drug that caused stomatitis is discontinued and another restoration is prescribed, simultaneously treating stomatitis.
Thrush (candidiasis)
Antibiotics kill bacteria friendly to the body, which inhibit the activity of harmful microorganisms. As a result, favorable conditions for the activity of Candida fungi develop in the baby’s oral cavity. They are insensitive to conventional antibiotics.
At first, the mouth feels dry and burning. Then redness, swelling, white coating on the mucous membrane occurs, and the temperature rises. As soon as the beneficial microflora is renewed, the temperature drops. The success of treatment depends on how quickly a diagnosis is made and recovery is prescribed.
After taking antibacterial drugs, a child may develop thrush
Allergic reaction
Antibiotics are foreign to the child’s body, and an allergic reaction to them can occur at any time. It manifests itself in the form of urticaria, skin itching, rashes, and anaphylactic shock. Negative reactions to antibiotics of the penicillin and cephalosporin group occur especially often. If an allergy is detected, a change in the drug is required under the supervision of a doctor. The reaction is unsafe and can endanger the lives of young patients.
Weakening of the immune system
By destroying beneficial microflora, antibiotics weaken the immune system and provoke the growth of an abnormal number of yeast fungi. At the same time, there is a high risk of them leaving the intestines and penetrating into other systems. The immune system reacts to this and begins to fight microorganisms. Yeast fungi secrete harmful enzymes, which leads to an imbalance in the body.
Intestinal permeability during illness is increased, and toxins easily penetrate into the blood. They provoke allergies even to familiar foods. In the absence of help, autoimmune pathologies arise - Crohn's disease, rheumatoid arthritis, immunodeficiency.
Intestinal infections
Intestinal disorders in children after taking antibiotics are not uncommon. They arise due to disruption of the microflora and stimulation by drugs of active contraction of the intestinal muscles.
Taking antibiotics can cause gastrointestinal upset and problems with bowel movements
Diarrhea occurs especially often after taking Erythromycin. In this case, there is no abdominal pain, slight bloating is observed, and there are no blood clots in the stool. After stopping the antibiotics, the diarrhea goes away, it is necessary to restore the dehydrated body.
Avitaminosis (lack of vitamins)
Antibiotics destroy vitamins B and C and interfere with the absorption of important microelements such as calcium, iron and magnesium. In an organism deprived of these substances for a long time, vitamin deficiency occurs. It manifests itself in pale and dry skin, brittle hair, and muscle weakness. The child loses his bright appearance, becomes nervous and excited, and loses weight. His body is defenseless against viruses.
When to sound the alarm
Sweating can be caused by various factors. These can be natural processes occurring in the body after an illness, external influences or serious illnesses. The last reason is the most dangerous. To understand that the cause is a symptom of a serious illness, you need to pay attention to the accompanying symptoms. They may be different, but some of them are present in almost all cases.
Symptoms indicating that a child is sweating during illness:
- Fever is one of the most common symptoms for most diseases. Moreover, these indicators often increase to only 37-37.2 degrees;
- There is also a high probability that if the child has any disease, his appetite will be reduced. Parents should be wary if the child refuses even his favorite treats;
- Irritability and tearfulness are also common symptoms of many diseases. Therefore, it is important to understand that a child’s whims can be caused not by bad behavior, but by illness;
- We should not ignore the weakness that is characteristic of most diseases. It may be accompanied by dizziness, headaches and nausea.
These symptoms accompany almost all diseases that cause sweating. Of course, these signs may be accompanied by other manifestations characteristic of the existing disease.
Can there be weakness after taking antibiotics?
Any drug, but especially a chemotherapy drug (antibiotic), if not indicated, is contraindicated. 1
V. G. Bochorishvili
The term “antibiotic” itself, literally translated, looks very ominous: “anti” - against, “bio” - life. An opponent of life, in short. But, fortunately, we are not talking about life in general, but about the life of microorganisms in particular.
Penicillin was discovered in 1928. Please note, it is not invented, not invented, but discovered. After all, the whole point is that antibiotics have existed and exist in living nature for as long as nature itself has existed. Certain microorganisms are capable of producing substances that protect them from the damaging effects of other microorganisms. These substances are essentially antibiotics.
His laboratory was small and dark. He never closed the door to it - a typical passage yard. His name was Alexander Fleming. He then became a Nobel laureate and Sir Alexander Fleming.
It was Fleming's penchant for "work disorder" that led to a discovery that would soon shock the world.
Fleming was a bacteriologist. How are bacteria studied? They take a certain medium in which bacteria are supposed to be present (this medium can be anything - soil, water, food, blood, etc.), and place it on a special flat dish with nutrients, where the supposed bacteria should multiply. The bacteria grow and clearly visible points of different sizes form on the cup - colonies of microbes. Colonies are placed on special pieces of glass, painted with special dyes, and then examined under a microscope.
Many end-of-life cups accumulate in the laboratory. One of them turned out to be contaminated with mold. Fleming “only” noticed that the colonies of bacteria (these were staphylococci) around the mold had dissolved - that is, the bacteria had died. The scientist’s conclusion that mold produces a certain substance that can destroy microbes led to the discovery of penicillin.
In the case of the discovery of penicillin, this “producer” of the antibiotic turned out to be a special type of mold. There is “quite a bit” left - to borrow from mold only its inherent weapons, figure out how to create these weapons in quantities adequate to the needs of humanity, and learn to use these weapons.
Since 1943, industrial production of penicillin began. And since that time, antibiotics have become an essential component of modern medicine.
After all, at first glance, the use of these funds looks simple and logical. There is a certain microbe that causes disease. There is a medicine that can destroy the microbe that causes the disease. We prescribe a medicine, destroy the microbe, the disease disappears. Everything is very simple and works out great.
But the more we prescribe and the more we destroy, the more problems appear... Because antibiotics are a very serious weapon. But you need to be able to use serious weapons skillfully.
Hence, it would seem, a completely natural and completely logical conclusion - only a specialist who is properly trained in this matter, in short, a doctor, can use antibiotics. In practice, however, this is not always the case.
People liked the fundamental opportunity to fight infections so much that it is almost impossible to meet a person who has never tried to “crush” any microbe in himself on his own. Any antibiotic will be sold to you in any pharmacy without any prescription. Recently, however, the number of people who like to treat themselves is slowly decreasing due to the general decrease in the solvency of the population, but they do not spare money for children, and they are offended by doctors if they do not prescribe anything serious.
The author does not at all set out to teach readers how to use antibiotics! The task is seen to be:
— once again emphasize the complexity and unsafety of antibiotic therapy;
- pay attention to the obvious: the very fact of prescription, and the dose, and the timing of use, and the direct choice of an antibiotic require the highest professionalism - certain and considerable knowledge, experience, intuition, common sense;
- explain the meaning of some particularly wise medical words that certainly accompany the process of treatment with antibiotics;
— list and insist on mandatory compliance with the rules for the use of antibiotics. Rules that are relevant specifically for those who are treated with antibiotics (knowledge of these rules for those who treat with antibiotics is implied).
Antibiotics are not the only means that can destroy pathogens in the body.
The fundamental possibility of using any antimicrobial drugs is based on the fact that in a certain bacterial cell there are certain structures that have no analogues in the human body. Simply put, it is necessary to find in a microorganism something (a protein, an enzyme) without which it cannot exist, but this “something” must be characteristic of the microbe - that is, there should not be such enzymes or such proteins in a person.
Example: the cell wall of some bacteria has nothing in common in its anatomy with any cells of any mammal. Naturally, it is quite possible (although not at all easy) to create a substance that destroys the bacterial membrane, but does not damage the cells of the human body. By the way, this is exactly how the famous penicillin, ampicillin, and cephalexin act by destroying the bacterial membrane.
Another example: almost all bacteria have an enzyme that has the complex name “DNA gyrase”. Without it, bacteria lose their ability to reproduce and quickly die. Drugs have been created that destroy DNA gyrase and, of course, have a pronounced antibacterial effect on many bacteria - norfloxacin, ofloxacin, etc.
But the drugs listed are not antibiotics!
This state of affairs is not very clear and requires explanation.
I emphasize once again: antibiotics are substances that some microorganisms produce to destroy other microorganisms.
Some fungi (penicillium, cephalosporium, etc.) produce antibiotics - for example, penicillin, cephalosporin. Some bacteria (actinomycetes) produce antibiotics - for example, tetracycline, streptomycin.
Scientists try to modernize any natural antibiotic (change, improve, make it more active against microbes and less dangerous for humans). Thus, by changing the structure of penicillin, its synthetic derivatives were obtained - oxacillin, ampicillin; by changing tetracycline - doxycycline, metacycline, etc. Thus, antibiotics are natural and synthetic.
At the same time, an antimicrobial agent may have nothing to do with living nature - it may be a product exclusively of the human mind, that is, it may be a substance that a person invented himself. You have, of course, heard about many of these drugs. These are the famous sulfonamides (streptocide, etazol, biseptol), nitrofurans (furazolidone, furagin), fluoroquinolones (we have already named norfloxacin, ofloxacin, etc.).
The point of the above: antibacterial agents and antibiotics are not the same thing.
There is such a term in medicine - “chemotherapy”. Chemotherapy is the treatment of infectious diseases with drugs. And all the drugs we have listed - sulfonamides, antibiotics, fluoroquinolones, and nitrofurans - are chemotherapeutic agents, or, more understandably, antimicrobial agents.
The information provided is of more theoretical than practical importance, since the principles and rules for the use of any antimicrobial agents are the same. Everything that we tell about antibiotics will equally apply to fans of biseptol and fans of furazolidone, and to all other fans of fighting microbes.
Antibiotics are different, and this is quite obvious. But, using a completely specific antibiotic in each specific case, doctors (I repeat once again, it is doctors) proceed from the completely specific properties of a particular drug. What are these properties?
ANTIBIOTIC ACTION SPECTRUM
Each antibiotic acts on strictly defined microorganisms. For example, penicillin actively acts on the so-called cocci - streptococcus, meningococcus, gonococcus, pneumococcus, but does not act on E. coli, dysentery bacillus, and salmonella. The antibiotic polymyxin, on the contrary, acts on rods, but does not act on cocci. Levomycetin and ampicillin act on both the former and the latter. That is, the spectrum of action of chloramphenicol is wider than the spectrum of action of penicillin. Hence the obvious concepts of “ broad-spectrum antibiotic ” and “ narrow-spectrum antibiotic ”.
Is a broad-spectrum antibiotic good or bad? On the one hand, it’s very good, because if the causative agent of the disease is not known (well, it’s just not clear who caused a specific meningitis, or a specific pneumonia), the use of a broad-spectrum antibiotic is more likely to be effective. On the other hand, such an antibiotic will destroy not only the causative agent of the disease, but also “peaceful” intestinal microbes, which will manifest itself in the form of dysbiosis. Hence the obvious conclusion is that narrow-spectrum antibiotics (penicillin, oxacillin, erythromycin) are more preferable than broad-spectrum antibiotics (ampicillin, gentamicin, tetracycline, chloramphenicol). But it is more difficult for a doctor to treat with narrow-spectrum drugs - it is easier not to guess, not to get in, not to help and, in the end, to be guilty.
MECHANISM OF ANTIBIOTIC ACTION
Some antibiotics completely inhibit the growth of bacteria, that is, they destroy them irreversibly. Such antibiotics are called bactericidal ; they act on very important cellular structures, destroying microbes quickly and in huge quantities. Penicillin destroys the membrane of the bacterium, and the latter has no chance of existence. It is clear that penicillin is a bactericidal antibiotic, as are ampicillin, cephalexin, and gentamicin.
Some antibiotics act completely differently - they prevent the growth of bacteria. The colony of microorganisms does not increase; the bacteria, on the one hand, die on their own (“from old age”), on the other hand, they are actively destroyed by immune cells (leukocytes) and the person quickly recovers. Such antibiotics - they are called bacteriostatic - seem to help the body overcome the infection itself. Examples are erythromycin, tetracycline, chloramphenicol.
If you stop taking a bacteriostatic antibiotic early, the disease will definitely return. The effect of the bactericidal drug will come faster.
DISTRIBUTION OF ANTIBIOTIC IN THE BODY
No matter how the antibiotic enters the body, it eventually ends up in the blood and spreads throughout the body. In this case, in a certain organ, a certain antibiotic accumulates in a very specific amount.
Otitis media can be treated with both penicillin and ampicillin, but ampicillin accumulates better in the middle ear cavity and therefore will be more effective. The antibiotic lincomycin penetrates well into the bones and is used to treat osteomyelitis (purulent inflammation of the bones). The swallowed antibiotic polymyxin is not absorbed into the blood at all and acts only in the intestines - convenient for the treatment of intestinal infections.
The distribution of some modern drugs in the body is generally unique. For example, the antibiotic azithromycin attaches in a special way to phagocytes—immune cells that engulf and digest bacteria. When a focus of inflammation occurs in the body, phagocytes move exactly there and accumulate in huge quantities in the inflammatory focus. Azithromycin moves along with phagocytes - that is, in the presence of pneumonia, the maximum amount of antibiotic will be in the lungs, and in case of pyelonephritis - in the kidneys.
WAYS FOR ADMINISTRATION OF ANTIBIOTIC INTO THE BODY
There are different ways to “direct” an antibiotic to places where microbes accumulate. You can apply antibiotic ointment to the abscess on the skin. Can be swallowed (tablets, drops, capsules, syrups). You can inject - into a muscle, into a vein, into the spinal canal.
The route of administration of the antibiotic is not of fundamental importance - it is only important that the antibiotic is in the right place and in the right quantity on time. This is, so to speak, a strategic goal. But the tactical question - how to achieve this - is no less important.
Obviously, any tablets are clearly more convenient than injections. But... Some antibiotics are destroyed in the stomach, for example penicillin. Others are not absorbed or hardly absorbed from the intestine, such as gentamicin. The patient may vomit or be completely unconscious. The effect of a medicine swallowed will occur later than from the same medicine administered intravenously - it is clear that the more severe the disease, the more reasons for unpleasant injections.
WAYS TO REMOVE ANTIBIOTICS FROM THE BODY
Some antibiotics, such as penicillin or gentamicin, are excreted unchanged from the body in the urine. This allows, on the one hand, to successfully treat diseases of the kidneys and urinary tract, but on the other hand, if there is a significant disruption of the kidneys, and with a decrease in the amount of urine, it can lead to excessive accumulation of the antibiotic in the body (overdose).
Other drugs, such as tetracycline or rifampicin, are excreted not only in the urine, but also in the bile. Again, the effectiveness in diseases of the liver and biliary tract is obvious, but special caution is needed in case of liver failure.
SIDE EVENTS
There are no medications without side effects. Antibiotics are no exception, to put it mildly.
Allergic reactions are possible. Some drugs cause allergies often, such as penicillin or cephalexin, while others rarely, such as erythromycin or gentamicin.
Certain antibiotics have a damaging (toxic) effect on some organs. Gentamicin - on the kidneys and auditory nerve, tetracycline - on the liver, polymyxin - on the nervous system, chloramphenicol - on the hematopoietic system, etc. After taking erythromycin, nausea and vomiting often occur, large doses of chloramphenicol cause hallucinations and decreased visual acuity, any antibiotics broad spectrum of action contribute to the development of dysbacteriosis...
***
Now let's think about it!
On the one hand, the following is obvious: taking any antimicrobial agent requires mandatory knowledge of everything that was listed above. That is, all the pros and cons must be well known, otherwise the consequences of treatment can be the most unpredictable.
But on the other hand, when you swallowed Biseptol on your own, or, on the advice of a neighbor, when you put an ampicillin tablet into your child, were you aware of your actions? Did you know all this?
Of course they didn't know. They didn’t know, didn’t think, didn’t suspect, wanted what was best...
It’s better to know and think...
***
What you need to know
— Any antimicrobial agent should be prescribed only by a doctor!
- It is unacceptable to use antibacterial drugs for viral infections, supposedly for the purpose of prevention - in order to prevent the development of complications. This never works out; on the contrary, it only gets worse. Firstly, because there is always a microbe that will survive. Secondly, because by destroying some bacteria, we create conditions for the proliferation of others, increasing, rather than decreasing, the likelihood of the same complications. In short, an antibiotic should be prescribed when a bacterial infection is already present, and not to supposedly prevent it. The most correct attitude to preventive antibiotic therapy is contained in the slogan put forward by the brilliant philosopher M. M. Zhvanetsky: “Troubles must be experienced as they arise!”
Prophylactic antibiotic therapy is not always evil. After many operations, especially on the abdominal organs, it is vital. During a plague epidemic, massive intake of tetracycline can protect against infection. It is only important not to confuse concepts such as prophylactic antibiotic therapy in general and the prophylactic use of antibiotics for viral infections in particular.
— If you are giving (taking) antibiotics, under no circumstances stop treatment immediately after you feel a little better. Only a doctor can determine the required duration of treatment.
— Never beg for something stronger.
The concept of the strength and weakness of an antibiotic is largely arbitrary. For our average compatriot, the power of an antibiotic is largely related to its ability to empty pockets and purses. People really want to believe in the fact that if, for example, thienam is 1000 times more expensive than penicillin, then it is a thousand times more effective. It wasn’t like that...
In antibiotic therapy there is such a thing as “ antibiotic of choice ”. That is, for each infection, for each specific bacteria, an antibiotic is recommended that should be used first - it is called the antibiotic of choice. If this is not possible - for example, allergies - second-line antibiotics are recommended, etc. Sore throat - penicillin, otitis media - amoxicillin, typhoid fever - chloramphenicol, whooping cough - erythromycin, plague - tetracycline, etc.
All very expensive drugs are used only in very serious and, fortunately, not very frequent situations, when a specific disease is caused by a microbe that is resistant to the action of most antibiotics, when there is a pronounced decrease in immunity.
— When prescribing any antibiotic, a doctor cannot predict all possible consequences. There are cases of individual intolerance to a particular drug by a particular person. If this happened, and after taking one erythromycin tablet the child vomited all night and complained of abdominal pain, then the doctor is not to blame. Pneumonia can be treated with hundreds of different drugs. And the less often an antibiotic is used, the wider the spectrum of its action and, accordingly, the higher the price, the greater the likelihood that it will help. But the greater the likelihood of toxic reactions, dysbacteriosis, and immunosuppression. Injections are more likely and will lead to recovery faster. But it hurts, but suppuration is possible in the place where it was injected. And if you have an allergy, after the pill you rinsed your stomach, and after the injection, what should you rinse? The patient's relatives and the doctor must find a common language . Using antibiotics, the doctor always has the opportunity to play it safe - injections instead of tablets, 6 times a day instead of 4, cephalexin instead of penicillin, 10 days instead of 7... But the golden mean, the correspondence between the risk of failure and the likelihood of a quick recovery is largely determined by the behavior of the patient and his relatives. Who is to blame if the antibiotic doesn't help? Is it really just a doctor? What kind of organism is this that, even with the help of the strongest drugs, cannot cope with an infection! This is the kind of lifestyle that had to be organized in order to take immunity to the extreme... And I don’t want to say at all that all doctors are angels - their mistakes, unfortunately, are not uncommon. But it is necessary to shift the emphasis, because for a specific patient nothing answers the question “who is to blame?” The question “what to do?” - always more relevant. But all the time:
- “We should have prescribed injections!”;
- “Don’t you know any other medicine besides penicillin?”;
- “What does expensive mean, we don’t feel sorry for anything for Mashenka!”;
- “Do you, doctor, guarantee that this will help?”;
- “You change the antibiotic for the third time, but you still can’t cure an ordinary sore throat!”
v The boy Sasha has bronchitis. The doctor prescribed ampicillin, 5 days passed, and things improved significantly. After 2 months, another illness, all the symptoms are exactly the same - bronchitis again. I have personal experience: ampicillin helps with this disease. Let's not bother the pediatrician. We will swallow proven and effective ampicillin. The situation described is very typical. But its consequences are unpredictable. The fact is that any antibiotic is capable of combining with blood serum proteins and, under certain circumstances, becoming an antigen - that is, causing the production of antibodies. After taking ampicillin (or any other drug), antibodies to ampicillin may be present in the blood. In this case, there is a high probability of developing allergic reactions, sometimes very (!) severe. In this case, an allergy is possible not only to ampicillin, but also to any other antibiotic similar in its chemical structure (oxacillin, penicillin, cephalosporin). Any repeated use of an antibiotic greatly increases the risk of allergic reactions . There is another important aspect. If the same disease recurs after a short time, then it is quite logical to assume that when it reoccurs, it (the disease) is associated with those microbes that “survived” after the first course of antibiotic therapy, and therefore, the antibiotic used will not be effective.
— A corollary of the previous point. The doctor cannot choose the right antibiotic if he does not have information about when, for what, what medications and in what doses your child received. Parents should definitely have this information! Write down! Pay special attention to any manifestations of allergies.
- Do not try to adjust the dose of the drug . Antibiotics in small doses are very dangerous because there is a high probability of the emergence of resistant bacteria. And if it seems to you that “2 tablets 4 times a day” is a lot, and “1 tablet 3 times a day” is just right, then it is quite possible that you will soon need 1 injection 4 times a day.
— Do not part with your doctor until you clearly understand the rules for taking a particular drug. Erythromycin, oxacillin, chloramphenicol - before meals, take ampicillin and cephalexin - anytime, tetracycline cannot be taken with milk... Doxycycline - 1 time per day, biseptol - 2 times per day, tetracycline - 3 times per day, cephalexin - 4 times per day...
***
Once again about the most important thing.
Millions of people owe their lives and health to antibiotics. But:
Between the antibiotic and the person, there must be the most important intermediate link: the DOCTOR who treats the person with the antibiotic.
1 You will probably be able to fully appreciate the meaning of this quote only after familiarizing yourself with the contents of the chapter. As for its author, Professor V.G. Bochorishvili is a true professional and specialist in the field of antibiotic treatment, in the recent past the director of a clinic that treated sepsis (blood poisoning).
2Concerning prophylactic antibiotic therapy
What measures can be taken to prevent a child from sweating?
If a child is sweating, then this alarming sign should not be ignored. Especially if excessive sweating occurs in a calm state and is present for more than two weeks after recovery. If you experience excessive sweating, you should visit a doctor. In the case of children, first of all, you need to contact a pediatrician.
The specialist will examine the baby and get acquainted with his medical history. Next, blood and urine tests will be prescribed to help identify inflammation and other negative factors. Depending on the results of the initial examination and tests, the doctor will refer the child to a specialist or prescribe instrumental testing. After this, a diagnosis will be made.
If sweating is caused by an illness, then it must be treated by listening to the doctor’s recommendations. In this case, therapy is prescribed depending on the individual characteristics of the child, as well as the specifics of the pathology.
In the case when the doctor does not identify any diseases that can cause sweating, it is necessary to take a closer look at external factors. Perhaps they were the cause of the child’s sweating.
How do antibiotics work?
Antibiotics are effective for diseases caused by bacteria, not viruses. Bacteria are single-celled microorganisms several thousandths of a millimeter in size. They are divided into dangerous and harmful, causing otitis media, skin inflammation, throat and urinary tract infections.
Antibiotics are prescribed to children in the form of tablets, injections, suspensions, drops or ointments. They enter the site of inflammation and affect bacteria in different ways:
- bactericidal (penicillin, cephalosporin) kill bacteria;
- bacteriostatic (erythromycin, tetracycline) block the activity and proliferation of bacteria and have a positive effect on the immune system.
It is impossible to determine which microorganisms cause a child’s illness on your own. For this reason, parents should not give antibiotics to their children unless prescribed by a doctor. They are also never used as a preventive measure.
Elimination of negative factors
If the cause of sweating is not a disease, then it is quite possible that the problem lies in external factors. In this case, parents should follow a few tips to help solve it.
Prevention of child sweating and elimination of factors that contribute to this:
- First of all, it is necessary to normalize the temperature and humidity in the room. In summer, regular ventilation will help with this. In winter, it is necessary to set the heating temperature correctly and also use a humidifier;
- It is also important to dress your child correctly. Don't wrap him up too tightly. It is also advisable to purchase clothes made from natural fabrics. In summer it is not recommended to use warm blankets;
- Maintaining hygiene is also important. The baby must take cleansing procedures daily. It is also important to change your underwear every day. The bed must be changed at least once a week;
- It is necessary to normalize the child's diet. Nutrition should be balanced. The baby should receive a daily dose of vitamins, minerals and other beneficial microelements. You need to avoid harmful foods.
If a child sweats at night, this does not mean that he is seriously ill. However, this sign should make parents wary. After all, it can also be a symptom of various diseases. Be attentive to your children and they will be healthy.
Causes of excessive sweating after illness

With colds, acute respiratory viral infections, which are accompanied by elevated temperature, profuse sweating occurs, especially at night. This is a protective reaction of the body. The baby experiences weakness and fatigue.
It is considered normal if a child sweats during illness and for 1-2 weeks after a viral illness, since the body had to produce a lot of fluid when fighting an elevated temperature and it needs time to stop this process.
In addition, a physiological feature of children is thermoregulation, to a greater extent, not so much with the skin, as in adults, but with the lungs. But if a child is lethargic for a long time, feels weak, sweats during sleep, this may be evidence of a low-grade inflammatory process in the body.
Untreated cold

If the baby sweats heavily during sleep after an acute respiratory viral infection for a long time, this may be associated with the development of pathology. Pathological processes can be aggravated by serious complications if treatment is started at the wrong time.
Particular attention should be paid to infants: due to their anatomical characteristics and imperfect physiological development, they more often encounter complications after suffering from acute respiratory viral infections, when a bacterial infection can join a viral infection.
Also, repeated inflammatory processes in the body can be facilitated by premature stress on your baby’s body, which needs time to remove toxins, waste products of viruses and complete recovery. Therefore, you should not endanger a child who is not sufficiently strong after an illness and immediately take him to a children’s group, where there is too high a risk of new infections.
Pneumonia
The child sweats a lot after suffering from a viral illness, which results in a dry, prolonged cough, chest pain, shortness of breath, and increased body temperature at night.
It is very important not to miss these dangerous symptoms, because they may indicate the development of pneumonia, which requires immediate medical treatment.
sweating after pneumonia
I am 28 years old. at the time of illness I weighed 45 kg (this was my stable normal weight) with a height of 168 cm. Now I weigh 50 kg. I try to eat more. in November 2012 she was treated for pneumonia, but to no avail. Infiltrative tuberculosis of the lower lobe of the right lung was detected. She was treated first with isocomb, then with lomecomb, then ethambutol, rifampicin, isoniazid, and pyrazinamide were prescribed separately. I’ve been receiving treatment like this, without missing anything, for five and a half months now, on an outpatient basis. no drug resistance was detected. bk alternately minus and plus, at the beginning of treatment 50 colonies were sown. I would like to know what this means? is it a lot or a little? How serious was the process I had (and still am)? but my main question is about the tomogram. My TB doctor sent me for a tomogram in April because... BK was found in the sputum, and she said this shouldn’t happen, she suspected a lesion in the bronchus. Here are the results of multispiral TM: in spiral mode (with primary collimation 16X1 mm with slice thickness 1mm, 3-dimensional image processing MPR, MIP) the study was carried out. lungs, mediastinum. No bone destructive changes were detected. The lung parenchyma is of normal airiness, without additional fields of pathological changes, with the exception of C-6 on the right, where against the background of local pneumosclerosis a focal shadow of up to 12.5 mm to 62 units of N is visualized, around there are polymorphic foci from 3-4 mm to 7 mm. No decay cavities are identified. The bronchi can be traced to subsegments of normal caliber. The sinuses are free. There is no effusion in the pleural cavities. The diaphragm is located at the usual level. There are no additional formations or enlarged lymph nodes in the mediastinum. Conclusion: During the period of treatment and observation, the formation of tuberculoma in C-6 on the right in f. contamination. Consultation with a thoracic surgeon. CT scans https://www.sendspace.com/file/0tmbj2 tell me what this result means after 5 months of treatment? What should I expect with such dynamics? What else can I do besides continue to take the pills as an outpatient? The thing is that my doctor wants to stop me from ethambutol and pyrazinamide, leaving only 2 drugs. Tell me, is this justified? Will this make me feel worse? and a few more questions. In February I completed a course of laser therapy and went to the Milta device. the feeling was good. and then in April my TB doctor prescribed electrophoresis with theosulfate. I went 3 times and problems started - coughing (although I haven’t coughed since November), shortness of breath, heaviness under my right shoulder blade, sweating. I stopped walking and the cough went away. Can the condition worsen from electrophoresis and how dangerous is it? I have doubts about the competence of my doctor. She doesn’t explain or tell anything about the operation, I have absolutely no idea what the prognosis and prospects are. she just asked me “don’t you want to have surgery?” but how can I make such a responsible decision myself, knowing practically nothing about my condition. I still have discomfort under my right shoulder blade, sometimes I sweat at night - but not every night, as if in periods. My skin became very oily. Tell me, has my treatment been adequate all this time and what are the prospects for developments in my case?
Diagnostics

When your baby sweats heavily after pneumonia for more than 1-2 weeks and other symptoms of the inflammatory process appear, a visit to the doctor should not be postponed. After all, this can lead not only to the development of the disease into a chronic form, but even to death. During the examination, the pediatrician must determine the cause and prescribe appropriate treatment.
The reasons can be completely different:
- infection with viruses and bacteria;
- avitaminosis;
- lack of certain microelements;
- rickets;
- heart failure;
- disruption of the autonomic nervous system;
- severe genetic diseases (phenylketonuria, cystic fibrosis);
- diabetes;
- asthma.
You should consult a doctor at the slightest suspicion of health problems. It is better for the worries to be in vain than to miss the initial stage of the development of any disease.
Treatment

Sweating in your baby after an illness is associated with a large expenditure of energy to fight infection and eliminate toxins. To help him cope with clearing infections, doctors recommend special medications and procedures that provoke profuse sweating.
The air the baby breathes plays an important role. A dry room in the presence of inflammation of the respiratory tract causes impaired ventilation of the lungs.
Restoring strength and increasing immunity after illness in a shorter time, getting rid of possible residual effects is facilitated by:
- absence of physical and nervous overload;
- complete rest;
- balanced diet.
Tips and tricks

If there are no serious health problems, and the child sweats after fever for a long time, doctors advise:
- Review your child's daily routine - hyperactive children who run around during the day become very overexcited. Therefore, quiet games and reading books are preferable before bed.
- Calming herbal teas - tea with chamomile, motherwort, valerian, mint, fennel, linden, calendula or lemon balm will calm the nervous system, relieve anxiety and promote easy sleep.
- Selection of bedding - incorrect selection can cause children to sweat greatly during sleep. The material should be natural and hypoallergenic, it should be selected according to the season (terry cotton, flannel are suitable for winter; chintz, satin, calico are suitable for summer).
- Evening bathing - after a cool shower taken before bed, the baby falls asleep better and sweats less during sleep.
- Temperature and air humidity - it is recommended that the nursery have moderately humidified air no more than 20 degrees.
- Taking vitamins and walking in the fresh air - their benefits in the fight against hyperhidrosis against the background of a previous illness can hardly be overestimated.
Was the article helpful?
Rate the material on a five-point scale!
If you have any questions or want to share your opinion or experience, write a comment below.
Source










