Abdominal pain (in the abdomen) is quite common in both adults and children. Many people try to associate them with some food or drink consumed the day before. This reason for the development of events also occurs, but not always.
Abdominal pain can also be caused by more serious factors. One of them is that the lymph nodes in the abdominal cavity are enlarged. In children and adults, the symptoms of this pathology are approximately the same. The difference is that a small patient sometimes cannot explain clearly enough what is wrong with him. Concerned parents may attribute his complaints of abdominal pain to a dozen reasons that have no place in this case. Some even begin to self-medicate, thereby aggravating the baby’s condition.
Lymph nodes
First, let's take a brief overview of these small but very important organs. The lymph node is a natural filter that helps get rid of all kinds of pathogenic agents that have entered the body.
Its structure is quite complex. In general terms, a lymph node is a small (up to 50 mm maximum) round, bean-shaped or oval-shaped sac, to which lymph vessels (several incoming and one outgoing) are suitable. The outside of the “bag” is covered with a membrane consisting of connective tissue. Inside it is filled with the so-called stroma, made up of reticular fibers. A large number of lymphocytes of various types are concentrated in the space between them.
Lymph, slowly seeping through the reticular fibers, as if through a sieve, is cleared of all sorts of pathogenic agents that it has “collected” in the body (bacteria, viruses, protozoa, and so on). If a person has any disease, too many harmful elements enter the lymph. The lymph nodes can no longer cope with their task and become inflamed. This symptom always indicates the presence of some pathogenic process in the body.
While examining the patient, the doctor discovers that his lymph nodes are enlarged. In the abdominal cavity of a child and an adult, there are about 600 of them. They are located not one by one, but in groups, vaguely similar to a bunch of grapes. Lymph nodes are concentrated in the peritoneum where blood and lymph vessels pass - near the stomach, liver, spleen, mesentery, intestines.
Causes of inflammation
Based on the above, you can easily understand why the lymph nodes in the abdominal cavity of a child are enlarged. In general, this condition is called lymphadenopathy, and inflammation of the lymph nodes specifically in the mesentery is called mesadenitis. It is caused by the following reasons:
- Any bacterial infection (streptococci, staphylococci, salmonella, tuberculosis, E. coli).
- Any viral infection (enterovirus, herpes).
- Worm infestation.
- Fungal infection.
- In rare cases, toxic poisoning.
Pathogenic elements enter the lymph nodes with blood, lymph, and also through the lumen of the tract (worms).

Sometimes the infection seeps into the tissue of the lymph nodes directly from the intestines.
What diseases cause mesadenitis?
Most often, a child's lymph nodes in the abdominal cavity are enlarged due to the development of diseases in the organs near which they are located. Among them:
- Helminthiases.
- Brucellosis.
- Hepatitis.
- Trichinosis.
- Ascariasis.
- Echinococcosis.
- Salmonellosis.
- Mononucleosis.
But often the lymph nodes in the child’s abdominal cavity are enlarged due to infectious diseases not related to the gastrointestinal tract. Among them:
- Flu.
- ARVI.
- Tuberculosis.
- Pneumonia.
- Herpes.
- Lupus erythematosus.
The following can also cause enlargement of lymph nodes in the peritoneum:
- AIDS.
- Syphilis.
- Malignant formations (metastasis in the gastrointestinal tract).
These ailments are mainly observed in adults, but they also occur in children.
Indications and contraindications for ultrasound of lymph nodes in children
Each age category of children has different norms for the size of lymph nodes. They are sent for an ultrasound if they are larger than the standard and/or show signs of pathology. These are soreness, redness of the skin, an increase in local/general temperature, tissue inflammation, thickening, and other changes.
Some medications cause enlarged lymph nodes. During the examination, the doctor lists all the drugs used.
Ultrasound of lymph nodes is also performed when enlarged without symptoms of the disease. The child is observed without an emergency examination if he has had an acute respiratory viral infection, tonsillitis, or other viral, fungal or bacterial infection. Sonography is performed if they have not decreased within 2 weeks.
Indications for ultrasound examination of lymph nodes in children:
- suspicion of cancer of the lymphatic system or metastasis in areas near the enlarged lymph node;
- chronic headache;
- frequent apathy, nervousness;
- causeless weakness, drowsiness;
- fatigue;
- decreased academic performance, attention, memory;
- loss of appetite;
- insomnia, other sleep disorders;
- chronic infectious and inflammatory diseases;
- pain of unknown etiology;
- suspicion of systemic diseases;
- deformation of the bone, jaw, spine;
- local proliferation of soft or connective tissue (in one area);
- suspected tuberculosis, HIV or latent infection.
There are no age restrictions for sonography: ultrasound diagnostics are performed from the moment of birth. An emergency examination is performed on the day of seeking medical help.
A planned ultrasound is postponed until the condition normalizes in case of acute inflammation of the lymph node, eczema, pyoderma and skin damage in the examined area. Sonography of internal nodes is also not done in the first 5 days after X-rays with contrast, FGDS, or laparoscopy.
To watch Dr. Komarovsky’s program on the topic:
Classifications
A disease in which the lymph nodes in the child’s abdomen are enlarged can occur suddenly or last for years. Depending on the nature of the flow, the following forms are distinguished:
- Spicy.
- Chronic.
Depending on the number of enlarged lymph nodes, the following forms are distinguished:
- Local (affects one node).
- Regional (more than one lymph node is enlarged).
- Generalized (the entire peritoneum is affected).
Based on etiology, the following forms are distinguished:
- Primary (occurs as an independent disease).
- Secondary (occurs against the background of infections in the gastrointestinal tract, respiratory tract and others).

Types of lymphadenitis
Depending on the nature and duration of the disease, all lymphadenitis can be divided into subtypes:
- chronic;
- spicy.
Lymphadenitis can also be:
- Isolated – 1 lymph node is inflamed.
- Regional - the inflammatory process affects a group of neighboring lymph nodes.
- Total – lymphadenitis spread throughout the body.
The course of the disease is divided into specific and nonspecific: the first type includes inflammation as a result of tuberculosis, AIDS, toxoplasmosis or tumors, the second type includes all other types of lymphadenitis.
According to the International Classification of Diseases, better known as ICD-10, lymphadenitis is divided into groups according to location. They relate to diseases of the skin and subcutaneous tissue (ICD-10 code - L04), as well as diseases of the circulatory system (code - I88).
Acute lymphadenitis of the neck, head and face (L04.0)
About a third of the lymph nodes in the human body are localized in the head and neck area, which belong to group L04.0:
- submandibular;
- occipital;
- cervical;
- preauricular.
Inflammation of these lymph nodes occurs after tonsillitis and other bacterial diseases of the respiratory tract, with herpes, influenza and ARVI, due to dental diseases and inflammatory processes in the mouth. Lymphadenitis can also occur due to untreated wounds in the neck, face and cheeks. Another reason is infectious skin diseases.
Symptoms of lymphadenitis in this group include pain and discomfort in the affected area, difficulty swallowing, and fever in children. Lymphadenitis on the back of the head, behind the ears and under the chin is also visually noticeable: small spherical seals stand out on the skin and hurt when touched. You can see what the disease code L04.0 looks like in the photo.

Inflammation of the lymph node in the neck
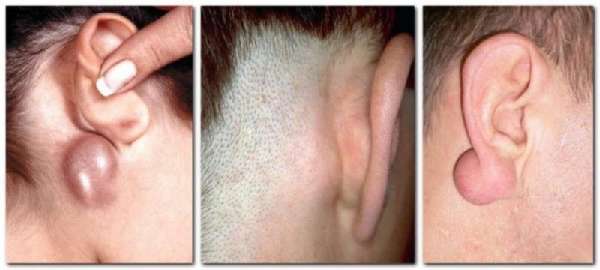
Inflammation of the lymph node in the neck
Inflammation of the lymph nodes behind the ears

Inflamed lymph node behind the ear
Acute lymphadenitis of the trunk (L04.1)
This group includes inflammation of the lymph nodes of the body, which are located in the abdominal and thoracic region.
These include:
- abdominal or mesenteric lymph nodes;
- retrocrural lymph nodes;
- paraortic, paracaval lymph nodes;
- supraclavicular and subclavian lymph nodes.

Inflammation of the lymph node in the chest area
This location of lymphadenitis may indicate viral and bacterial infections, as well as a specific type of disease resulting from tuberculosis, HIV infection, oncology of the abdominal and thoracic region.
Symptoms of the disease include severe chest or abdominal pain, increased body temperature, lethargy, and loss of appetite.
Acute lymphadenitis of the upper limb (L04.2)
Lymphadenitis of the upper limb includes inflammation of the lymph nodes of the elbow and armpit. Most often, the lymph node is enlarged on one side and visually appears as a swollen, reddish lump.
Axillary and ulnar lymphadenitis occurs due to infections of various etiologies:
- tonsillitis, tonsillitis, laryngitis and other bacterial diseases;
- influenza and herpes, ARVI;
- inflammatory diseases of the oral cavity;
- infected wounds and abrasions in the armpit, chest and arms.

Inflammation of the lymph node of the elbow
Also, inflammation of the lymph nodes in the axillary region can indicate mastopathy and mastitis that occur after childbirth and during feeding. In this case, the symptom manifests itself before menstruation, 2-3 days before the start of menstruation, and goes away on its own after a week.
Signs of the disease, in addition to noticeable swelling of the lymph node, include pain and discomfort in this area, possible itching, and fever.
Acute lymphadenitis of the lower limb (L04.3)
Lymphadenitis of the lower extremity includes inflammation of the inguinal and popliteal lymph nodes. They can develop as a result of inflammation of the soft tissues of the legs, from hypothermia, due to wounds and abrasions, infected calluses and uncomfortable shoes.
Also, the causes of inguinal lymphadenitis include diseases of the genital organs:
- urethritis;
- prostatitis;
- vaginitis;
- gonorrhea;
- chlamydia.

Inflammation of the inguinal lymph node
Most often, inflammation of the lymph nodes of this group occurs in adults.
Acute lymphadenitis of the lower extremities is accompanied by severe pain at the site of inflammation, discomfort, noticeable compaction and swelling of the lymph node.
Nonspecific mesenteric lymphadenitis (I88.0)
Nonspecific mesenteric lymphadenitis is an inflammation of the mesenteric lymph nodes resulting from a bacterial or viral infection.
The causative agents of mesadenitis include:
- streptococci and staphylococci;
- enteroviruses;
- salmonella;
- mononucleosis.

Inflammation of the inguinal lymph node
Most often, inflammation of the lymph nodes of this group occurs in adults.
Acute lymphadenitis of the lower extremities is accompanied by severe pain at the site of inflammation, discomfort, noticeable compaction and swelling of the lymph node.
Nonspecific mesenteric lymphadenitis (I88.0)
Nonspecific mesenteric lymphadenitis is an inflammation of the mesenteric lymph nodes resulting from a bacterial or viral infection.
The causative agents of mesadenitis include:
- streptococci and staphylococci;
- enteroviruses;
- salmonella;
- mononucleosis.
With nonspecific mesenteric lymphadenitis, the stomach hurts severely
The disease is characterized by severe abdominal pain, fever, vomiting and nausea. Disorders of stool and gastrointestinal functioning are also often observed: diarrhea, constipation, hiccups.
Chronic lymphadenitis (I88.1)
Chronic lymphadenitis is an inflammation of the lymph nodes that occurs over a long period of time. It can be unilateral or bilateral, specific or nonspecific, and localized in different parts of the body.
The chronic course of the disease may be due to:
- complications of tonsillitis, bronchitis and tonsillitis;
- purulent boils and ulcers on the body;
- oral infections;
- fungal infections;
- tuberculosis;
- AIDS and HIV infection.

With chronic lymphadenitis, pain decreases
As in the case of acute lymphadenitis, the disease is accompanied by thickening and enlargement of the lymph nodes. At the same time, a swollen and hard lymph node practically does not hurt and remains mobile. Other symptoms, such as fever, redness, pain and weakness, are also less pronounced.
Enlarged lymph nodes in the abdominal cavity in a child: symptoms
In children, the acute form of the pathology is more often diagnosed. It is characterized by a violent manifestation. Its manifestations are as follows:
- A sharp increase in temperature.
- Complaints of abdominal pain (paroxysmal, acute, localized or vague).
- Children's anxiety, tearfulness, moodiness.
- Vomit.
- Complaints of nausea.
- Diarrhea (this symptom often makes parents think that the child has eaten something wrong).
- Palpation of enlarged lymph nodes.
In the chronic form, all these symptoms are less pronounced. Also, with a long course of the disease, in which the child has enlarged lymph nodes in the abdominal cavity, the stomach hurts in the navel area or the pain spreads to the lower sections. Sometimes children have difficulty explaining exactly where it hurts, since the unpleasant sensations are vague and palpable throughout the entire abdominal area.
Why do mesenteric lymph nodes enlarge in children: mesenteric inflammation
Mesadenitis is a fairly common condition in children that causes pain in the abdomen. In many cases, the problem resolves without treatment. It can sometimes be difficult to diagnose because the symptoms are similar to appendicitis. Mesadenitis means inflammation of the lymph nodes of the abdominal cavity. How and why does it happen?
Baby has a stomach ache
Why do lymph nodes become inflamed?
Lymph glands, also called lymph nodes, are present throughout the body. They are part of the immune system. During an infection, the lymph nodes will become enlarged and painful as the body fights bacteria and viruses. After the body clears the infection, the lymph glands return to normal.
Important! With mesadenitis, the lymph nodes in the membrane (mesentery) that surrounds the large intestine and loops of the small intestine become inflamed and connects them to the abdominal wall. This usually occurs with intestinal infections, less often with other infections.
Mesadenitis in infants is rare; it is more often diagnosed in children over 2 years of age, but such cases do occur.
The concept of mesadenitis
Bend gallbladder in a child - causes
The mesentery, in addition to attaching the intestines to the abdominal wall, performs a number of other functions. Here are blood vessels, neuroreceptors and lymph glands.
Important! Due to the complex structure and importance of the functions assigned to it, many pathologies in the abdominal cavity arise precisely in the mesentery. One of them is mesenteric lymphadenitis (another name is mesadenitis).
Symptoms of mesenteric lymphadenitis can appear over several days, less often weeks (chronic form). These include:
- abdominal pain, often in the lower right corner;
- enlarged lymph nodes;
- temperature increase;
- general weakness;
- increased breathing and heart rate.
Sometimes nausea and vomiting and loose stools are observed.
Factors contributing to inflammation
Constipation in a 5 month old baby - causes and what to do
The main cause of inflammation of the lymph nodes in the intestines of a child is the penetration of infections.
Opportunistic microorganisms that live in the intestinal flora (staphylococci, streptococci) can also be direct pathogens.
When their number exceeds the norm due to the development of infectious diseases and insufficient immunity, opportunistic microorganisms can cause intestinal dysfunction and inflame the lymph nodes of the abdominal wall.
Lymph nodes of the mesentery
Infectious diseases that can cause inflammation of the lymph nodes in a child’s intestines:
- gastroenteritis;
- intestinal infections;
- pneumonia;
- otitis;
- pyelonephritis;
- tonsillitis;
- respiratory infections;
- vaginitis;
- cystitis.
Types of mesenteric lymphadenitis
A child has a rash on his hands - what is it, the causes of the rash
If the mesenteric lymph nodes are enlarged in a child, this may mean that there was a primary pathology, and mesadenitis is secondary. However, its course is not always the same.
There is an acute form of the disease, characterized by much more severe symptoms (primarily sharp, cramping abdominal pain). The chronic course of mesadenitis is longer, but also less painful for the patient.
Experts divide the disease into several varieties, determined by the pathogen:
- Non-specific. It is provoked by E. coli, staphylococci and other pathogens. Occurs with reduced immunity and can be purulent and simple;
- Specific. Caused by the influence of the tuberculosis bacillus (tuberculosis), the bacterium Yersinia enterocolitica (yersinia) and Yersinia pseudotuberculosis (pseudotuberculosis).
There are also types of mesadenitis, determined by the way the infection penetrates the lymph nodes: through the gastrointestinal tract or carried by blood and lymph.
Diagnostic methods
When there is a suspicion that the lymph nodes in a child’s stomach may become inflamed, various diagnostic methods are used.
To make a diagnosis, the doctor will most likely:
- Collect information about the child's medical history. In addition to information about current symptoms, information about previous illnesses, the baby’s diet, trips and illnesses of relatives will be needed;
- Will palpate the baby’s abdomen to detect the presence of swelling, feel that the lymph glands of the mesentery have increased in size;
Palpation of the abdomen
- Refer the patient for laboratory tests. You will need a blood test (biochemical and general) that can help identify the presence of an infection in the baby and its type. In some cases, stool and urine tests will be required;
- If necessary, a visual test will be prescribed. Since the mesenteric lymph nodes are not accessible for viewing, special diagnostic methods are needed, such as abdominal ultrasound and computed tomography.
Important! First of all, mesadenitis must be differentiated from Crohn's disease and appendicitis.
Ultrasound of the abdominal cavity of a baby
Which doctor treats mesadenitis
Treatment of mesenteric adenitis is carried out by a gastroenterologist or therapist, in children - by a pediatrician and usually depends on the cause of the problem.
Therapy methods
There is no special treatment for mesadenitis; this is not always necessary.
Important! It is necessary to treat the root cause of inflammation of the mesenteric lymph nodes, that is, bacterial and viral infections.
Treatment methods are mainly symptomatic. Uncomplicated cases of mesadenitis and diseases caused by a virus usually go away within a few days or weeks.
Medicines used in treatment may include:
- Painkillers and antipyretics (except aspirin, as it increases the risk of Rayet syndrome in children);
- Antibiotics are prescribed for moderate to severe bacterial infections;
- Medicines needed to boost immunity, vitamins, antihistamines.
In complicated cases, hospital treatment will be required.
At home you need to do the following:
- Get plenty of rest. This will help the child recover;
Baby resting
- To relieve pain, place a warm, damp cloth on your stomach;
- If diarrhea and vomiting occur, you should drink water in small sips at short intervals. The baby can be given a teaspoon of it every 10 minutes.
Children's doctor E. Komarovsky says that the best way to prevent inflammation of the mesenteric lymph nodes is to take preventive measures against infections that can provoke mesadenitis.
If enlargement of the lymph nodes does occur, then in most cases the swelling regresses even without special therapy, as the primary disease is treated.
However, only a doctor can determine whether it is dangerous or not, therefore, when a baby has signs of mesadenitis, he should be observed by a pediatrician.
Nutrition for mesadenitis
During mesenteric lymphadenitis, the baby must adhere to a special diet:
- Meals should be more frequent and portions small;
- It is advisable to exclude whole milk and dishes made from it. Fermented milk products can be consumed;
- When a child receives complementary foods, it is necessary to cook only by steaming, boiling foods in water or baking in the oven;
- Meat and fish should be with a minimum amount of fat, the use of butter is also limited;
- You need to make jelly and compotes from fruits and berries, and not eat them fresh;
- Porridge can be cooked from oatmeal, buckwheat or rice. In this case, it is better to cook them initially in water, adding a small amount of milk only at the end of cooking;
Baby is fed porridge
- It is good to give your baby rosehip decoction and medicinal chamomile tea.
Foods that should not be consumed
Prohibited use:
- whole milk;
- fatty foods;
- boiled and fried eggs (only soft-boiled eggs are allowed);
- fresh fruits and vegetables;
- fresh bread and pastries;
- sweets, maybe just a little honey.
The main thing for parents
If an infant experiences abdominal pain, parents should prepare for a visit to the doctor to speed up the diagnosis and increase the likelihood of it being correct.
What information does the doctor need:
- A description of all symptoms of illness and when they began. It is advisable to measure the temperature several times and record the results;
- Information about vaccinations performed and diseases suffered;
- The names of all medications that the child takes, their doses;
- Events preceding the onset of pain.
If necessary, the doctor will conduct additional tests. The baby needs constant monitoring by the parents until an accurate diagnosis is made and appropriate treatment is carried out.
Source: https://kpoxa.info/zdorovie-pitanie/limfouzly-kishechnike-rebenka-prichiny.html
Tuberculous mesadenitis
According to medical statistics, enlarged lymph nodes in the peritoneum are more often observed in children aged 6-14 years. In view of this, the occurrence of such a condition due to infection with Koch bacilli (tuberculosis form) is diagnosed in rare cases. It occurs due to the fact that pathogenic bacilli from the lungs enter the lymph, and with it are carried into the lymph nodes of the peritoneum. In this case, the following signs of inflammation are observed:
- The child becomes indifferent to games and lethargic.
- Lost appetite.
- There is weight loss.
- I am worried about a cough that cannot be treated with classical methods.
- The skin becomes pale.
- The temperature stays between 37.1-37.3 degrees Celsius.
If the lymph nodes in the child’s abdominal cavity are enlarged precisely because of suspected tuberculosis, what should be done? First of all, you need to perform a test for the presence of Koch bacilli in the blood. It is better known as the Mantoux reaction.

Nowadays, you can catch tuberculosis anywhere - in transport, in child care institutions, during public events. At risk are children whose family members suffer from this disease, as well as those children who have undergone any disease or surgery after which their immunity has decreased. Parents of such children should immediately consult a doctor if the child develops the above symptoms.
Decoding the research results
The protocol is interpreted by a doctor. The doctor compares the ultrasound data with the age standards of the lymph nodes. They must be distinguished by a homogeneous structure, retain their specific shape, mobility, have an evenly outlined light contour and a uniformly colored dark surface.
The normal size of lymph nodes depends on their location. In children, the size of the mesenteric structures reaches 3.5 cm, and in other groups it does not exceed 1.5 cm. Superficial nodes within 4 mm - 1 cm are elastic or cannot be felt on palpation.
What does an ultrasound of the lymph node(s) show in children:
- infectious disease - enlargement of nodes without inflammation near the pathological focus (on the neck, under the jaw, on the arm, in the groin, other places);
- hyperplasia - the node grows while maintaining the structure, the pathology is confused with signs of an infectious disease;
- lymphadenitis - the node enlarges, inflammation manifests itself as hypoechogenicity (darkening of areas);
- mesadenitis - inflamed mesenteric (mesenteric) nodes, an increase of more than 1 cm from normal, adhesions with surrounding tissues;
- metastasis, malignant tumor - a node is round, irregular in shape, heterogeneous, with black and white inclusions, a developed network of vessels;
- Hodgkin's lymphoma - a node with smooth borders and shadows;
- lymphoma - no clear boundaries, with a heterogeneous (heterogeneous) structure;
- purulent lymphadenitis - a round dark or heterogeneous spot with an unclear border;
- lymphogranulomatosis and latent cancer - an enlarged node does not hurt and does not decrease during treatment.
The accuracy of ultrasound results depends on the correct preparation, experience of the ultrasound specialist and the attending physician. There may be errors in deciphering the protocol, since similar ultrasound signs appear in different diseases. To clarify the diagnosis, children may be prescribed blood tests, biopsy, x-rays, and other examination methods.
After illness, the lymph node shrinks to normal size within a few months.
What pathology looks like on ultrasound, watch the video:
The difference between mesadenitis and appendicitis, gastritis and other gastrointestinal diseases
Symptoms such as abdominal pain, nausea, loss of appetite, weakness, fatigue, stool upset (diarrhea/constipation) are observed in most diseases of the gastrointestinal tract. Therefore, it is almost impossible to make a diagnosis based on clinical manifestations alone. This is especially true if the patient is a small child who cannot really explain anything. The following characteristic signs can help in making a preliminary diagnosis:
- With gastritis, discomfort intensifies after eating. Also (in addition to the signs of mesadenitis listed above), patients may experience flatulence, heartburn, and belching. With inflammation of the lymph nodes, there are no such symptoms.
- With appendicitis, sharp pain is most often localized in the right side of the peritoneum (in the iliac region). Palpation of this area causes muscle tension and increased pain. Another sign is that the temperature in the rectal area differs from that measured in the armpit by 1 or more degrees. There are a number of syndromes by which an experienced doctor can distinguish appendicitis from inflammation of the lymph nodes.
- With shigellosis (dysentery), the symptoms are very similar to the manifestation of the acute form of mesadenitis. The difference is that in the first case, patients experience repeated diarrhea, accompanied by the appearance of mucus and blood in the stool.
Diagnostics
All parents should remember that it is necessary to immediately call an ambulance for their child if they experience:
- A sharp increase in temperature.
- Vomit.
- Complaints of abdominal pain.
- Diarrhea.
Self-medication in such cases is unacceptable, since drugs “for diarrhea” or “for fever” can reduce or temporarily completely eliminate symptoms, which will affect the diagnosis. As a result, the child may die.
The doctor first conducts a clinical examination of the patient, performs palpation of the peritoneum, and various medical tests that help to exclude certain gastrointestinal diseases.
In a medical institution, the child is required to perform a number of tests:
- Total blood (determines the level of hemoglobin and leukocytes).
- Biochemical blood (detects the presence of hepatitis viruses and other pathogenic microorganisms).
- Total urine (shows the number of leukocytes in it).
- Coprogram (this analysis detects the presence/absence of blood in the stool).
- Mantoux test.
- Feces on worm eggs.
These studies help doctors rule out appendicitis, hepatitis, helminthiasis, and inflammation of the gastrointestinal tract in the patient.
The medical facility also checks how enlarged the child’s lymph nodes in the abdominal cavity are using an ultrasound. Additionally, specialists examine the liver, pancreas, kidneys, and bile ducts.
In cases where these studies do not provide an accurate picture of the patient’s condition, additional tests are performed:
- X-ray.
- Tomography (CT, MRI).
- Laparoscopy.
- Fibrogastroscopy.
Diagnosis of lymphadenitis
To establish the cause and type of lymphadenitis, a specialist needs to perform diagnostic procedures.
These include:
- Examination and interview of the patient, study of the anamnesis.
- General and biochemical blood tests.
- X-ray examination.
- Ultrasonography.
- Biopsy of an inflamed lymph node.

Ultrasound is used to identify the causes of inflammation of the lymph nodes
X-rays and ultrasound are used for abdominal and thoracic lymphadenitis, when it is not possible to determine their size and quantity during examination. A biopsy is used in rare cases and only when a specific type of disease is suspected.
Therapy methods
If a child has enlarged lymph nodes in the abdominal cavity, treatment can be carried out at home or in a hospital. This is determined by the doctor, depending on the severity of the pathological process. In some cases, all treatment consists of bed rest, eliminating the underlying disease (for example, influenza) and taking vitamins to strengthen the immune system. After recovery, all systems and organs gradually return to normal. This also applies to lymph nodes.

In other cases, drug therapy is carried out, which is primarily aimed at eliminating the causes of the pathology, that is, the underlying disease.
To relieve inflammatory processes in the lymph nodes, the following are prescribed:
- "Tempalgin".
- "Papaverine".
- "Drotaverine".
- "Ketorolac".
If inflammation of the lymph nodes is caused by intoxication, infusion solutions such as Neocompensan and its analogues are prescribed.
Children may also be prescribed physiotherapy, including compresses, mud applications, and ultraviolet radiation.
Both children and adults, when enlarged lymph nodes are detected, are required to be prescribed a diet (table No. 5). She excludes from the diet all foods that promote active digestion (spicy, spicy, salty, etc.), fresh bread, fried, smoked, hot seasonings.
Treatment of inflammation of the lymph nodes
The symptoms of pathology can be eliminated with the help of medications, traditional methods of treatment and physiotherapy.
Medicines
| Group name | Effect on lymphadenitis | Representatives |
| Antibacterial drugs | Antibiotics destroy the cell membrane of bacteria, which leads to their death. Used for bacterial infections. | Amoxiclav, Clindamycin, Azithromycin |
| Antiviral drugs | They inhibit the development of the virus by suppressing DNA replication or inhibiting neuraminidase. Used for viral lymphadenitis. | Amantandine, Remantandin, Tamiflu |
| Antifungal drugs | Drugs that increase the permeability of the fungal membrane, which prevents their reproduction and destroys the fungus from the inside. | Fluconazole, Amphotericin B |
| Antiseptics | Prevent the development of infection that occurs when the skin is injured. | Vishnevsky ointment, |
| Nonsteroidal anti-inflammatory drugs | Medicines that suppress the formation of prostaglandins and have a strong anti-inflammatory effect. | Ibuprofen, Ketorol, Nimesil |
| Antispasmodics | They are used for mesenteric lymphadenitis of viral, bacterial or tuberculous origin. Relieves pain. | No-Shpa, Drotaverine |
| Antihistamines | They constrict blood vessels at the site of inflammation, reduce capillary permeability, weaken and nullify the inflammatory process. | Cetirizine |
How to treat with folk remedies at home
If an accurate diagnosis has not been established and there are no medications at hand, you can use traditional methods of treatment. They include compresses and drinks made from vegetables, herbs and herbs, as well as echinacea tincture.
Uses of Echinacea
To get rid of lymphadenitis, a compress is made from echinacea - an effective remedy that resolves inflammation:
- 50 ml of tincture is mixed with 100 ml of water. The mixture is infused for half an hour.
- Gauze or a napkin is moistened with the solution and applied to the inflamed area.
- A small layer of cotton wool or soft cloth is laid on top.
- The compress is secured to the area with a bandage and held until it dries.

Compresses with echinacea tincture help get rid of lymphadenitis
Beet juice
Beetroot juice, obtained from the vegetable or its tops, has a strong cleansing effect and also improves the functioning of the lymphatic system.
To cure lymphadenitis, it should be consumed as follows:
- Extract juice from beets using a juicer. It is advisable to pre-cut it into pieces.
- Let the juice steep for half a day.
- Drink 100 ml of the drink on an empty stomach, morning and evening.

Beetroot juice is good for lymphadenitis
If the product is given to a child, the volume of juice should be reduced by half. It is also advisable to add a little carrot juice to make the drink more palatable.
Anti-inflammatory collection
Herbal infusions that relieve inflammation - you can use either ready-made pharmaceutical ones or mix the following ingredients yourself:
- peppermint;
- raspberry leaves and berries;
- dandelion root;
- Linden blossom;
- wormwood grass.
The components must be dried and mixed in equal proportions. 4 tbsp. l. the resulting collection is poured with 1 liter of boiling water, the infusion is allowed to brew for half a day, and then drunk half a glass 3-4 times a day.

Herbal tea helps relieve inflammation
Celandine compress
Celandine is an effective disinfectant and anti-inflammatory agent. To combat lymphadenitis, it can be applied to fresh leaves; they must be scalded with boiling water, cool slightly and applied to the affected area for 30-40 minutes.
A celandine compress is made as follows:
- 25 ml of celandine is diluted in 100 ml of water. The mixture is infused for half an hour.
- Gauze is soaked in the solution and applied to the lymph node.
- The compress is covered with cotton wool or a soft cloth, secured with a bandage and left for an hour.

Apply compresses with celandine to inflamed lymph nodes
Horsetail infusion
Horsetail is a blood purifier that improves the functioning of the lymphatic system.
An infusion of it is taken orally and prepared as follows:
- A tablespoon or 1 pharmaceutical bag of herbs is brewed in 250-300 ml of boiling water.
- The mixture is infused for 20-30 minutes, then filtered.
- Take 3 times a day, half an hour before meals.

Horsetail infusion improves the functioning of the lymphatic system
To enhance the effect, it is worth making a decoction of knotweed herb according to the same recipe. Taking infusions should be alternated at intervals of 2 days.
Physiotherapy
Physiotherapy is the use of physical factors on the body to treat a disease. The use of the method for lymphadenitis reduces inflammation, accelerates tissue regeneration, and also alleviates the patient’s general condition.
Physiotherapeutic methods used for inflammation of the lymph nodes:
- Ultra-high frequency or UHF therapy. It affects the body with a high-frequency electromagnetic field, increasing temperature and dilating blood vessels. This helps leukocytes quickly reach the site of inflammation, which speeds up recovery.
- Laser therapy. It affects the body's tissues with light waves, improving microcirculation, analgesically and relieving inflammation in the lymph node. Accelerates regeneration, helps with all types of lymphadenitis.
- Galvanization. It affects the body with a weak low-voltage electrical tone, relieving pain, restoring tissue and nerve fibers, stimulating microcirculation inside the lymph node.

Horsetail infusion improves the functioning of the lymphatic system
To enhance the effect, it is worth making a decoction of knotweed herb according to the same recipe. Taking infusions should be alternated at intervals of 2 days.
Physiotherapy
Physiotherapy is the use of physical factors on the body to treat a disease. The use of the method for lymphadenitis reduces inflammation, accelerates tissue regeneration, and also alleviates the patient’s general condition.
Physiotherapeutic methods used for inflammation of the lymph nodes:
- Ultra-high frequency or UHF therapy. It affects the body with a high-frequency electromagnetic field, increasing temperature and dilating blood vessels. This helps leukocytes quickly reach the site of inflammation, which speeds up recovery.
- Laser therapy. It affects the body's tissues with light waves, improving microcirculation, analgesically and relieving inflammation in the lymph node. Accelerates regeneration, helps with all types of lymphadenitis.
- Galvanization. It affects the body with a weak low-voltage electrical tone, relieving pain, restoring tissue and nerve fibers, stimulating microcirculation inside the lymph node.
UHF therapy accelerates the healing process
When using these methods, lymphadenitis goes away faster, but they cannot completely replace drug therapy. Physiotherapy should be used as an adjuvant and only under the supervision of a physician to avoid complications.
Complications
If you do not consult a doctor immediately as soon as the child begins to complain of abdominal pain, accompanied by vomiting, diarrhea and high fever, and instead self-medicate, then mesodenitis and lymphadenopathy, which are not considered life-threatening, can lead to serious complications:
- Suppuration of inflamed lymph nodes. In this case, the patient’s condition worsens significantly: abdominal pain intensifies, the temperature rises (up to 40 degrees), and symptoms of severe intoxication appear.
- Peritonitis (inflammation of the peritoneum).
- Localized mesadenitis develops into generalized (throughout the body).
- Sepsis. This is one of the most dangerous complications that occurs when pathogenic microorganisms enter the blood.
Mesadenitis - what is it?
Mesadenitis is an inflammation of the lymph nodes in the intestinal mesentery. Other names are mesenteric, or mesenteric, lymphadenitis.
The mesentery is a fold of peritoneum that supports the small intestine and attaches it to the wall of the abdomen. There are many lymph nodes here. Their task is to prevent an infection from spreading to other tissues and organs when an infection enters the body.

If the level of pathogenic agents (viruses, bacteria, tumor cells) is excessively high, then the immune system weakens. The result of this may be inflammation of the mesenteric lymph nodes.
Mesadenitis is most often diagnosed in childhood. The risk group consists of children with congenital immunodeficiency and weakened immunity.
The causes of mesadenitis in children are different. Mesenteric lymphadenitis can be an independent pathology or a complication of other diseases. Depending on this, primary and secondary mesadenitis are distinguished.
In the first case, inflammation occurs immediately in the mesenteric lymph nodes. It is often provoked by opportunistic microorganisms that become active only when immunity is reduced. The causative agents of primary mesadenitis can be:
- coli;
- Epstein-Barr virus;
- adenovirus;
- salmonella;
- enterovirus;
- cytomegalovirus.
Secondary mesenteric lymphadenitis occurs when infection is introduced into the mesenteric lymph nodes from other inflamed organs. This type of disease can develop against the background of pneumonia, appendicitis, tonsillitis, pyelonephritis, enteritis.
There are also two types of mesadenitis:
- Specific, or tuberculous, when the causative agent is Koch's bacillus.
- Nonspecific, caused by other microorganisms, often opportunistic. It can be purulent (with the formation of an abscess) and simple (without an abscess).
Mesadenitis can occur in chronic or acute form.
The child has enlarged lymph nodes in the abdominal cavity and spleen
In the human peritoneum, in its upper left part, there is a small organ called the spleen. In the fetus it is a hematopoietic organ. In the newborn baby and throughout the rest of a person’s life, the spleen performs many important functions, including lymphopoiesis. This means that lymphocytes and antibodies are produced in it. It also serves, like lymph nodes, as a natural filter that retains pathogenic agents (bacteria, viruses, foreign particles).
If a child has a stomach ache, ultrasound shows that the lymph nodes in the abdominal cavity and the spleen are enlarged - this is a sign that an inflammatory process is occurring in the body caused by infection with pathogenic microbes or protozoa.
However, an enlarged spleen can mean another unpleasant disease - lymphoma. It is diagnosed in people of any age, including children. Other names of the pathology are lymphogranulomatosis, Hodgkin's disease.
Its characteristic features are that in the first stages, enlarged lymph nodes practically do not manifest themselves at all and are discovered only by chance, for example, during an ultrasound of the abdominal cavity. They can spontaneously increase and decrease without causing any discomfort to the patient. As the disease progresses, symptoms such as fever, weight loss, refusal to eat, night sweats, and abdominal pain appear. Inflamed lymph nodes and the spleen stop performing their main function - protection against microbes. Therefore, people with this pathology have a sharply reduced immunity.
The cause of an enlarged spleen is the presence of the Epstein-Barr virus (herpes 4) in the blood. It is found in approximately 50% of children over 5 years of age, but not everyone gets lymphoma. Provoking factors include conditions that reduce immunity (diseases, surgeries, stress, poor nutrition) and genetic predisposition.

Treatment methods depend on the degree of development of the disease. In the early stages, antiviral therapy is prescribed using the drugs Valacyclovir, Ganciclovir and their analogues. If indicated, surgery may be performed to remove the spleen.
Symptoms of mesadenitis in children and its treatment
Clinical ophthalmology. Medical Review. Mesenteric lymphadenitis, mesenteritis - inflammation of the lymph nodes of the mesentery - is often the cause of acute abdominal pain syndrome in children. Diagnostic and therapeutic tactics for mesadenitis is a pressing interdisciplinary problem that is at the intersection of interests of pediatricians and pediatric surgeons.
Material and methods: a retrospective analysis of medical records of 65 children aged 1 year 6 months was carried out. Vladimir in - gg. Results of the study: the highest incidence of mesadenitis is in children of primary school age; the average age of patients was 10.5 years, which correlates with an increasing infectious load. The more pronounced the symptoms of the disease, the faster the patient comes to the attention of a specialist.
The absence of pathognomonic complaints and symptoms in acute mesadenitis, the polymorphism of the clinical picture, the relative rarity and non-specificity of changes in clinical and biochemical blood tests and a general urine test do not allow an accurate diagnosis to be made without the use of additional studies. To fully verify the diagnosis of acute mesadenitis, instrumental studies are used: ultrasound of the abdominal organs, retroperitoneal space and pelvis for differential diagnosis of the causes of abdominal pain and diagnostic laparoscopy for final verification of the diagnosis.
Serological studies are necessary to establish the etiology of mesadenitis and select complex treatment for the disease. It is advisable to expand the diagnostic search algorithm among viral infections that induce lymphoid proliferation. Key words: acute mesadenitis, children, onset of the disease, differential diagnosis, ultrasound examination, diagnostic laparoscopy.
Bardenikova 1, L. Shavlokhova 1, M. Shuvalov 2. Mesenteric lymphadenitis mesadenitis — a mesenteric lymph nodes inflammation — is the common cause of acute abdominal pain in children. Aim: to analyze the clinical picture impact of the disease onset on diagnostic verification terms of acute mesadenitis in children.
Vladimir in - underwent a retrospective analysis. Results: it was revealed that there was a high rate of mesadenitis incidence in children of primary school age average age was The more pronounced the disease symptoms, the faster the patient comes onto the radar of specialist. So, the following instrumental methods of examination are needed for a complete diagnostic verification of acute mesadenitis: abdominal cavity ultrasound, pelvic and retroperitoneum ultrasound for the differential diagnosis of the abdominal pain causes, and diagnostic laparoscopy for the final diagnostic verification.
Serological studies are necessary to establish the etiology of mesadenitis and the complex treatment tactics for the disease. Diagnostic search algorithm expansion among viral infections that ind uce lymphoid proliferation is also advisable.
Conclusion: acute mesadenitis is the interdisciplinary problem of pediatrics and pediatric surgery that requires skilled and consistent joint efforts aimed at accelerating the provision of specialty care to the child. Keywords: acute mesadenitis, children, disease onset, differential diagnostics, ultrasound, diagnostic laparoscopy. For citation: Bardenikova S.
Acute mesadenitis: pediatrician point of view. Medical Review. The article is devoted to the problem of acute mesadenitis in pediatrics, the results of an original study are presented. Mesadenitis, or mesenteric lymphadenitis, mesenteritis - inflammation of the lymph nodes of the mesentery - is often the cause of acute abdominal pain syndrome in children. Diagnosis and treatment of mesadenitis are at the intersection of interests of pediatricians and pediatric surgeons, which constantly maintains the relevance of this problem.
Difficulties in verifying the disease due to the lack of uniform diagnostic criteria do not allow us to estimate the true frequency of acute nonspecific mesadenitis, i.e.
The disease is diagnosed mainly in children aged 5 to 13 years [1, 2, 4, 7, 8], and boys are more often affected. The incidence of mesadenitis increases in the off-season, correlating with the epidemiology of ARVI [9]. In recent years, there has been an increase in incidence among both children and adults, however, perhaps this fact reflects an improvement in the diagnosis of mesadenitis [1, 9].
According to the current opinion in practical medicine, clinical examination using traditional routine methods does not allow establishing the correct diagnosis [3, 11]. The relatively high incidence of mesadenitis in children is associated with age-related anatomical and physiological characteristics of the digestive tract and intestinal lymphatic system. The mucous membrane of the small intestine in childhood is well developed, has a large number of villi, a developed network of blood and lymphatic capillaries of relatively large diameter, has increased permeability and high absorption capacity.
Lymphatic capillaries, starting from the top of the villi of the mucous membrane, branch, form broadly looped plexuses, increasing in diameter 10 times at the mesenteric edge of the intestine. Lymph is directed through the drainage vessels from the small intestine and the right half of the colon to the mesentery, and then into the venous bed. Lymphatic vessels are interrupted by mesenteric lymph nodes, located in four rows, their number increases with distance from the proximal small intestine, reaching an average of - With age, the histological structure, vascularization, innervation, number and size of mesenteric lymph nodes change: they become larger, more numerous, closely adjacent to each other.
By the age of 5-7 years of a child’s life, the maximum development of elements of lymphoid tissue in the body and in the mesentery in particular is observed, which is accompanied by an increase in the incidence of nonspecific mesadenitis.
At the age of 9-15 years, the number of lymph nodes decreases. The lymphatic system of the small intestine performs important functions in the body: conduction, lymphopoietic, barrier, fat and water are absorbed in it. The distal part of the ileum bears the greatest functional load, and therefore the passage of food masses in it slows down, stasis often occurs, which is also facilitated by the weak development of the ileocecal valve.
In case of intestinal diseases, favorable conditions are created for the return of chyme from the cecum and the absorption of toxic substances in the distal ileum. The regional lymph nodes, which perform a barrier function, take the aggressive blow. Thus, the development of mesadenitis is associated with the penetration of infection and toxins into the lymph nodes, and further spread of the inflammatory process to surrounding tissues, periadenitis with purulent melting of the node can become a source of local interintestinal abscess or diffuse peritonitis [1, 12].
At present, the etiology of mesadenitis is not fully understood, but the state of the body's immune reactivity reliably plays a significant role in its development.
Mesadenitis is not an independent disease - many diseases and reactive conditions that form secondary generalized or regional lymphadenopathy can become its clinical masks. Among them: infections - nonspecific viral, bacterial and specific tuberculosis, syphilis, tularemia, parasitic echinococcosis, alveococcosis, autoimmune ulcerative colitis, Crohn's disease and oncohematological diseases leukemia, Hodgkin and non-Hodgkin lymphomas, mesenteric lymphadenopathy of allergic, toxic and drug origin caused by intake om cephalosporins , penicillins, sulfonamides, atenolol, captopril and other drugs [13].
In the specialized literature, an opinion is expressed about the leading role of sensitization in the etiopathogenesis of the disease [2]. In practice, doctors more often encounter nonspecific mesadenitis, caused mainly by conditional pathogens that live in a healthy body and manifest their pathogenic properties when the immune defense is reduced [14, 15]. The causative agents of mesadenitis can be adenoviruses, enteroviruses, herpes viruses - cytomegalovirus [CMV] and Epstein-Barr virus [EBV], measles, rubella, parainfluenza viruses, Yersinia bacteria, salmonella, campylobacter, colibacillus and typhoid fever, tularemia, toxoplasma, chlamydia, staphylo- and streptococci [9, 10, 16].
Adenoviruses serotypes 1, 2, 3, 5 and enteroviruses of the Coxsackie group are considered the most common causative agents of mesadenitis. It should be noted that the replication of these viruses occurs slowly, there is a high ability to mutate, which slows down the immune response, and there is a long-term, often lifelong, persistence in the lymphoid tissues of the palatine tonsils, adenoids, and lymph nodes due to the integration of the viral genome with the genome of lymphoid cells and evasion from the system antiviral protection.
Thus, viruses and bacteria, entering the gastrointestinal tract from the upper respiratory tract with ingested mucus, multiply intensively in the small intestine, and when immune resistance decreases, the pathogenic microflora breaks into the regional lymph nodes. In addition to the enteral route, infection of the mesenteric lymph nodes from various primary foci of infection is possible through the lymphogenous route from the intestine, appendix, or hematogenous route from the respiratory system.
With a viral etiology of the disease, catarrhal phenomena in the nasopharynx, unilateral conjunctivitis at the start of adenoviral infection and systemic polyadenia are simultaneously observed [8]. Taking into account the most common etiological factors, it is obvious that the diagnosis of mesadenitis often begins with a pediatric consultation; It is of great importance not only to clarify complaints and examine a sick child, but also to interview parents regarding recent acute infections and known dispensary diseases.
It should be noted that with the formation of purulent mesadenitis, the intensity of pain decreases with a simultaneous increase in symptoms of intoxication; chronic inflammation in the lymph node is characterized by mild pain without a specific localization with increased dyspeptic disorders. Any abdominal pain raises suspicion of acute surgical pathology and requires an emergency examination of the patient by a pediatric surgeon to primarily exclude acute appendicitis [5-7, 11, 17-21]. The clinical picture of mesadenitis often resembles acute appendicitis, however, diagnostic difficulties are associated with the need for a differential diagnosis with a number of surgical cholecystitis, diverticulitis, torsion of the ovarian cyst, ovarian apoplexy, neoplasms, and therapeutic diseases pancreatitis, renal colic, colitis, exacerbation peptic ulcer of the stomach and duodenum, adnexitis, lymphogranulomatosis, accompanied by abdominal pain [5, 17, 18, 21].
Pain from mesadenitis, depending on the age of the child, can be localized near the navel or in the right iliac region, in the upper abdomen, or become diffuse.
Often the pain is moderate, dull, aching, almost constant, or, less commonly, cramping pain, which intensifies with changes in body position, movement, and coughing. Pain syndrome with mesadenitis, as a rule, increases more slowly, lasts a long time, without subsiding, unlike pain with appendicitis, for 3-7 days; very rarely spontaneously stops.
Considering the presence of predominantly central pain in mesadenitis, as well as the inability of children to detail their sensations, pediatric surgeons in practice very rarely evaluate these symptoms. It is important to know that the characteristic features of mesadenitis are increased gas formation in the intestines and the absence of local peritoneal signs [3, 7].
Palpation of enlarged lymph nodes in the area of the root of the mesentery with severe flatulence is very difficult, but in the presence of conglomerates of lymph nodes it can be informative. Bimanual examination (palpation of the abdomen with simultaneous rectal digital examination) is widely used in pediatric practice to assess the condition of the pelvic organs. However, according to leading experts, the cause of abdominal pain in half of the patients remains unclear after the initial examination [6, 18, 22].
It should be noted that in the differential diagnosis of abdominal pain, in children in particular, dynamic monitoring of the patient is very important. The differential diagnostic value of laboratory markers of inflammation: leukocytosis with neutrophilia or lymphocytosis, acceleration of ESR, increased levels of C-reactive protein is small [1, 3, 9, 10], since with mesadenitis the changes are nonspecific and can be observed in inflammatory processes of various localizations. The parameters of cellular and humoral immunity are studied when systemic or autoimmune diseases are suspected, but the methods are not readily available in routine clinical practice, the indicators are difficult to interpret without initial data, and the results are significantly delayed from an acute situation requiring prompt tactical decisions [1].
Thus, at the stage of differential diagnostic search for the causes of abdominal pain, the value of comparing the totality of clinical and laboratory data is high, but today the results of non-invasive and invasive instrumental methods are the main ones in diagnosis [1, 3].
With mesadenitis, single or multiple mesenteric lymph nodes are visualized, 2-3 large with adjacent numerous small ones, often in the form of a conglomerate, increased in diameter due to inflammatory edema depending on the age of the child up to 25-28 mm, irregularly rounded in shape with smooth, clear contours , with reduced echogenicity of the cortical layer and increased echogenicity of the medulla. Doppler examination reveals increased vascularization in inflamed lymph nodes. There is increased pneumatization and increased peristalsis of the small intestine with thickening of its wall and swelling of the mesentery [4].
Severe flatulence, especially when a patient is hospitalized for emergency reasons, complicates visualization and reduces the information content of ultrasound. Diagnostic capabilities can be expanded using magnetic resonance imaging (MRI) with 3-dimensional modeling, which has high resolution.
The study allows us to obtain complete information with absolute certainty about the location, size, number and structure of the affected lymph nodes, as well as the condition of the adjacent organs of the retroperitoneum and pelvis [1, 17, 21].
Diagnostic laparoscopy, performed under general anesthesia, is recognized today as the most accurate method for differential diagnosis of the causes of abdominal pain, including. The laparoscopic picture of acute mesadenitis is usually represented by enlarged lymph nodes of dense consistency, hyperemic, located in a conglomerate in close proximity to the primary source of inflammation; the mesentery of the small intestine is swollen, hyperemic and infiltrated.
During diagnostic laparoscopy, a thorough examination of the abdominal cavity is carried out; at the same time, intraoperative biopsy and rapid cytological examination of the lymph node, abdominal effusion, enzyme-linked immunosorbent assay [ELISA], and bacteriological culture are possible.
The histological picture in the changed mesenteric lymph nodes corresponds to acute inflammation: swelling of the capsule, intense proliferation of lymphocytes in the cortex, in the medulla - disruption of the structure of the strands with diffuse cellular infiltration of lymphocytes and macrophages, the reaction of immunocompetent cells to the infectious process [1, 2]. However, it is important to understand that excluding acute surgical pathology, leading to early discharge home, in the absence of clarity of the etiology of the disease and, accordingly, without adequate therapy, is fraught with the development of complications, relapses of the disease, and therefore repeated hospitalizations [9].
Treatment of acute nonspecific mesadenitis, as a rule, is conservative and is carried out in a surgical hospital. The patient is recommended [1, 22] to limit physical activity with bed rest until complete recovery, drink plenty of fluids and eat sparingly.
Knowledge of the etiology of the disease provides significant assistance in choosing treatment tactics: antibacterial drugs, antiviral agents and immunostimulants are prescribed, painkillers, antispasmodics, and detoxification therapy are administered. Physiotherapeutic procedures are widely used - magnetic therapy, UHF. The basis of prevention is a healthy lifestyle, strengthening the immune system, identifying and treating chronic foci of inflammation, which can serve as a source of development of mesadenitis.
Children who underwent appendectomy and were diagnosed with concomitant nonspecific mesadenitis during a diagnostic examination were excluded from the analysis. There was a tendency towards an increase in the incidence of mesadenitis in children in the off-season and warm season (Fig. The reason for seeking medical help and referral to a surgical hospital for all children was abdominal pain. However, the urgency of hospitalization did not correlate with the child’s age and largely depended on the attention and anxiety of the patient’s parents.
Upon receipt of rice. All children complained of abdominal pain.